6 Optimization Strategies for Client Education and
advertisement
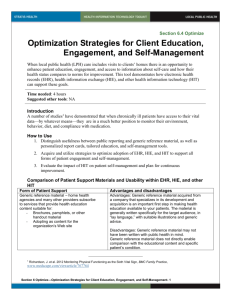
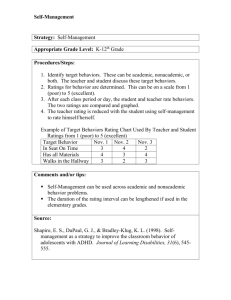
Section 6.6 Optimize Optimization Strategies for Client Education and Report Cards This tool describes how electronic health records (EHR), health information exchange (HIE), and health information technology (HIT) can support enhanced patient education; patient access to their vital data, including the ability to compare their status with normative data; and their ability to become more engaged patient in self-management. Time needed: 4 hours Suggested other tools: NA Introduction A number of studies1 have demonstrated that when chronically ill patients have access to their vital data they are in a much better position to monitor their environment, behavior, diet, and compliance with medication. Researchers have observed2 that medical outcomes and quality of life improve, and patients feel more in control of their own health, and have suggested identifying ways to ensure that patients who want access to their EHR obtain information on health data that is most relevant for them. Home care affords an important opportunity for enhanced patient education, engagement, and access to information about clients’ own care, as well as information about how their health status compares to norms for improvement. How to Use 1. Distinguish between public reporting and generic reference material, as well as personalized report cards, tailored education, and self-management tools. 2. Acquire and utilize strategies to optimize adoption of EHR, HIE, and HIT to support all forms of patient engagement and self-management. 3. Evaluate the impact of HIT on patient self-management and plan for continuous improvement. Comparison of Patient Support Materials and Usability within EHR, HIE, and other HIT Form of Patient Support Advantages and disadvantages Generic reference material. Home health agencies and many other providers subscribe to services that provide health education content suitable for: - Brochures, pamphlets, or other handout material - Content for the organization’s Web site Generic reference material acquired from a company that specializes in its development and acquisition is an important first step in making health education available to your patients. The material is generally written for the target audience, in “lay language” with suitable illustrations and generic advice. Generic reference material may not have been written 1 Richardson, J. et al. 2012 Monitoring Physical Functioning as the Sixth Vital Sign, BMC Family Practice, www.medscape.com/viewarticle/767764 2 Cimino, et al. 2001 cited in M. Pieper and K. Stroetmann, Universal Access in Health Telematics, Berlin: Springer, 2005 Section 6 Optimize—Optimization Strategies for Client Education and Report Cards - 1 Form of Patient Support Customizable educational material is available as a utility in some EHR systems. - Some systems enable the professional user to select specific educational material and have it print with the patient’s name, photo, language, and even large font. - Some systems enable the professional user to combine educational material on multiple conditions for a single patient so one unique packet of information can be provided. - Some systems pre-populate educational material with patientspecific information, further customizing it to the specific patient. Public reporting of quality outcomes is designed to assist consumers in selecting the home health agency most suitable for their needs. Advantages and disadvantages with home health in mind. It does not directly enable comparison with the educational content and specific patient’s condition. When distributed by a home health professional, generic material may require more explanation than customizable material. Educational materials that are customizable through the EHR provide a closer bond between the material and the patient and provides specific guidance. The more patient information that can be incorporated, the more beneficial the materials. The home health professional can spend time focusing on specific messages rather than filling in patient-specific information missing from generic material. Although there is some evidence that public reporting is fulfilling its primary, consumer-based intent, there is also evidence that agencies are using public reporting to benchmark themselves, improve, and be more competitive. Both outcomes are positive. Results from public reporting will not necessarily translate directly to the results a given patient can expect. The reports tend to be far removed from the patient’s direct care activities. They may be available to patients via a Web browser or may be pushed to a patient’s personal health record (PHR) via a health information exchange organization (HIO). Patient-specific report cards and diaries (sometimes referred to as “participatory medicine”) are intended to motivate the patient to partner with the home health professional to improve health, take an active role in self-management, participate in decision-making about their care, and assume responsibility for making behavioral changes. See also an example of a portal to multiple sources for public data: http://reportcard.opa.ca.gov/rc2013/ Patient-specific report cards provide very