Rheumatoid basics
advertisement

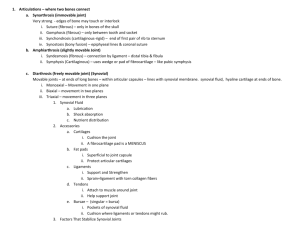
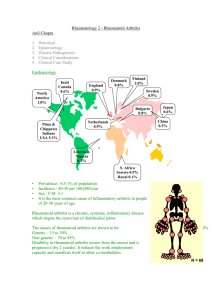
RHEUMATOID ARTHRITIS Definitions Rheumatoid arthritis (RA) is a systemic autoimmuine inflammatory disease involving primarily the synovial membranes. Diagnostic criteria - 4 of 7 (American College of Rheumatology). Symptoms must be present for at least six weeks: 1. Morning stiffness lasting longer than 1 hour before improvement 2. Arthritis involving 3 or more joints 3. Bilateral joint involvement (ie, both wrists, symmetric PIP and MCP joints) 4. Arthritis of the hand, particularly involvement of the proximal interphalangeal (PIP) joints, metacarpophalangeal (MCP) joints, or wrist joints 5. Positive serum rheumatoid factor (RF) 6. Rheumatoid nodules (50-80%) 7. Radiographic evidence of RA Joint space narrowing Periarticular osteopenia Juxtaarticular erosions Periarticular soft tissue swelling Subluxation and gross deformity Epidemiology 1% in US. Lower in Asia 3:1 F:M incidence increases with advancing age. Peak incidence 40-60 years. Prognosis clinical course of the disease is variable and ranges from mild, self-limited arthritis to a progressive multisystem disease Daily living activities are impaired in most patients. Spontaneous clinical remission is uncommon (approximately 5-10%). After 5 years of disease, approximately 33% of patients will not be working; after 10 years, 50% will have substantial functional disability. Poor prognostic factors: 1. persistent synovitis 2. early erosive disease 3. extra-articular findings (including subcutaneous rheumatoid nodules), 4. positive serum RF findings although worse outcome than seronegative, response to surgery is more predictable 5. elevated acute-phase markers (ESR/CRP) 6. family history of RA 7. female sex 8. advanced age. Life expectancy for patients with RA is shortened by 5-10 years, although those who respond to therapy may have lower mortality rates Mortality is increased by causes such as infections, cardiovascular disease, renal disease, GI bleeding, and lymphoproliferative disorders; these events may be directly due to the disease and its complications (eg, vasculitis, amyloidosis) or to therapy-induced adverse effects. Aetiology RA is associated with a number of autoimmune responses, but whether autoimmunity is a secondary or primary event is still unknown. Genetics The so-called shared epitope of the HLA-DR4/DR1 cluster is present in up to 90% of patients with RA, although it is also present in more than 40% of controls. Environmental infectious agents have been suggested to induce RA. Among these are Mycoplasma organisms, Epstein-Barr and rubella viruses, and others. Hormonal Sex hormones may play a role, as evidenced by the disproportionate number of females with RA, its amelioration during pregnancy, its recurrence in the early postpartum period, and its reduced incidence in women using oral contraceptives. Immunology Th-1 CD4 cells play a central role (produce IL-2 and interferon gamma.) They activate macrophages and other cell populations, including synovial fibroblasts. The latter 2 populations are the main producers of the proinflammatory cytokines TNFalpha and IL-1 that appear to be the major driving forces of inflammation. Experimental models suggest that synovial macrophages and fibroblasts may become autonomous and thus lose responsiveness to T-cell activities in the course of the disease. The hyperactive and hyperplastic synovial membrane is ultimately transformed into pannus tissue and invades cartilage and bone, the latter being degraded by activated osteoclasts. The major difference between RA and other forms of inflammatory arthritis, such as psoriatic arthritis, does not lie in their cytokine patterns but rather in the highly destructive potential of the RA synovial membrane and in the local and systemic autoimmunity. Whether these 2 events are linked is unclear; however, the autoimmune response conceivably leads to the formation of immune complexes activating the inflammatory process to a much higher degree than is otherwise the case. This theory is supported by the much worse prognosis of RA among patients positive for RF. Pathophysiology RA is characterized by 1. destructive synovitis 2. digital vasculitis 3. rheumatoid nodules 4. carpal tunnel syndrome