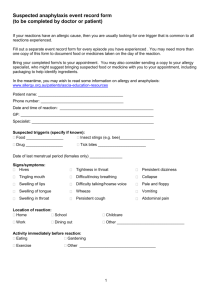
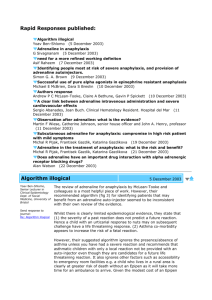
Anaphylaxis
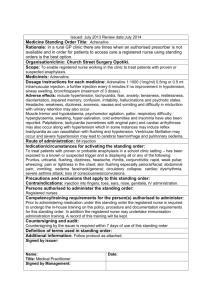
advertisement
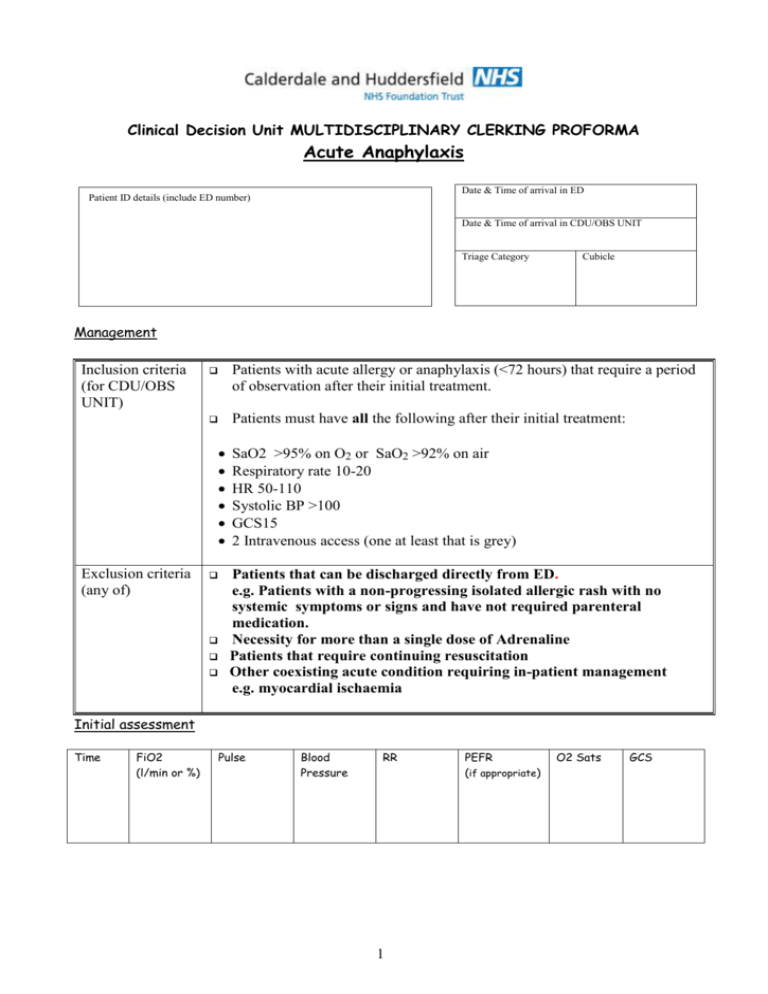
Clinical Decision Unit MULTIDISCIPLINARY CLERKING PROFORMA Acute Anaphylaxis Date & Time of arrival in ED Patient ID details (include ED number) Date & Time of arrival in CDU/OBS UNIT Triage Category Cubicle Management Inclusion criteria (for CDU/OBS UNIT) Patients with acute allergy or anaphylaxis (<72 hours) that require a period of observation after their initial treatment. Patients must have all the following after their initial treatment: Exclusion criteria (any of) SaO2 >95% on O2 or SaO2 >92% on air Respiratory rate 10-20 HR 50-110 Systolic BP >100 GCS15 2 Intravenous access (one at least that is grey) Patients that can be discharged directly from ED. e.g. Patients with a non-progressing isolated allergic rash with no systemic symptoms or signs and have not required parenteral medication. Necessity for more than a single dose of Adrenaline Patients that require continuing resuscitation Other coexisting acute condition requiring in-patient management e.g. myocardial ischaemia Initial assessment Time FiO2 (l/min or %) Pulse Blood Pressure RR 1 PEFR (if appropriate) O2 Sats GCS 2 Summary of Acute Anaphylaxis Management Guideline Management in ED Management in CDU/OBS UNIT: Observations: temperature, pulse, blood pressure, respiratory rate, SaO2, PEFR (if bronchospasm), GCS, Treatment: Resuscitation Intravenous access Adrenaline IM (IV)/ Chlorphenamine/ Steroids -as appropriate Nebulised bronchodilators if significant wheeze Consider H2 Blockade for resistant urticaria Patient must remain in ED for at least 2 hrs to confirm clinically stable prior to transfer to CDU Investigations: FBC, U&E, RBS Mast Cell Tryptase Observations: Continuous ECG and SaO2 monitoring Every 30 mins the patients general clinical status should be assessed along with the following observations: Airway assessment Pulse, Blood pressure, Respiratory Rate, PEFR (if bronchospasm) Treatment: Oxygen to keep SaO2 > 95%, Chlorphenamine 4mg tds (safe in pregnancy) Prednisolone 40mg od for 2-3 days Salbutamol 5mg neb for bronchospasm Timing of review If clinical deterioration- at any time If isolated urticaria - 2 hours All other patients - 6 hours Consider more prolonged observation (8-24hours) for: Severe reactions with slow onset Reactions in severe asthmatics or with a severe bronchospasm Reactions with the possibility of continuing absorption of allergen Patients with a previous history of biphasic reactions Criteria for discharge (All must be met) Criteria for admission (at any time) Indications for Epipen The patient must have normal physiology Symptoms and signs must be resolved or if still present have progressively improved during the observation period GP letter sent Discharge medication as above. (See indications for Epipen) Verbal and written discharge advice Referral for investigation (by GP) suggested on discharge letter Unstable patient requiring resuscitation of ABC'S Social circumstances prevent discharge Sudden onset