CASE-BASED REVIEW
Chronic Obstructive Pulmonary Disease
Exacerbations
Case Study and Commentary, Cynthia D. Brown, MD, and Neil R. MacIntyre, MD, FCCP
INTRODUCTION
hronic obstructive pulmonary disease (COPD) is the
fourth leading cause of death in the United States,
accounting for approximately 110,000 deaths per
year. COPD is a slowly progressive condition, with symptoms typically arising around age 50 to 60 years. As the U.S.
population of current and former smokers ages, the prevalence of this disease is expected to climb [1]. More than
16 million adults in the United States currently have the disease. COPD accounts for 16,367,000 office visits, 500,000
hospitalizations, and direct health care costs of $18 billion
annually [2].
The term COPD refers to a group of disorders characterized by permanent or minimally reversible expiratory airflow limitation, including chronic bronchitis and emphysema. Between 85% and 90% of all cases of COPD are caused
by smoking; other causative factors include genetic factors
(including alpha1-antitrypsin deficiency), passive smoking,
occupational exposures, air pollution, and, possibly, hyperresponsive airways. Patients with chronic bronchitis have
persistent airway inflammation that leads to dyspnea and a
productive cough. Chronic bronchitis is clinically defined as
the presence of a recurrent productive cough for 3 months of
the year in 2 consecutive years [3]. Emphysema is a destructive process that involves the lung parenchyma. In emphysema, the elastic fibers of the alveoli and distal air spaces that
provide the elastic recoil powering expiration are destroyed.
In both the chronic bronchitis and emphysema variants of
COPD, patients encounter a similar constellation of symptoms and a collection of derangements in respiratory function, including cough, sputum production, dyspnea, airflow
limitation, and impaired gas exchange.
A common feature of COPD is the development of episodes of acute worsening of airway function. Often termed
“flares” or acute exacerbations of COPD, these episodes are
major causes of morbidity and mortality in this disease process. In the natural history of COPD, exacerbations occur more
frequently as the disease progresses. In managing patients
with acute exacerbations, physicians must first exclude other
possible causes of the patient’s symptoms and then initiate
multi-agent therapy to provide relief of symptoms.
C
Vol. 7, No. 11
CASE STUDY
Initial Presentation
A 58-year-old man presents to his primary care
physician’s office with a complaint of increasing
shortness of breath and dyspnea on exertion as well as
wheezing and increased cough and sputum production,
progressing over a 1-week period.
History
The patient does not report experiencing fever, chills, night
sweats, weight loss, arthralgias or myalgias, or nausea or
vomiting. He has no chest pain or pressure, orthopnea, or
paroxysmal nocturnal dyspnea. His cough is more productive of sputum, but the sputum has not changed in quality.
Prior to the start of his symptoms, he visited with a friend
who had a cold. He does have rhinorrhea with clear drainage and nasal congestion.
The patient’s past medical history is significant for COPD
diagnosed 5 years ago and for hypertension. His baseline
oxygen saturation on room air measured by pulse oximetry
(SpO2) is 91%, and baseline forced expiratory volume in
1 second (FEV1) is 35% of predicted. He currently is taking
albuterol 2 puffs by metered dose inhaler (MDI) every
6 hours, ipratropium 2 puffs by MDI every 6 hours, and
hydrochlorothiazide 50 mg daily. He is not on chronic oxygen therapy. The patient smoked 1 pack of cigarettes per day
for 30 years but quit smoking 1 year ago. He is employed as
a telephone installer.
Physical Examination
The patient has a temperature of 100.8°F, pulse of 91 bpm,
respiratory rate of 22 breaths/min, and blood pressure of
146/73 mm Hg. Arterial oxygen saturation (SaO2) on room
air is 84%, increasing to 92% with 1 L of supplemental oxygen by nasal cannula. His throat is mildly erythematous, and
Cynthia D. Brown, MD, Fellow, Pulmonary and Critical Care Medicine,
Duke University Medical Center, Durham, NC; and Neil R. MacIntyre, MD,
FCCP, Professor, Pulmonary and Critical Care Medicine, Duke University
Medical Center.
