Adrenaline 2013
advertisement

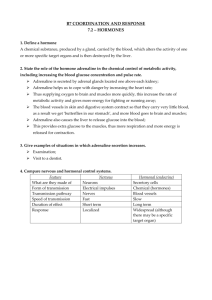
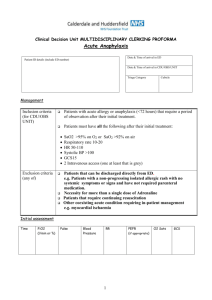
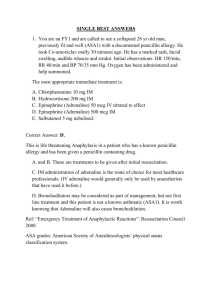
Issued: July 2013 Review date:July 2014 Medicine Standing Order Title: Adrenaline Rationale: In a rural GP clinic there are times when an authorised prescriber is not available and in order for patients to access care a registered nurse using standing orders is the best option. Organisation/clinic: Church Street Surgery Opotiki. Scope: To enable registered nurse working in the clinic to treat patients with proven or suspected anaphylaxis. Medicine/s: Adrenaline. Dosage instructions for each medicine: Adrenaline 1:1000 (1mg/ml) 0.5mg or 0.5 ml intramuscular injection, a further injection every 5 minutes if no improvement in hypotension, airway swelling, bronchospasm (maximum of 3 doses). Adverse effects: include hypertension, tachycardia, fear, anxiety, tenseness, restlessness, disorientation, impaired memory, confusion, irritability, hallucinations and psychotic states. Headache, weakness, dizziness, anorexia, nausea and vomiting and difficulty in micturition with urinary retention may also occur. Muscle tremor and hypokalaemia, psychomotor agitation, pallor, respiratory difficulty, hyperglycaemia, sweating, hyper-salivation, cold extremities and insomnia have also been reported. Palpitations, tachycardia (sometimes with anginal pain) and cardiac arrhythmias may also occur along with hypertension which in some instances may induce reflex bradycardia as can vasodilation with flushing and hypotension. Ventricular fibrillation may occur and severe hypertension may lead to cerebral haemorrhage and pulmonary oedema. Route of administration: IM injection Indication/circumstances for activating the standing order: To treat patients with proven or probable anaphylaxis in a school clinic setting – has been exposed to a known or suspected trigger and is displaying all or any of the following: Pruritus, urticarial, flushing, dizziness, headache, rhinitis, conjunctivitis; rapid, weak pulse; wheezing; pain or tightness in the chest; skin flushing especially perioral/facial; abdominal pain; vomiting; oedema face/neck/general; circulatory collapse; cardiac dysrhythmia, severe asthma attack; loss of consciousness/convulsions. Precautions and exclusions that apply to this standing order: Contraindications: injection into fingers, toes, ears, nose, genitalia, IV administration. Persons authorised to administer the standing order: Registered nurses. Competency/training requirements for the person(s) authorised to administer: Prior to administering medication under this standing order the registered nurse is required to undergo the in-house training on the policy, procedure and documentation requirements for this standing order. In addition the registered nurse may undertake immunisation administration training. A record of this training will be kept. Countersigning and audit: Countersigning by the issuer is required within 7 days of use of this standing order Definition of terms used in standing order: Additional information: Follow protocol as attached. Signed by issuer: Name: Title: Medical Practitioner Signed by Management: Date: Name: Title: Signed by Nurses working with Standing Order: Date: Name/s : Date: This Medicine Standing Order is not valid after the review date. Nurse Protocol for the Treatment of Anaphylaxis Registered Nurses may give Adrenaline 1:1000 IM to clients that have symptoms of anaphylaxis according to the following protocol: 1. ASSESS THE PATIENT USUALLY HAVE 3 OF THE FOLLOWING Red, raised and itchy rash, generalised rash Swollen face, swollen eyes Difficulty breathing – noisy breathing from airway obstruction (wheeze or stridor), difficulty swallowing, respiratory arrest Hypotension; tachycardia; dysrhythmias, circulatory arrest Abdominal cramps +/ diarrhoea 2. CALL FOR HELP - CALL AMBULANCE AIRWAY PATENCY: insert airway if necessary BREATHING: assist with oxygen, mouth to mouth, ambubag CIRCULATION: – CPR (Cardio Pulmonary Resuscitation) 3. ADMINISTER ADRENALINE Dosage: 1: 1000 Adrenaline 0.5ml deep IM (try deltoid first) You can expect to see some response to the adrenaline within 1 – 2 minutes. If necessary, adrenaline can be repeated at 5 – 15 minute intervals to a maximum of three doses, alternating sites/ limbs for additional doses 4. Administer OXYGEN @ 8 - 10L if there is respiratory distress (stridor, wheeze) 5. LIE FLAT Check BP and pulse - if hypotensive - elevate legs/feet If stridor present -elevate head/chest Record vital signs every 5 – 10 minutes and document fully all symptoms and treatment given. All cases of moderate to severe anaphylaxis should be admitted to hospital for observation as rebound anaphylaxis can occur 12 – 24 hours after the initial episode. Flow Chart Summary Anaphylaxis Suspected Assess Symptoms Airway Breathing Circulation Severe Symptoms: Mild / Moderate Symptoms Hypotension with collapse, bronchospasm, airway oedema + urticarial rash Rash, Urticaria Stop Medication. Stop Medication (if IV, withdraw blood from line and flush) Administer Adrenaline 0.5mg IM Assess Patient Position Supine - If available, administer high flow oxygen Report to appropriate Medical Officer (GP, Emergency Department, consulting doctor) and arrange patient review Dial 111 If in Cardiac arrest Monitor Patient: Commence CPR as indicated Perform CPR until ambulance arrives Elevate legs Administer adrenaline Persistent hypotension, bronchospasm or airway swelling 5 minutes after adrenaline: Repeat Adrenaline 0.5mg IM (maximum 3 doses) AMBULANCE HOSPITAL TRANSFER ASAP