CHAPTER 24 - Nursing Pharmacology
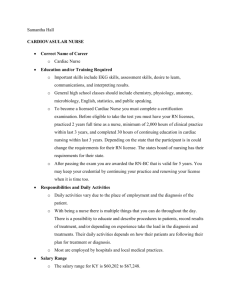
advertisement

CHAPTER 24 DRUGS FOR HEART FAILURE LEARNING OUTCOME 1 Identify the major diseases that accelerate the progression of heart failure. Concepts Heart failure (HF) is defined as the inability of the ventricles to pump enough blood to meet the body’s metabolic demands. Weakening of the heart muscle occurs with aging; however, the following diseases may cause or accelerate HF: mitral stenosis, myocardial infarction (MI), chronic hypertension (HTN), coronary artery disease (CAD), and diabetes mellitus. There is no cure, only prevention and slowing the progression of HF. LEARNING OUTCOME 2 Relate how the symptoms associated with heart failure may be caused by weakened heart muscle and diminished cardiac output. Concepts 1. In left-sided HF, excess blood accumulates in the left ventricle, causing it to thicken and enlarge (hypertrophy) in order to compensate for the increased workload. Blood eventually backs up into the lungs, resulting in the classic symptoms of cough and shortness of breath. 2. In right-sided HF, excess blood backs up into veins, resulting in peripheral edema and engorgement of organs, such as the liver. Right-sided heart failure is less common than left-sided HF. Figure 24.1 The pathophysiology of HF LEARNING OUTCOME 3 Explain how preload and afterload affect cardiac function. Concepts 1. Cardiac output is affected by preload; that is, the degree to which the myocardial fibers in the heart are stretched prior to contraction. This occurs just before the chambers of the heart contract as they are filling to their maximum capacity with blood. 2. Cardiac output is also affected by afterload, or the degree of pressure in the aorta that must be overcome for blood to be ejected from the left ventricle. Adams_IRM Ch 24-1 LEARNING OUTCOME 4 Describe the nurse’s role in the pharmacologic management of heart failure. Concepts 1. The role of the nurse is to obtain a complete health history, including allergies, drug history, and possible drug interactions. Assess vital signs, urinary output, and cardiac output, initially and throughout therapy. Drugs are used to treat the symptoms of HF by mechanisms such as slowing the heart rate, increasing contractility, and reducing the heart’s workload. 2. The nurse’s role in the pharmacological management of HF with ACE-inhibitor therapy includes monitoring the CBC, since these drugs can cause neutropenia; assessing for severe hypotension (especially with initial doses); and using with caution in patients who have impaired kidney function, hyperkalemia, and autoimmune diseases. Patient teaching should include notifying the patient that it may take weeks or months for the maximum therapeutic response, noting sodium and potassium restrictions, and cautioning patient to not take any other medications, OTCs, herbals, or vitamins without notifying the prescriber. 3. The nurse’s role in diuretic therapy for HF includes assessing renal function, because these drugs are contraindicated for kidney diseases, and monitoring electrolyte levels and for weakness, hypotension, and confusion. Additionally, the nurse should monitor vital signs, intake and output, and blood glucose and blood-urea nitrogen (BUN). Patient teaching includes instructing patients to monitor their sodium intake in order to not exceed 4,000 mg daily; to report a weight loss of more than two pounds per week and any fatigue or muscle cramping; and to change position slowly to avoid dizziness. 4. The nurse’s role in beta-adrenergic blockers (antagonists) includes monitoring for worsening of symptoms, hepatic toxicity, and liver function. These drugs are contraindicated in patients with chronic obstructive pulmonary disease (COPD), bradycardia, heart block, and decompensated heart failure. Patient teaching should include monitoring for blood pressure and pulse (notify health care provider if the pulse is below 50 beats/minute); reporting signs and symptoms of worsening HF, such as shortness of breath, edema, and chest pain; and being warned to not stop taking the drug without notifying the prescriber. 5. The nurse’s roles in cardiac glycoside therapy includes evaluating the patient for ventricular dysrhythmias not associated with HF and assessing renal function, since this drug is excreted by the kidneys. Monitor for drug interactions, and do not give the medication within two hours of giving antidiarrheal medications or antacids, because this decreases the absorption of digoxin. Patient teaching includes having lab tests to monitor therapeutic range, knowing the signs and symptoms of toxicity (nausea, vomiting, anorexia, and visual disturbances), and counting the pulse for one full minute and notifying the prescriber if the pulse is below 60 or above 100. The patient should report a weight gain of two or more pounds per day and should eat foods high in potassium. 