JCOM November 2000 43
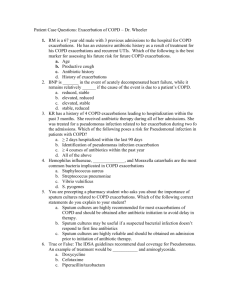
COPD EXACERBATIONS
Table 1. Winnipeg Criteria for Staging Acute Exacerbations
of COPD
Symptoms
Increased sputum purulence
Increased sputum volume
Increased dyspnea
Type of exacerbation
Type 1: All 3 symptoms present
Type 2: 2 symptoms present
Type 3: At least 1 symptom plus 1 of the following present:
Upper respiratory infection in the past 5 days
Fever without other apparent cause
Increased wheezing
Increased cough
Respiratory or heart rate increased 20% above baseline
accessory respiratory muscles are not being used. The patient experiences dyspnea only when speaking or walking.
The lung examination is significant for decreased breath
sounds throughout, with expiratory wheezing; fremitus and
percussion are normal. Cardiac examination reveals tachycardia, with normal rhythm and no murmurs or gallops.
There is no edema or clubbing of the extremities.
• What is the most likely cause of this patient’s symptoms?
• What evaluations are helpful in assessing a patient
with COPD exacerbation?
Clinical Criteria
As mentioned, COPD exacerbations characterized by worsening airways function occur in the natural history of the disease. Acute exacerbations are usually diagnosed on a clinical
basis. Although at present there are no established criteria to
define an exacerbation, most criteria used by clinicians
include some combination of 3 clinical findings: worsening of
dyspnea, increased sputum purulence, and increased sputum volume. The most accepted system for describing and
grading an exacerbation is the “Winnipeg criteria,” which
grades the severity of an exacerbation based on the number
of symptoms in a patient’s presentation [4] (Table 1). This
system was used to define the severity of exacerbations in a
trial of antibiotic therapy and is widely used in clinical
research.
Diagnostic Testing
Diagnoses to be considered in the setting of a COPD exacerbation include pneumonia, pneumothorax, congestive heart
44 JCOM November 2000
failure, and deep vein thrombosis/pulmonary embolus. A
number of laboratory assessments can be used to help rule
out these disease entities and to determine the severity of the
exacerbation (Table 2).
Chest Radiograph
The conditions most likely to present with a constellation of
symptoms similar to those found in an exacerbation are congestive heart failure and pneumonia, both of which can be
diagnosed from a chest radiograph. A chest radiograph
done during a COPD exacerbation typically does not demonstrate changes from a baseline radiograph done when the
patient is in stable condition. A retrospective study of chest
radiograph abnormalities in 97 patients with COPD exacerbation found that 17 (17%) patients had abnormalities on
radiograph, of which only 8 were significant (5 due to congestive heart failure and 3 due to pneumonia) [5]. The most
significant predictors of a radiograph abnormality were an
increased neutrophil count (> 8000/µL), history of congestive heart failure, and peripheral edema on physical examination. A second study that attempted to validate the predictors from the previous study found similar rates of
radiographic abnormalities (16%) but was unable to validate
the predictors with any statistical significance [6]. Both studies supported the use of a chest radiograph in evaluating
patients with COPD exacerbations, showing that a radiograph can eliminate congestive heart failure or pneumonia
as a cause of the symptoms and guide treatment.
Lung Function Tests
Spirometry showing reduced airflow is the key diagnostic
study employed in the initial diagnosis and staging of COPD
and subsequent monitoring of disease progression. Similarly, spirometry can be used during an acute exacerbation
to stage severity of the exacerbation. However, when performed during an exacerbation, spirometry has not been
shown to be helpful in making decisions regarding patient
care. Investigators measuring the relationship between FEV1
and arterial blood gas abnormalities in 70 patients with
acute exacerbations presenting to an emergency department
found a poor correlation between measured FEV1 and arterial PO2 (r = 0.47, P > 0.05) [7]; FEV1 showed a small but statistically significant correlation with pH (r = 0.36; P < 0.01).