specific, clear messages about the patient’s health status and can be generated by some EHRs, especially when linked to an HIO where multiple providers can contribute data (e.g., medications from pharmacy, lab results from lab or hospital, vital signs from home health agency). If the patient report card can be tailored to both the patient’s vital data and specific goals and used as a diary, it can be even more motivational. These are sometimes found in PHRs. Patient report cards may or may not include specific instructions for improvement. They must be explained to the patient and/or family in a supportive, partnering manner. These should not be introduced as “grades” in school. The home health professional must be skilled to Section 6 Optimize—Optimization Strategies for Client Education and Report Cards - 2 Form of Patient Support Advantages and disadvantages use them properly. Motivational interviewing See also: http://www.jopm.org/evidence/casestudies/2011/04/04/creating-a-participatory-officepractice-for-diabetes-care/attachment/shahady-table-1/ Motivational interviewing is a non-judgmental approach to increasing a patient’s awareness of the potential problems caused, consequences experienced, and risks faced as a result of a health-related behavior – especially those that contribute to chronic disease (e.g., diet, exercise) and behavioral disorders (e.g., drinking, isolation). Steps include involving patient in talking about issues and establishing rapport, focusing on specific things the patient wants to change, and allowing patient to plan the specific steps to implement the desired change so that the patient feels empowered to actuate the change. Shared decision-making tools allow patients and providers to make health care decisions together. Patient self-management/patient engagement tools often refer to technology used by a patient or informal caregiver to manage health problems outside formal institutions. See also: http://www.motivationalinterview.org/ This is a collaborative process that takes into account the best scientific evidence available, as well as the patient’s values and preferences. It honors both the provider’s knowledge and the patient’s right to be fully informed. It is most applicable to major clinical decisions patient face, such as whether to have a particular surgery. See also: http://www.informedmedicaldecisions.org/what-is-shareddecision-making/ Patient self-management/patient engagement tools include those accessible independently by a patient and those provided by a health care provider who also uses motivational interviewing and shared decisionmaking to help patients address barriers to achieving their health goals (e.g., lose weight, stop smoking). Some EHRs offer templates to build a patient’s selfmanagement plan of care. Patient education, diaries, and report cards are helpful adjuncts. Increasingly patient self-management is being linked to the broader scope of care coordination in the chronic care model. See also: http://www.chcf.org/~/media/MEDIA%20LIBRARY%20 Files/PDF/P/PDF%20PatientSelfManagementToolsOve rview.pdf http://informedmedicaldecisions.org/wpcontent/uploads/2012/04/Patient_Engagement_What_ Works_.3.pdf http://www.google.com/url?sa=t&rct=j&q=&esrc=s&frm =1&source=web&cd=4&ved=0CEkQFjAD&url=http%3A %2F%2Fwww.lphi.org%2FLPHIadmin%2Fuploads%2F Pt-Engage-Self-Mgt-Knox24859.ppt&ei=EXlxUsDNL8qQyAHWk4CYAg&usg=AF QjCNFsUt3qW7U12kKNVefKwvNDig4wQ&sig2=ahJt3bYrA23 Section 6 Optimize—Optimization Strategies for Client Education and Report Cards - 3 Form of Patient Support Advantages and disadvantages Y1n5mUrWxnA http://healthinsight.org/Internal/events/05-2312/megalan_talk.pdf Adoption and Evaluation of Patient Self-Management Results 1. Consider using a tool to plan and track how you aid patient education and self-management 2. At a minimum, list self-management techniques that your agency has or can readily acquire/develop. Provide staff training and encourage use of these techniques. (Some states have more state-based reporting than others. CMS Home Health Compare can be a starting point in the absence of more specific data available within a state. Each agency can also track its own data through EHR functionality or by contributing to a registry via a local or state HIO.) 3. Ideally, document the utilization of self-management techniques for each patient. (Techniques may need to be reinforced with discussions, and some techniques may need to be used repeatedly.) 4. Although it is unlikely that only one technique will cause improvement, it can be helpful to focus on a specific goal and document results. 5. Two examples are provided below. Add your own focus areas and techniques. SelfManagement Technique Report Card Date Initiated Baseline Data May 2 Uncontrolled diabetes; goal: Hg A1c = 8 in 3 months May 8 PHQ = 9 (Has fluctuated between 7 and 9) Diabetic diary PHR to receive lab results Depression Self-Care Action Plan Results after __ Time Aug 5: Hg A1c = 8.2 Jun 12 PHQ = 8 Specific Instructions to Patient -Use structured diabetic diary to record diet and blood sugars -Track Hg A1c values through PHR -Have patient develop a selfcare plan Copyright © 2013 Section 6 Optimize—Optimization Strategies for Client Education and Report Cards - 4 Results after __ Time Nov 3: Hg A1c = 7.4 Aug 14 PHQ = 7 Updated 11-20-13