life threatening reaction to unknown / unavoidable substance. High likelihood of recurrence 3 Emergency Management of Anaphylactic Reaction (From Resus Council(UK)) Airway, Breathing, Circulation, Disability, Exposure, Diagnosis - look for: • Acute onset of illness • Life-threatening Airway and/or Breathing and/or Circulation problems1 • And usually skin changes • Call for help • Lie patient flat • Raise patient’s legs Adrenaline2 When skills and equipment available: • Establish airway • High flow oxygen Monitor: • IV fluid challenge 3 • Pulse oximetry 4 • Chlorphenamine • ECG 5 • Hydrocortisone • Blood pressure 1 Life-threatening problems: Airway: swelling, hoarseness, stridor Breathing: rapid breathing, wheeze, fatigue, cyanosis, SpO2 < 92%, confusion Circulation: pale, clammy, low blood pressure, faintness, drowsy/coma 2 Adrenaline (give IM unless experienced with IV adrenaline) IM doses of 1:1000 adrenaline (repeat after 5 min if no better) • Adult • Child more than 12 years: • Child 6 -12 years: • Child less than 6 years: 500 micrograms IM (0.5 mL) 500 micrograms IM (0.5 mL) 300 micrograms IM (0.3 mL) 150 micrograms IM (0.15 mL) 3 IV fluid challenge: Adult 500 – 1000 mL Child crystalloid 20mL/kg Stop IV colloid if this might be the cause of anaphylaxis Adrenaline IV to be given only by experienced specialists Titrate: Adults 50 micrograms; Children 1 microgram/kg 4 Chlorphenamine (IM or slow IV) Adult or child more than 12 years Child 6 - 12 years Child 6 months to 6 years Child less than 6 months 10 mg 5 mg 2.5 mg 250 micrograms/kg 4 5 Hydrocortisone (IM or slow IV) 200 mg 100 mg 50 mg 25 mg Medical Notes History presenting complaint Past Medical History Drug History Examination findings Management: 1. 2. 3. 4. Impression/Diagnosis Signature Date Print Name Time 5 Investigations Requests The following investigations may be performed on all those with acute allergy / anaphylaxis Investigation When performed Dr/Nurse Time signature Reason if not performed ECG CXR Arterial blood gases FBC, U&E, glucose Mast Cell Tryptase Investigation results Result Signature Date/Time Hb ECG WCC Platelets Na K Chest X-ray Urea Creatinine FiO2 SaO2 Other investigations PH PO2 PCO2 Mast Cell Tryptase 6 Free text page (for use by all staff on CDU) Date and Time Comments / notes Signature 7 Free text page (for use by all staff on CDU) Date and Time Comments / notes Signature 8 CLINICAL DECISION UNIT DISCHARGE SUMMARY Anaphylaxis PATIENT NAME/ ADDRESSOGRAPH GP Details: Name Address ADDRESS DATE OF BIRTH Dear Dr Your patient attended the Clinical Decision Unit at Huddersfield Royal Infirmary with ANAPHYLAXIS / MODERATE ALLERGIC REACTION(delete as appropriate) The precipitant appeared to be Your Patient DID / DID NOT require Adrenaline to control their symptoms. □ Your patient has been advised to contact yourself or the Emergency Department at Huddersfield Royal Infirmary should there be any further problems. □ Your patient has been advised to contact yourself with a view to consideration of further investigation by an Immunologist Additional Comments Thank You Signed Name Designation Date ________________ 9