Another study involving 199 patients with acute exacerbation showed a good correlation between PEFR and FEV1
(r = 0.84; P < 0.001) [8]; however, the difference in the measurements was greater than 10% in a small group of these
patients, suggesting that the 2 measurements are not interchangeable and making the clinical relevance of the study
findings uncertain. It must also be remembered that patients
in respiratory distress are usually unable to perform lung
function studies adequately.
Vol. 7, No. 11
CASE-BASED REVIEW
Table 2. Evaluation of Suspected COPD Exacerbation
Assessment
History
Sputum volume*
Sputum characteristics (purulence)*
Level of dyspnea*
Constitutional symptoms (fever and fatigue)
Changes in exercise tolerance
Exposure to infectious agents
Diagnostic studies
Chest radiograph
Complete blood count
Arterial blood gases
Gram stain/culture (when sputum present)
Spirometry
Others: ventilation/perfusion scans, ultrasound,
electrocardiogram, computed tomography
scan
Comment
Used to assess for pneumonia and congestive heart failure; also useful for diagnosis and
treatment
Used to assess for infectious causes
Used to measure level of severity, including new or worsening hypoxia or hypercarbia;
useful when deciding whether to admit patient and whether to institute assisted ventilation
Used for staging exacerbations; not useful for guiding therapy
Useful only when specific disease suspicion is high
*Components of the Winnipeg criteria.
Sputum Examination
Most exacerbations are believed to be due to tracheobronchial
infections. There is some controversy, however, regarding the
infectious agents involved and their actual role in the exacerbation. Sputum collected from patients with mild to moderately severe chronic bronchitis has grown many bacteria on
culture, including Haemophilus influenzae (22%), Pseudomonas
aeruginosa (15%), Streptococcus pneumoniae (10%), and Moraxella catarrhalis (9%) [9]. P. aeruginosa has been found more frequently in patients with exacerbations requiring intensive care
unit admission. The colonization of airways with nonpathogenic bacteria such as Haemophilus parainfluenzae accounted
for up to one third of all isolates. Investigators suggest that up
to 10% of all exacerbations are due to infection with Mycoplasma pneumoniae or Chlamydia pneumoniae [10–13]. There is
also evidence that viruses (notably rhinovirus) may play an
important role in the etiology of COPD exacerbations [13].
These studies suggest that sputum collection and Gram
stain/culture should be considered in the routine management of COPD exacerbations as they can aid in both specific
bacteriologic diagnosis and targeted antibacterial treatment.
Laboratory Testing and Diagnosis
A complete blood count reveals the following: white
blood cell (WBC) count, 6100 cells/mm3; hemoglobin, 10.6 g/dL; hematocrit, 32 mL/dL; platelets 263,000/mm3;
differential, 83% neutrophils, 7% lymphocytes, and 4% monocytes. Blood chemistries are significant for a BUN level of
Vol. 7, No. 11
17 mg/dL and a creatinine level of 1.0 mg/dL. FEV1 shows a
25% decrease from baseline. Chest radiograph shows bilateral hyperinflated lungs, flattened diaphragms, and no apparent infiltrate or consolidation. Arterial blood gas measurements are as follows: pH, 7.34; PCO2, 65 mm Hg; PO2,
52 mm Hg; SaO2, 84% on room air. Sputum Gram stain shows
gram-negative rods and many WBCs.
The physician makes a diagnosis of a moderately severe
COPD exacerbation as suggested by the presence of 3 Winnipeg criteria and decreased FEV1. She admits the patient to the
hospital because of worsening hypoxia and hypercarbia.
• When should patients with COPD exacerbation be
hospitalized?
COPD exacerbations can be treated in both the outpatient
and inpatient settings. The decision to admit a patient is usually based on clinical and laboratory criteria (Table 3). Treatment is aimed at decreasing symptoms and eradicating any
causes (ie, infectious agents) of the exacerbation.
• What is the approach to treatment of COPD exacerbations?