6. The nurse’s role in phosphodiesterase inhibitors and other inotropic agents involves assessment of potassium levels for hypokalemia, monitoring for hypotension, and assessing for renal impairment and dysrhythmias. If given an IV, the patient should be continuously monitored for ventricular dysrhythmias, such as premature ventricular contractions (PVCs), ectopic beats, ventricular tachycardia, and fibrillation. Patient teaching includes ensuring the patient immediately reports irregular or rapid heart rate, a fever of 101 degrees or higher, or an increase in chest pain. If given an IV, the patient should be monitored for a fever of 101 degrees or higher or pain or swelling at the infusion site. Ch 24-2 Adams_IRM LEARNING OUTCOME 5 For each of the drug classes listed in Drugs at a Glance, know representative drug examples and explain their mechanisms of action, primary actions, and important adverse effects. Concepts 1. ACE inhibitors: The prototype drug is lisinopril (Prinivil, Zestril). The mechanism of action is to reduce the afterload on the heart and lower blood pressure by enhancing the excretion of sodium and water, which lowers peripheral resistance and reduces blood volume. These are drugs of choice for HF. The primary use is to lower the blood pressure and the risk of heart failure. Important adverse reactions include first-dose hypotension, cough, hyperkalemia, and renal failure. 2. Diuretics: The prototype drug is furosemide (Lasix). The mechanism of action increases urine flow, which reduces blood volume and cardiac workload and also reduces edema and pulmonary congestion. The primary uses are to reduce blood pressure, reduce blood volume, and reduce the workload of the heart. Important adverse reactions include dehydration, electrolyte imbalances, hypotension, and ototoxicity. 3. Beta-adrenergic blocker: The prototype drug is carvedilol (Coreg). The mechanism of action works by slowing the heart and reducing blood pressure, which reduces the workload of the heart by exhibiting a negative inotropic effect. The primary use is to reduce symptoms of heart failure and slow the progression of the disease. Important adverse reactions include fluid retention and worsening of HF, fatigue, hypotension, bradycardia, and heart block. 4. Vasodilators: The prototype drug: isosorbide dinitrate (Isordil). The mechanism of action is to directly relax blood vessels. The primary use is to lower the blood pressure. These drugs are usually only used for patients who cannot take ACE inhibitors. Important adverse reactions include reflex tachycardia and orthostatic hypotension. 5. Cardiac glycosides: The prototype drug is digoxin (Lanoxin). The mechanism of action is to cause the heart to beat more forcefully and more slowly, which improves cardiac output. The primary use is to increase the contractility or strength of myocardial contraction. These drugs are now considered second-line treatment for heart failure. Adverse effects include neutropenia, dysrhythmias, and digitalis toxicity. 6. Phosphodiesterase inhibitors and other inotropic agents: The prototype drug is milrinone (Primacor). The mechanism of action is to block the enzyme phosphodiesterase in cardiac and smooth muscle, which increases the amount of calcium available for myocardial contraction. This causes a positive inotropic response and vasodilation, thus increasing cardiac output by increasing the contractility and decreasing afterload. These drugs are usually only used for very short periods of time—2 to 3 days—when ACE inhibitors are not effective. The primary use is for short-term treatment of heart failure. Important adverse reactions are hypokalemia, hypotension, and ventricular dysrhythmias. Table 24.1 Drugs for Heart Failure Prototype Drug lisinopril (Prinivil, Zestril) furosemide (Lasix) digoxin (Lanoxin) metoprolol (Lopressor) Adams_IRM Ch 24-3 milrinone (Primacor) LEARNING OUTCOME 6 Use the nursing process to care for patients who are receiving drug therapy for heart failure. Concepts 1. Assessment of the patient who is receiving drug therapy for heart failure should include obtaining a complete health history (including allergies and drug history for possible interactions); assessing vital signs, urinary output, and cardiac output; determining the reason the medication is being administered; and assessing the patient’s knowledge of the disease process. 2. Nursing diagnoses: Possible nursing diagnoses would include Ineffective Tissue Perfusion, related to impaired cardiac status; Decreased Cardiac Output; Excess Fluid Volume; and Deficient Knowledge, related to drug regimen and disease process. 3. Planning: Patient goals and expected outcomes for the patient receiving drug therapy for heart failure include the patient’s reporting decreased symptoms of cardiac decompensation related to fluid overload, exhibiting signs of improved organ perfusion, demonstrating an understanding of the drug regimen, and immediately reporting important side effects. 4. Implementation: Interventions that the nurse may implement include monitoring the patient’s ECG, observing for drug side effects, weighing the patient for drug effectiveness or signs of fluid overload, monitoring serum-drug levels of medication and for signs of drug toxicity, and monitoring electrolyte levels. 5. Evaluation of the effectiveness of drug therapy is evidenced by patient goals and outcomes being met. Ch 24-4 Adams_IRM