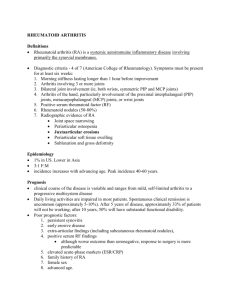
RHEUMATOID ARTHRITIS PRESENTED BY HEENA AMNA Subgroup: 6th Student of Medical faculty No.2 A chronic progressive disease causing inflammation in the joints and resulting in painful deformity and immobility, especially in the fingers, wrists, feet, and ankles. EPIDEMIOLOGY Prevalence: Rheumatoid arthritis (RA) is estimated to affect approximately 0.24 to 1 percent of the population. Sex: ♀ > ♂ (3:1); predominantly affects middle-aged women. Incidence: The annual incidence of RA in the United States and northern European countries is estimated to be approximately 40 per 100,000 persons Peak incidence: 50–75 years. Prevalence of self-reported rheumatoid arthritis, by age and sex, 2017–18 ETIOLOGY Chronic inflammatory autoimmune disorder of unknown etiology Genetic disposition: RA appears to be associated with specific HLA types (HLA-DR4, HLA-DR1). Hypotheses suggest the etiology is multifactorial, with the following factors playing a role: Environmental triggers (e.g., infection, tobacco) Hormonal factors PATHOPHYSIOLOGY • Initially, non-specific inflammation affects the synovial tissue, which is later amplified by activation of T-cells (autoimmune response). • With time, it may lead to inflammatory joint effusion and synovial hypertrophy, as well as progressive destruction and deterioration of cartilage and bone. • Synovial lining hyperplasia • Pannus formation along the synovial tissue → produce proteinases → destroy cartilage extra-cellular matrix • Patients with positive rheumatoid factor (RF) are more likely to develop extra-articular manifestations of rheumatoid arthritis. Synovial pannus formation and bone invasion: proliferative granulation tissue with mononuclear inflammatory cells Angiogenesis Synovial lining hyperplasia with mononuclear cell infiltrate Perivascular inflammatory infiltrates Fibrin deposition on synovial surfaces Characteristic histology of rheumatic nodules: central fibrinoid necrosis with histiocytes and surrounding epithelioid cells SCHEMATIC REPRESENTATION OF THE PATHOPHYSIOLOGY OF RA 1) Initially, non-specific inflammation of the synovial tissue, joint swelling, osteoporosis of the surrounding bones over the course of disease, as well as the erosion; 2)Progressive destruction and deterioration of cartilage and bone; 3)Complete joint destruction with malpositioning and loss of mobility in the end stage of the disease. CLINICAL FEATURES ARTICULAR MANIFESTATIONS: • Polyarthralgia • Symmetrical pain and swelling of affected joints (also at rest). • Frequently affected joints: • Metacarpophalangeal joints (MCPJs) • Proximal interphalangeal joints (PIPJs) • Wrist joints • Knee joints • Joints of the axial skeleton are usually spared except for the cervical spine • Morning stiffness > 30 min; often improves with activity. • Joint deformities • "Rheumatoid hand" is characteristic, and can include the following deformities: • Deepening of the interosseous spaces of the dorsum of hand • Swan neck deformity: PIP hyperextension and DIP flexion • Boutonniere deformity: PIP flexion and DIP hyperextension. • Hitchhiker thumb deformity (Z deformity of the thumb): hyperextension of the interphalangeal joint with fixed flexion of the MCP joint • Ulnar deviation of the fingers • Hammer toe • Atlanto-axial subluxation Female patient with RA: Swelling especially of the PIP joints Hands of a male patient: Swan neck deformity on the 4th and 5th fingers of the left hand with hyperextension of PIP joint and flexion of the DIP joint. Also there is pronounced swelling of the MCP joint. Common deformities of the lesser toes Rheumatoid nodules:Multiple erythematous subcutaneous nodules are visible at the MCP, PIP and DIP joints EXTRA-ARTICULAR MANIFESTATIONS: Constitutional symptoms: low-grade fever, myalgia, malaise, night sweats Skin: rheumatoid nodules (common); non-tender, firm, subcutaneous swellings (2 mm–5 cm) Lungs: fibrosis, nodules, pleuritis, and pleural effusions Eye: Keratoconjunctivitis sicca, scleritis, and episcleritis Endocrine and exocrine glands: secondary Sjogren syndrome Hematological: anemia of chronic disease EXTRA-ARTICULAR MANIFESTATIONS: • Other musculoskeletal • Tenosynovitis and bursitis • Carpal tunnel syndrome (entrapment neuropathy) • Typical nocturnal paresthesia of volar hand and fingers I–III • Atrophy of thenar muscles → difficulty making a fist; inability to oppose the thumb • Tarsal tunnel syndrome • Heart: Pericarditis and myocarditis; higher risk of myocardial infarction, stroke, and CHF • Vascular: Peripheral vasculitis manifesting as livedo reticularis, Raynaud phenomenon, purpura, necrosing fingertips or peripheral neuropathy RHEUMATOID ARTHRITIS FACTSHEET SUBTYPES AND VARIANTS • RA of the cervical spine • RA normally spares the thoracic and