JCOM November 2000 45
COPD EXACERBATIONS
Table 3. Indications for Hospital Admission in Acute
Exacerbation of COPD
Poor response to outpatient management
Dyspnea that interferes with daily living (eating, walking)
High-risk comorbid conditions (pulmonary or nonpulmonary)
Altered mental status
New or worsening cor pulmonale
New or worsening hypercarbia/hypoxia
Adapted with permission from Standards for the diagnosis and care of
patients with chronic obstructive pulmonary disease. American
Thoracic Society. Am J Respir Crit Care Med 1995;152(5 Pt 2):S98.
The mainstays of therapy are bronchodilators, corticosteroids,
and antibiotics (Table 4). If the exacerbation progresses
despite adequate treatment, patients can develop respiratory
failure and hypoxia due to a combination of bronchoconstriction, collapse of airways during expiration, and air trapping.
Treatment for these conditions includes supplemental oxygen
and, traditionally, intubation and mechanical ventilation. Recently, noninvasive positive pressure ventilation (NPPV) increasingly has been used with success in this population.
Bronchodilating Agents
Bronchoconstriction caused by airway inflammation and
contraction of smooth muscle within the bronchial wall contributes to airflow obstruction and dyspnea in the COPD
patient with an acute exacerbation. Bronchodilators alleviate
this symptom by relaxing the smooth muscle and possibly
reducing inflammation. The 2 classes of bronchodilators currently available—β2 agonists and anticholinergics—bind to
their respective receptors on smooth muscle and inhibit contraction, thus preventing bronchoconstriction. The results of
randomized studies show that short-acting β2 agonists and
anticholinergic inhaled bronchodilators are equally effective,
and both are superior to parenterally administered bronchodilators, including methylxanthines and sympathomimetic agents, in the care of patients with acute exacerbations of COPD [14–18]. Patients may benefit from the
addition of a second bronchodilating agent once the maximal dose of the initial bronchodilator is reached [14,17].
These generalizations regarding use of bronchodilators are
limited by the small number of analyzable trials published,
substantial differences in inclusion and exclusion criteria
between them, and variability in the drug dosages that were
studied (many were substantially higher than the dosages
conventionally used) [18].
Corticosteroids
Several randomized controlled trials provide good evidence
that the use of systemic corticosteroids may be of benefit
46 JCOM November 2000
Table 4. Treatment for COPD Exacerbations
Bronchodilators
β2 agonists: 6 to 8 puffs by MDI every 1 to 2 hours OR 2.5 mg
inhaled solution by nebulizer every 1 to 2 hours
Ipratropium: 6 to 8 puffs by MDI every 3 to 4 hours OR 0.5 mg
inhaled solution by nebulizer every 3 to 4 hours
Corticosteroids
Methylprednisolone: 50 to 100 mg IV for first dose, then 40 to
60 mg every 6 to 8 hours; OR 40 to 60 mg orally once daily to
start
For both IV and oral regimens, taper as quickly as possible based
on clinical improvement
Antibiotics
Initial therapy is directed at most likely pathogen, and changes
are guided by results of sputum culture
Assisted ventilation
Utilization is guided by presence of new or worsening hypoxia or
hypercarbia
IV = intravenous; MDI = metered dose inhaler.
[19–24]. In the largest study to date, 271 patients were randomized to receive either intravenous and then oral corticosteroids or placebo [24]. A 10% reduction in treatment failures was seen in the population taking the glucocorticoid
compared with those taking placebo. The trial also showed
no difference in outcome between patients on an 8-week
and a 2-week drug-tapering regimen. Although the importance of treating with steroids has been studied, the optimal
dose and duration of treatment remains uncertain.
Antibiotics
Randomized, placebo-controlled studies and a recent metaanalysis of antibiotic treatment conclude that antibiotics are
beneficial in the treatment of patients with acute exacerbations of COPD [4,25–35]. Three of the trials stratified patients
by severity of disease [4,25,26]. Although they used different
severity scales, in each case patients with more severe exacerbations were more likely to experience benefit than those
less ill. This finding held up when studied in the context of
the meta-analysis [35]. Thus, the data support the use of
antibiotics in virtually all exacerbations of COPD. Antibiotic
therapy initially should be targeted toward suspected organisms and then adjusted according to sputum culture results.