Synovitis Proliferative phase characterized by swelling and fibrin deposition that cause pain with motion, decreased movement, and nerve compression. It starts in the synovial membrane, with the initial processes of edema, neovascularization, and hyperplasia of the synovial lining. proliferative tissue is composed of synoviocytes that resemble macrophages and fibroblasts. Accompanying the synovial proliferation is angiogenesis to support the new growth and allow leukocyte infiltration. The influx of leukocytes is composed of T cells, B cells, macrophages, and plasma cells thickening of the synovial lining forms the pannus. Destructive Phase Pannus is a sheet of invasive cellular tissue that is continuous with the synovial lining Synovium or pannus invades both tendon sheath and synovial joints causing tendon displacement and abnormal pull, tendon rupture and articular damage. Prominent villous formation occurs in the synovium, as does an inflammatory joint effusion. The effusion causes capsule distension and stretching of the ligamentous tissues, resulting in laxity of the capsule. With further progression of disease, the joint becomes unstable and subluxate. high level of proinflammatory cytokines is also present along with matrix metalloproteinase production. 2 main cytokines are tumor necrosis factor-alpha and interleukin-1, which induce cellular proliferation, matrix metalloproteinase expression, adhesion molecule expression, and secretion of other cytokines and prostaglandins. Matrix metalloproteinase degrades extracellular matrix components and is implicated in the cartilage and bone destruction that occurs in the later stages of RA. Increased adhesion molecule expression aids in recruiting leukocytes to the joint spaces and may perpetuate the inflammatory reaction and allow pannus to attach to cartilage and bone. Reparative/Deformational Phase inflammatory reaction extinguishes and is replaced by fibrosis, which causes tendon adhesions, fibrous ankylosis and fixed deformities 1. imbalance between flexor and extensor tendons, which produces the characteristic hand deformities. Classifications FUNCTIONAL STAGING (ACR) Class I - Completely able to perform all activities of daily living Class II - Able to perform usual self-care and vocational activities but limited in avocational activities (hobbies) Class III - Able to perform usual self-care activities but limited in vocational and avocational activities Class IV - Limited in ability to perform usual self-care, vocational, and avocational activities REMISSION OF RA * Five or more of the following conditions present for at least 2 consecutive months 1. Duration of morning stiffness not exceeding 15 minutes 2. No fatigue 3. No joint pain 4. No joint tenderness or pain with motion 5. No soft tissue swelling in joints or tendon sheaths 6. ESR of less than 30 mm/h for a female or less than 20 mm/h for a male STAGING HAND SURGERY STAGE I synovitis without deformity STAGE II synovitis with passively correctable deformity STAGE III fixed deformity without joint involvement STAGE IV articular destruction Clinical History Time and Onset of Disease 1. monocyclic – only 1 attack followed by permanent remission (10%) 2. polycyclic – intermittent attacks of differing severity (45%) 3. progressive – unremitting, inexorfable course (45%) Major Problems Other Problems Previous Treatment Functional Assessment Self care, work, hobbies Use of aids Pain Weakness/Stiffness Numbness and Parasthesias Medications Examination Deformity Posterior subluxation of elbow Palmar subluxation of wrist Ulnar translocation of carpus Radial deviation of metacarpus Ulnar drift of fingers Volar subluxation of MCPJ Swan neck and Boutonniere deformities of fingers Z deformity of thumb Lateral dislocation of IPJ Swelling Rheumatoid nodules Benign pseudo-rheumatoid nodules Identical histologically but without other stigmata of rheumatoid disease Rheumatoid nodulosis Similar nodules in Rh(+) patients but no joint destruction or deformity Prominent ulnar head Synovial swelling Tenderness Stiffness Pain on motion Limitation on motion Extraarticular manifestations Rheumatoid nodules Investigations Imaging Xrays o o o o soft tissue swelling juxta-articular demineralization uniform joint-space narrowing erosions (rarely) - often first evident at the