(台北) 91-10-12 胃腸內科 朱正心 醫師 健保(F3)
advertisement

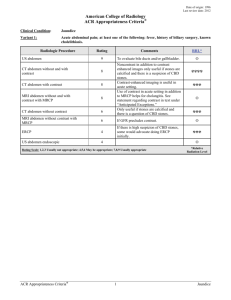
CC: skin itching sensation for 3 weeks PI: According to the previous chart record and the statement of this patient herself, we knew that this 49y/o female patient had colon cancer diagnosised and operated in 89/5. She took regular F/u and chemotherapy at our OPD. In 91/06 , liver metastasis was diagnosised by abdominal CT and TAE was done. Since 3 weeks ago, she sufferred from epigastric pain, loss of appetite ,vomiting ,insomia, and general malaise. Yellowish skin with itching sensation and tea color urine were noted.She visited our OPD for help and was suggested for admission. Physical examination finding:icteric sclera,yellowish skin,Abdemen: soft and no tenderness no ascites,no palpable liver or spleen, Due to the impression of 1.Malignant neoplasm of colon post OP and C/T ,with liver metastasis post TAE, 2.Jaundice, R/O obstuction of biliary tract, she was admitted to our ward for further evaluation and treatment. Dr Buttrey’s rewrite: Source of hx: patient, old chart [?family] CC 49 y/o female c/o pruritus for 3 weeks HPI: The patient was diagnosed with colon cancer in 89/5. [Stage?] She was subsequently treated with chemorx, including [agents?] resulting in [any response noted?] In 91/6, she was found on abdominal CT to have metastases to the liver, and she was treated with TAE with [response? Agent injected?]. Three weeks PTA, she noted the onset of epigastric pain [quality of the pain, any radiation?], loss of appetite, vomiting, insomnia, and general malaise. She also developed yellowish skin, generalized [Correct?] pruritus and tea colored urine. [At the same time as the other symptoms? Fever?] She was admitted from the OPD for further evaluation of possible biliary tract obstruction. Missing data: More details about her colon CA are needed: stage at dx, type of C/T given, response to C/T, side effects of C/T/ Was there any response to TAE? When was the last C/T given? What was the nature of the epigastric pain and did it radiate? Was there any fever? Weight loss? Why were these symptoms present for 3 weeks before she was admitted? How much does the patient herself understand about her disease? Comments Content: As this history is presented, it sounds most consistent with biliary tract obstruction, most likely secondary to liver metastases or possibly malignant lymph nodes in the porta hepatis. Benign obstruction by gall stones is less likely because of the apparent insidious onset of the symptoms, which were present for 3 weeks before the patient was admitted. However, the actual course of the symptoms and the reason she didn’t present for 3 weeks weren’t reported in the history, so I have to assume the course was insidious. It’s much better to give a reason rather than making the reader guess, since the guess could well be wrong! It’s important to note whether or not there was fever, because, whatever the cause of the obstruction, cholangitis is a possibility and would require antibiotic treatment. (Also, we’ll need to see if the patient is neutropenic. If so, the presence of fever would be important.) The epigastric pain may originate from the biliary tract and/or liver, but the presence or absence of radiation should also be noted. If the biliary obstruction is extrahepatic, could this woman have a low-grade pancreatitis accounting for some of her symptoms? More information about the cancer itself should be included, not because it would necessarily change the management at this point, but because it would help us better understand what she has been through, how her tumor has responded to therapy, and what issues are important to her and her family at this point in her life. Median survival after development of liver metastases varies somewhat from series to series and is also dependent on the presence of other metastases, etc. Therefore, giving a fuller description of her disease to this point is important. Most of this can be gleaned from the old chart. Because there are no details about the C/T or TAE, we don’t know whether we might expect any response to further treatment, whether she’s already had as much as should be given, whether she’d want more treatment, etc., etc., etc. The role of TAE for liver mets is still under investigation. There have been a number of small studies from Japan, suggesting favorable response in some patients, but its influence on survival is still unclear. We need to know if she appeared to have a good response to it or not. While we certainly will want to relieve her obstructive jaundice if possible, our concern for her as a person goes beyond that immediate problem to considering how we will continue to care for her through the final stages of her life. It would be wise to include some comment on how much she is aware of her condition. Is she to be included in discussions of prognosis, treatment, etc., or does the family want to handle all that themselves? English: skin itching sensation: “Itching sensation” is redundant. By definition, itching is a sensation. Use “itching” or “pruritus.” While we shouldn’t use technical medical terms when talking with patients, it’s fine to use them in the chart because they communicate clearly to other doctors. According to the previous chart record and the statement of this patient herself: While this is acceptable English, it’s long and a bother to write. I think it’s better to note the source of the history before even beginning it. An alternative is just to state the history, assuming that the patient is telling the story. Any other source can then be added at appropriate points, e.g., “The patient’s daughter said her mother’s eyes turned yellow….” “The old chart states that the tumor was Stage III at the time of surgery.” took regular F/u: Patients “have” F/U or “they are followed.” We don’t use “take” in this phrase. was suggested for admission: “…admission was suggested” or “she was admitted.” I prefer the latter. If she’s in the hospital, then she must have followed the suggestion! Don’t focus on the suggestion, just on what happened. The only exception would be if we suggested something and she refused. Then we should note both our recommendation and her reason for refusing. Due to the impression of: The list of diagnoses isn’t the reason she was admitted. Don’t bother relisting all the diagnoses. This wording is not used in English.