Unfortunately, little evidence is available regarding the most
effective duration of a course of antibiotics. Typical administration periods range from 3 to 14 days.
Mucus Clearance
Data from randomized controlled trials involving 5 different
mucolytic drugs showed that mucolytic agents are ineffective
at shortening the course of patients with acute exacerbations
Vol. 7, No. 11
CASE-BASED REVIEW
of COPD, although it is possible that these agents may
improve symptoms [30,36–39]. Two trials of chest physiotherapy show that these strategies are ineffective in the treatment of patients with acute exacerbations of COPD [40,41].
Oxygen Therapy
The use of supplemental oxygen during COPD exacerbations
is beneficial in patients with hypoxemia (PO2 < 55 mm Hg).
Supplemental oxygen can alleviate vasoconstriction of pulmonary vasculature and improve oxygen delivery to tissues.
However, hypercarbia and respiratory failure can develop
when providing oxygen therapy to some hypoxemic patients. Mechanisms leading to these complications include
depression of respiratory drive, ventilation-perfusion mismatch, and the Haldane effect (ie, oxygenated erythrocytes
having a lower capacity for CO2 than deoxygenated erythrocytes). A study of proposed methods to identify patients at
high risk to develop hypercapnic respiratory failure during
supplemental oxygen therapy looked at 50 patients with
COPD exacerbations [42]. Thirteen (26%) patients developed
hypercarbia requiring mechanical ventilation. Arterial pH,
PO2, and PCO2 were not predictive of respiratory failure. To
date, no data have been published regarding the best method
for titration of oxygen following an acute exacerbation of
COPD. Based on data from the Nocturnal Oxygen Therapy
Trial (NOTT), it can be estimated that 20% of patients requiring oxygen during an exacerbation will not require oxygen
3 weeks after hospital discharge [43].
Assisted Ventilation
Acute respiratory failure can be defined as potentially lifethreatening hypoxia, hypercarbia, and respiratory acidosis.
Combinations of abnormal ventilation patterns, severe airway obstruction (due to bronchospasm and secretion immobilization), and pulmonary edema produce the pathophysiologic disturbances of ventilation-perfusion mismatch, air
trapping (intrinsic positive end-expiratory pressure [PEEP]),
and increased work of breathing. For persons with COPD,
this condition is considered “acute on chronic” respiratory
failure since the pathophysiologic changes occur in the context of chronic gas exchange abnormalities. Management of
acute respiratory failure is targeted at correcting the hypoxia, hypercarbia, and acidosis, while treating the cause of the
exacerbation. Bronchodilators and corticosteroids are still
the cornerstones of medical management.
Both traditional invasive mechanical ventilation and
NPPV address the mechanical disturbances of acute respiratory failure. Positive pressure during inspiration facilitates
ventilation by unloading ventilatory muscles; during expiration it reduces the breath initiation load imposed by intrinsic
PEEP. Supplemental oxygen is used to correct hypoxia. Traditional invasive mechanical ventilation, however, is associated
Vol. 7, No. 11
with more complications than NPPV, including nosocomial
and ventilator-associated pneumonias, barotraumas, and
hemodynamic changes such as decreased cardiac output
[44]. For patients with more severe COPD at baseline, weaning from the ventilator can also be a very difficult process.
NPPV has a lower complication rate than traditional mechanical ventilation [44], allows the concomitant use of conventional treatments (bronchodilators), and helps preserve patients’ nutrition and communication functioning.
In selected patients with acute exacerbations of COPD,
NPPV can decrease the need for mechanical ventilation and
improve survival. In 2 trials comparing NPPV with standard treatment, the need for intubation in the NPPV groups
was significantly lower: 26% versus 74% in a study involving
85 patients [45], and 9% versus 67% in a study involving
23 patients [46]. Other studies have found similar outcomes
[47,48]. A meta-analysis concluded that the risk of death was
lower in patients who were randomized to receive NPPV
(odds ratio [OR] = 0.22, 95% confidence interval [CI], 0.09 to
0.54), as was the risk of requiring invasive mechanical ventilation (OR = 0.12, 95% CI, 0.05 to 0.29) [49].