lumbar spine. In some cases, it initially affects the cervical spine, causing early-morning neck pain at rest. • Complication: atlanto-axial subluxation • Life-threatening complication! • Symptoms • • • • Pain and stiffness of the neck Neurological deficits, e.g., cervical radiculopathy with peripheral paresthesias Deformity, e.g., stiffness and scoliosis In some cases, symptoms of high spinal cord compression • Slowly progressive spastic quadriparesis • Hyperreflexia or positive Babinski reflex • Respiratory insufficiency • Diagnosis • Extension and flexion x-rays of the cervical spine • MRI • Treatment: surgery if instability or myelopathy are present • Felty syndrome • Definition: Felty syndrome is a severe subtype of seropositive RA. • Clinical features • Clinical triad consisting of arthritis, splenomegaly, and neutropenia (leads to ↑ risk of recurrent bacterial infections) • Other symptoms: skin ulcers of the lower limbs (indicating vasculitis), hepatomegaly, fever, and chest pain (indicating pleuritis or pericarditis) • Diagnosis • Leukopenia with selective neutropenia • ↑↑ RF • ↑↑ ACPA • Treatment • • • • DMARD: methotrexate Alternative: cyclophosphamide Prompt and aggressive antibiotic treatment for suspected infections Consider splenectomy to treat leukopenia and improve the disease course. DIAGNOSTICS • ACR criteria for RA (ACR/EULAR classification criteria (2010) LABORATORY TESTS NON-SPECIFIC PARAMETERS SPECIFIC PARAMETERS (SEROLOGY) SYNOVIAL FLUID ANALYSIS • ↑ Inflammatory markers: CRP, ESR correlate with inflammatory activity. • ↑ Ferritin as an acute phase protein. • Possibly leukocytosis, thrombocytosis • Anemia of chronic disease • Anti-citrullinated peptide antibodies (e.g., anti-CCP) --> Sensitivity >90% • Rheumatoid factor (RF) --> IIgM autoantibodies against the Fc region of IgG, Low specificity • Antinuclear antibodies (ANA): elevated in 30% of cases • Synovial fluid is collected by joint aspiration. • Findings : (1) Cloudy yellow appearance, (2) Sterile specimen with leukocytosis (WBC: 5,000–50,000/μL), (3) ↑ Neutrophils, granulocytes and ragocytes, (4) ↑ Proteins, ↓ viscosity; (5) Possibly rheumatoid factor IMAGING • Conventional x-ray • Dorso-palmar x-ray of both hands • Radiological findings • Early: soft tissue swelling, demineralization (juxta-articular) • Late: joint space narrowing, erosions of cartilage and bone, demineralization (generalized) Even if radiographic findings are normal, RA is still possible! • MRI: (with or without contrast), especially if cervical spine involvement is suspected or in early stages • Ultrasound: joint effusion, formation of pannus • Further diagnostic measures: contrast-enhanced ultrasound, scintigraphy KNEE JOINT DESTRUCTION IN RA Anteroposterior x-ray of the right knee Severe erosive changes with joint space narrowing and valgus deformity RA: X-ray of both hands (PA view) Generalized decrease of bone radiodensity & narrowing of the joint spaces of MCP, PIP and wrist joints. TREATMENT • General measures • For acute episodes of inflammation: cryotherapy • Physical and occupational therapy • Physical activity • Acute anti-inflammatory therapy • Indication: acute attack • Glucocorticoids: given until DMARD's onset of action or as long-term therapy for highly active RA. • Prevention of osteoporosis: optimization of sufficient calcium and vitamin D intake • NSAIDs and COX-2 inhibitors: symptomatic relief without improving prognosis • PPI's are recommended because combining glucocorticoids with NSAIDs substantially increases the risk of GI ulcers. • Long-term anti-inflammatory therapy with disease-modifying antirheumatic drugs (DMARDs) • Induce immunosuppresion, leading to potential remission of RA • Reduce mortality and morbidity by up to 30% • Slow onset of action (≥ 6 weeks), so symptomatic treatment with glucocorticoids and NSAIDs is often required • Non-biologic agents • Drug of choice: methotrexate (MTX) • First-line treatment for moderate to severe RA • Benefits: highly effective, relatively well-tolerated, low cost, possibly life-prolonging • To minimize side effects, folic acid is recommended 24–48 hours after taking MTX. • Biologic therapy • Indication: moderate or severe disease activity remaining after three months of DMARD therapy • Should be combined with non-biologic DMARDs • Tumor necrotic factor (TNF) α inhibitors: e.g., adalimumab, infliximab PROGNOSIS • Factors associated with poor prognosis • • • • • Prolonged disease progression without initiation of treatment Late onset (> 60 years of age) Sex: ♀ Smoking Social factors (e.g., low socioeconomic status, low level of education) • Laboratory tests associated with worsened prognosis if abnormally elevated • • • • CRP ESR ACPA RF titer THANK YOU FOR YOUR ATTENTION ANY QUESTIONS ? NO....? GREAT. GOODBYE