Self-management after stroke
advertisement

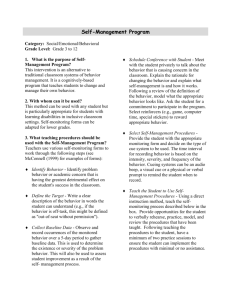
Dr Fiona Jones Principal Lecturer, Rehabilitation Now embedded in Health Policy ( DH 2008) Stroke- not only an acute condition- or a ‘one-off’ ( O’Neil 2008) Lack of specialist support long term (NSSA 2008) Goal setting principles align with selfmanagement theory, but there is inconsistency (Jones, 2006; Playford, 2009) Involves.... Problem solving Goal setting Self-discovery Utilising resources Knowledge about condition Shared decision making Collaboration Behaviour change By 2010, 15 million people will have personalised care plans, named lead professionals will ensure that plans and services are tailored to needs (Darzi, 2008; NHS Next Stage Review, July 2008) There will be a patients prospectus to provide advice for those people with LTC’s that want to take control of their health (NHS Next Stage Review, 2008) Rehabilitation and ongoing support should be designed around individual needs and goals Healthcare for London : Guidance for Commissioners (2010) Inpatient rehabilitation Early supported discharge Too medical? Too much going on Risks to high? Patient not ready Community rehabilitation Support structures after rehabilitation Team Goal setting method in place Support not available Limited time Limited understanding of rehabilitation Goals ..who is in control? When we don't agree with goals Use clinical reasoning to justify Framing goals around early rather than long term Collaboratively framing goal with other team members Goals are non-negotiable Never written down Playford et al., 2009 In-depth reflective case reports from professionals Experiences of using a selfmanagement programme Different stages of stroke pathway A new stroke self-management programme: preliminary analysis of training for practitioners International Journal of Stroke: 4: Supplement 2: December 2009 Timing when to use ‘Difficult to use in Intermediate care as timing is so short Lost impetus when transferred to day centre as the no-one took over supervision with workbook’ Unrealistic goals? ‘I worried the goal was too difficult and he had set himself high expectations But he did manage itI could have trusted him more!’ ◦ People with cognitive, perceptual and communication deficits ◦ Takes time which is limited in the acute setting ◦ Difficult when patients have limited motivation ◦ Too early in recovery – patients often still adjusting to what's happened to them/finding out what they have lost/kept ◦ Some difficulties in using the programme alongside traditional rehab ◦ Not easy when the whole team has not been trained ◦ Time pressures to “push through” patients ◦ Patient goals too ambitious Just giving it a go and getting some practice Knowing the content of the programme reasonably well Helped to involve family in rehab Using it flexibly e.g. with family, different sections Letting the patient set their own goals in own words Patient chooses an important goal to themselves Knowing other clinicians on stroke pathway are trained Incorporating self-management into daily practice Belief in the concept and commitment Confidence in the use of the workbook Yes ...but more limited in acute stage Yes.... if we do not try it then we will never know Helps with communication but dependent on existing relationships between services Therapists need to get together and discuss how the transition of care/self management concept is taken forwards. Puts client in charge of own pathway leads to continuity of care Aids continuity of care The same goals are aimed for by all clinicians and teams involved The patient could feel less vulnerable and more in control Helpful for transitional stages Help patient to focus on what they want to achieve at difficult stages of their journey Helps seamless transfer of goals Hardeman and Mitchie (2009) ‘in the absence of training healthcare professionals do not usually posses the knowledge and skills to deliver self-management interventions ‘(p102). Early supported discharge acute community Supporting individuals to: ◦ Make informed choices ◦ To assess their own needs and develop confidence to self-care ◦ Access appropriate information to manage needs ◦ Develop skills to self-care ◦ Use technology to support selfcare ◦ Access support networks, and participate in the planning and development of services ◦ Risk management and risk taking to maximise independence and choice Skills for Health & Skills for Care, 2008 Services need: Benchmarks of good practice Framework for staff development Develop new ways of working People focused services Emphasis on role of people in their own care Address personalisation agenda Boost confidence to ‘let go’ Reflective practice Research in partnership Patient’s and carer’s experiences Responsive CPD. Exemplars of best practice 13/04/2015 14 Measuring change : PROMs, Goal Attainment Scale, COPM The goal setting dilemma Self-management will mean risk Professional intransigence Translational research, multi-methods ‘Our plans to transform care for patients with long-term conditions will involve people being offered personalised care planning and support for self-care.’ NHS 2010–2015: from good to great preventative,peoplecentred,productive. ( DH, 2009) Self-management principles embedded into pathway Shared benchmarks of good practice Research programme in self-management ◦ Effectiveness, feasibility, acceptability, equity, efficiency Training and research in collaboration with service users ‘I read the book to begin with, and then I had another small stroke, I started looking at the workbook properly after that, I didn’t realise how fed up I was, looking in it regularly made me realise I can make some small steps to make progress in my life, and that those small steps could add up to giant steps’ f.jones@sgul.kingston.ac.uk www.bridges-stroke.org.uk