Treatment and Hospital Course
On admission to the hospital, the patient is treated
with methylprednisolone, albuterol, and ipratropium. Supplemental oxygen is administered because of the
patient’s hypoxia, and NPPV is instituted to treat his hypercarbia. The hypercarbia and hypoxia resolve with these therapies. Sputum cultures are positive for H. influenzae, and an
appropriate antibiotic agent is administered intravenously
for 3 days; the patient is then switched to an oral agent for a
7-day course.
Four days after admission, after his dyspnea has improved and he has been stable for 24 hours, the patient is discharged from the hospital. He completes the antibiotic regimen and a steroid taper as an outpatient. At a follow-up visit
to his primary care physician 2 weeks after discharge, his
respiratory status has returned to baseline.
Future Directions
A number of new modalities for the diagnosis and treatment
of COPD are being investigated. Research has been directed
at identifying biologic markers of infection and inflammation (eg, antioxidants, cytokines) in the blood and/or sputum. Future research in therapeutics for COPD may address
the components of mucus formation and content; strategies
for improving muscle strength and reducing muscle fatigue;
therapies aimed at aborting the exacerbation cycle; and
strategies aimed at preventing infectious exacerbations.
Authors’ address: Box 3221, Duke University Medical Center, Durham,
NC 27710.
JCOM November 2000 47
COPD EXACERBATIONS
References
1. Petty TL, Weinmann GG. Building a national strategy for the
prevention and management of and research in chronic
obstructive pulmonary disease. National Heart, Lung, and
Blood Institute Workshop Summary. JAMA 1997;277:246–53.
2. US Department of Commerce, Bureau of Commerce.
Statistical Abstract of the United States 1997. Washington
(DC): The Department; 1997.
3. Standards for the diagnosis and care of patients with chronic obstructive pulmonary disease. American Thoracic
Society. Am J Respir Crit Care Med 1995;152(5 Pt 2):S77–121.
4. Anthonisen NR, Manfreda J, Warren CP, et al. Antibiotic
therapy in exacerbations of chronic obstructive pulmonary
disease. Ann Intern Med 1987;106:196–204.
5. Sherman S, Skoney JA, Ravikrishnan KP. Routine chest radiographs in exacerbations of chronic obstructive pulmonary
disease. Diagnostic value. Arch Intern Med 1989;149:2493–6.
6. Emerman CL, Cydulka RK. Evaluation of high-yield criteria
for chest radiography in acute exacerbation of chronic obstructive pulmonary disease. Ann Emerg Med 1993;22:680–4.
7. Emerman CL, Connors AF, Lukens TW, et al. Relationship
between arterial blood gases and spirometry in acute exacerbations of chronic obstructive pulmonary disease. Ann
Emerg Med 1989;18:523–7.
8. Emerman CL, Cydulka RK. Use of peak expiratory flow rate
in emergency department evaluation of acute exacerbation
of chronic obstructive pulmonary disease. Ann Emerg Med
1996;27:159–63.
9. Miravitlles M, Espinosa C, Fernandez-Laso E, et al. Relationship between bacterial flora in sputum and functional
impairment in patients with acute exacerbations of COPD.
Group of Bacterial Infection in COPD. Chest 1999;116:40–6.
10. Gump DW, Phillips CA, Forsyth BR, et al. Role of infection
in chronic bronchitis. Am Rev Respir Dis 1976;113:465–74.
11. Beaty CD, Grayston JT, Wang SP, et al. Chlamydia pneumoniae,
strain TWAR, infection in patients with chronic obstructive
pulmonary disease. Am Rev Respir Dis 1991;144:1408–10.
12. Smith CB, Golden CA, Kanner RE, et al. Association of viral
and Mycoplasma pneumoniae, infections with acute respiratory illness in patients with chronic obstructive pulmonary
diseases. Am Rev Respir Dis 1980;121:225–32.
13. Schaberg T, Gialdroni-Grassi G, Huchon G, et al. An analysis of decisions by European general practitioners to admit
to hospital patients with lower respiratory tract infections.