ulnar styloid and at the juxta-articular margins, where the bony surface is not protected by cartilage. U/S – easily reveal soft tissue swelling and shows up erosions in 80% of patients at first presentation MRI – may reveal synovial hypertrophy as early as 4 months after the onset of synovitis Blood tests FBC, ESR/CRP, Rh, ANA Systemic Review Cervical spine instability o Nearly one third of patients have unstable cervical joints, with atlantoaxial (C1-C2) subluxation being the most common instability. o Myelopathy secondary to rupture of the transverse ligament may lead to neurologic deficits. o Radiculopathy is most common at the C2 root, though symptomatic subluxations may occur at any level. o Pain frequently radiates over the occiput region in the distribution of the C1-3 nerve roots. o The Lhermitte sign, in which tingling paresthesias that descends through the thoracolumbar spine into the limbs, occurs as the neck is flexed, is typically observed. TMJ involvement Pulmonary involvement Felty's syndrome (splenomegaly and neutropaenia) Anemia of chronic disease Sjogren’s syndrome – dry eyes Medical Management Medications 1. NSAIDS 2. Gold compounds o For patients who fail to improve on or who cannot tolerate methotrexate o Gold is taken by macrophages, which in turn inhibit phagocytosis and lysosomal membrane stabilization. 3. Immunosuppressants o Methotrexate o Cyclophosphamide 4. Antimalarials o Hydroxychloroquine - inhibits chemotaxis of eosinophils, inhibits locomotion of neutrophils, and impairs complement-dependent antigen-antibody reactions 5. Antiinflammatories o Sulfasalazine - decreases inflammatory reactions and systemically inhibits prostaglandin synthesis. 6. Steroids 7. Penicillamine o depresses circulating IgM rheumatoid factor and T-cell activity but does not affect Bcell activity 8. Anti-TNF o Adalimumab Recombinant human IgG1 monoclonal antibody specific for human TNF o Etanercept recombinant human TNFa-receptor fusion protein. interferes with the inflammatory cascade by binding to TNFa, thereby blocking its interaction with cell-surface receptors. o Infliximab chimeric monoclonal antibody that binds with high affinity to TNFa, thereby neutralising its activity. early intervention offers RA patients the most promise for preventing irreversible joint damage and avoiding severe disability. combination treatment, with DMARDs as well as with biologic agents, has been shown to yield more favorable outcomes than a single treatment. Continuation of DMARDs during surgery o Continuation of methotrexate treatment does not increase the risk of either infections or of surgical complications occurring in patients with RA within one year of elective orthopaedic surgery. Thus methotrexate treatment should not be stopped in patients whose disease is controlled by the drug before elective orthopaedic surgery. (Ann Rheum Dis. 2001) o in patients with RA undergoing elective foot and ankle surgery, the use of TNFalpha inhibition agents may be safely undertaken in the perioperative period without increasing the risk of healing or infectious complications. (Foot Ankle Int. 2004) o no statistically significant risk of wound infection or breakdown in patients taking methotrexate or steroids or both having surgical procedures on the hand and wrist (J Hand Surg [Am]. 2002) AIMS and SURGICAL GOALS 1. Pain relief 2. Improvement of function 3. Retardation of disease progression 4. Improvement of cosmesis SURGICAL SEQUENCE Painful before painless Function before cosmetic High priority to tendon ruptures and significant nerve compressions lower extremity recon. to be completed before hand and wrist in most cases proximal before distal, alternating fusion with motion-sparing procedures stabilizing operations before mobilizing operations procedures that are predictable and have a high patient acceptance procedures that are complimentary tendon reconstruction before MP arthroplasty thumb alignment to follow digital reconstruction so as to place the thumb in the most useful position Indications for surgery 1. nodules 2. triggering 3. rupture 4. compression 5. prevention of progression 6. instability (pain) 7. mobility (function) 8. deformity (aesthetics) Five basic surgical procedures 1. synovectomy 2. tenosynovectomy 3. tendon surgery 4. arthroplasty 5. arthrodesis