The European Study Group of Community Acquired
Pneumonia (ESOCAP) of the European Respiratory Society.
Thorax 1996;51:1017–22.
14. Backman R, Hellstrom P. Fenoterol and ipratropium bromide for treatment of patients with chronic bronchitis. Curr
Ther Res 1985;38:135–40.
15. Karpel JP, Pesin J, Greenberg D, Gentry E. A comparison of
the effects of ipratropium bromide and metaproterenol sulfate in acute exacerbations of COPD. Chest 1990;98:835–9.
16. Zehner WJ Jr, Scott JM, Iannoli PM, et al. Terbutaline vs.
albuterol for out-of-hospital respiratory distress: a randomized, double-blind trial. Acad Emerg Med 1995;2:686–91.
17. Lloberes P, Ramis L, Monserrat JM, et al. Effect of three dif48 JCOM November 2000
18.
19.
20.
21.
22.
23.
24.
25.
26.
27.
28.
29.
30.
31.
32.
33.
34.
ferent bronchodilators during an exacerbation of chronic
obstructive pulmonary disease. Eur Respir J 1988;1:536–9.
O‘Driscoll BR, Taylor RJ, Horsley MG, et al. Nebulised salbutamol with and without ipratropium bromide in acute airflow obstruction. Lancet 1989;1:1418–20.
Albert RK, Martin TR, Lewis SW. Controlled clinical trial of
methylprednisolone in patients with chronic bronchitis and
acute respiratory insufficiency. Ann Intern Med 1980;92:753–8.
Bullard MJ, Liaw SJ, Tsai YH, Min HP. Early corticosteroid
use in acute exacerbations of chronic airflow obstruction.
Am J Emerg Med 1996;14:139–43.
Emerman CL, Connors AF, Lukens TW, et al. A randomized
controlled trial of methylprednisolone in the emergency treatment of acute exacerbations of COPD. Chest 1989;95:563–7.
Thompson WH, Nielson CP, Carvalho P, et al. Controlled
trial of oral prednisone in outpatients with acute COPD exacerbation. Am J Respir Crit Care Med 1996;154(2 Pt 1):407–12.
Davies L, Angus RM, Calverley PM. Oral corticosteroids in
patients admitted to hospital with exacerbations of chronic
obstructive pulmonary disease: a prospective randomised
controlled trial. Lancet 1999;354:456–60.
Niewohner DE, Erbland ML, Deupree RH, et al. Effect of systemic glucocorticoids on exacerbations of chronic obstructive
pulmonary disease. Department of Veterans Affairs Cooperative Study Group. N Engl J Med 1999;340:1941–7.
Berry DG, Fry J, Hindley CP, et al. Exacerbations of chronic
bronchitis: treatment with oxytetracycline. Lancet 1960;1:137–9.
Elmes PC, Fletcher CM, Dutton AA. Prophylactic use of
oxytetracycline for exacerbations of chronic bronchitis. BMJ
1957;(5056):1272–5.
Fear EC, Edwards G. Antibiotic regimes in chronic bronchitis. Brit J Dis Chest 1962;56:153–62.
Jorgensen AF, Coolidge J, Pedersen PA, et al. Amoxicillin in
treatment of acute uncomplicated exacerbations of chronic bronchitis. A double-blind, placebo-controlled multicentre study in
general practice. Scand J Prim Health Care 1992;10:7–11.
Nicotra MB, Rivera M, Awe RJ. Antibiotic therapy of acute
exacerbations of chronic bronchitis. A controlled study using
tetracycline. Ann Intern Med 1982;97:18–21.
Petersen ES, Esmann V, Honcke P, Munkner C. A controlled
study of the effect of treatment on chronic bronchitis. An
evaluation using pulmonary function tests. Acta Med Scand
1967;182:293–305.
Pines A, Raafat H, Greenfield JS, et al. Antibiotic regimens in
moderately ill patients with purulent exacerbations of
chronic bronchitis. Br J Dis Chest 1972;66:107–15.
Elmes PC, King TK, Langlands JH, et al. Value of ampicillin
in the hospital treatment of exacerbations of chronic bronchitis. BMJ 1965;(5467):904–8.
Pines A, Raafat H, Plucinski K, et al. Antibiotic regimens in
severe and acute purulent exacerbations of chronic bronchitis. BMJ 1968;2:735–8.
Sachs AP, Koeter GH, Groenier KH, et al. Changes in symptoms, peak expiratory flow, and sputum flora during treatment with antibiotics of exacerbations in patients with
chronic obstructive pulmonary disease in general practice.
Thorax 1995;50:758–63.
Vol. 7, No. 11
CASE-BASED REVIEW
35. Saint S, Bent S, Vittinghoff E, Grady D. Antibiotics in chronic obstructive pulmonary disease exacerbations. A metaanalysis [see comments]. JAMA 1995;273:957–60.
36. Petersen ES, Esmann V, Honcke P, Munkner C. A controlled
study of the effect of treatment on chronic bronchitis. An
evaluation using pulmonary function tests. Acta Medica
Scandinavica 1967; 182(3):293-305.
37. Fingiguerra M, Conti P, Figura I, et al. Clinical study on the
effects of an antibiotic and mucolytic association (amoxicillin
and domiodol) in hypersecretory chronic bronchopulmonary diseases. Curr Ther Res 1982;31:895–905.
38. Aylward M, Maddock J, Dewland P. Clinical evaluation of
acetylcysteine in treatment of patients with chronic obstructive bronchitis: a balanced double-blind trial with placebo
control. Eur J Respir Dis Suppl 1980;111:81–9.
39. Langlands JH. Double-blind clinical trial of bromhexine as a
mucolytic drug in chronic bronchitis. Lancet 1970;1:448–50.
40. Peralta J, Poderoso JJ, Corazza C, et al. Ambroxol plus amoxicillin in the treatment of exacerbations of chronic bronchitis.
Arzneimittelforschung 1987;37:969–71.
41. Newton DA, Bevans HG. Physiotherapy and intermittent
positive-pressure ventilation of chronic bronchitis. Br Med J
1978;2:1525–8.
42. Wollmer P, Ursing K, Midgren B, Eriksson L. Inefficiency of
chest percussion in the physical therapy of chronic bronchitis. Eur J Respir Dis 1985;66:233–9.
43. Bone RC, Pierce AK, Johnson RL Jr. Controlled oxygen
administration in acute respiratory failure in chronic obstructive pulmonary disease: a reappraisal. Am J Med 1978;
65:896–902.
44. Keenan SP, Kenerman PD, Cook DJ, et al. Effect of noninvasive positive pressure ventilation on mortality in patients
admitted with acute respiratory failure: a meta-analysis.
Crit Care Med 1997;25:1685–92.
45. Continuous or nocturnal oxygen therapy in hypoxemic
chronic obstructive lung disease: a clinical trial. Nocturnal
Oxygen Therapy Trial Group. Ann Intern Med 1980;93:391–8.
46. Brochard L, Mancebo J, Wysocki M, et al. Noninvasive ventilation for acute exacerbations of chronic obstructive pulmonary
disease [see comments]. N Engl J Med 1995;333:817–22.
47. Kramer N, Meyer TJ, Meharg J, et al. Randomized, prospective trial of noninvasive positive pressure ventilation in
acute respiratory failure. Am J Respir Crit Care Med 1995;
151:1799–806.
48. Angus RM, Ahmed AA, Fenwick LJ, Peacock AJ. Comparison of the acute effects on gas exchange of nasal ventilation and doxapram in exacerbations of chronic obstructive
pulmonary disease. Thorax 1996;51:1048–50.
49. Barbe F, Togores B, Rubi M, Pons S, Maimo A, Agusti AG.
Noninvasive ventilatory support does not facilitate recovery
from acute respiratory failure in chronic obstructive pulmonary disease. Eur Respir J 1996;9:1240–5.
Copyright 2000 by Turner White Communications Inc., Wayne, PA. All rights reserved.
Vol. 7, No. 11
JCOM November 2000 49