bmt reportdoc
advertisement

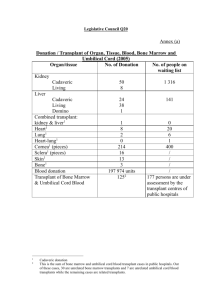
Bone Marrow Transplants: Are they Worth the Risks? The Nitty Gritty What is a Bone Marrow Transplant (BMT) exactly? Wait, what the heck is Bone Marrow? Well for starters, Bone Marrow is a soft and spongy material found inside of bones. The cells necessary for a BMT are found in the marrow of the breast bone, skull, hips, and spine. These are called Hematopoietic stem cells also known as bloodforming stem cells. They can form into any blood cell such as: White blood cells, Red blood cells, or platelets. The transplant part of all this comes in when someone had a disease that has destroyed or corrupted the bone marrow, or if they have received strong doses of radiation or chemo therapy in which the treatment destroyed the living bone marrow in the patient. There are three types of transplants: Autologous transplants, where the patients actually receive there own stem cells harvested at an earlier point when the marrow was not damaged or their marrow was harvested and cleaned of the disease, Syngeneic transplants, where a patient has an identical twin and receive stem cells from them, or an allogeneic transplant in which the patient receives stem cells from a family member with a close match or a complete stranger. A BMT is most commonly used on types on cancer such as Lymphoma and Leukemia. Other diseases include Aplastic Anemia, Melanoma and some varied other types of cancers. Infection When undergoing a transplant, the body has been administered very high doses of chemo therapy or radiation. These treatments have the ability to kill off all of the cancerous cells, but also have the ability to kill perfectly healthy cells along with them. By the time the high doses of chemo or radiation have been administered the patient has almost no immune system. Thus everyday things that we all encounter become potentially deadly breading grounds of bacteria and fungi. Bacteria: During the first two to four weeks a bacterial infection is rather common happening in up to 50 percent of patients. After a BMT the mucous membrane and skin barriers are damaged allowing more bacteria than normal to enter the body. Also the white blood cells and T-cells that are used to fight off harmful bacteria are in very low counts and do not have the ability to fight off everything. The antibodies in your blood that help immune you to chicken pox and other diseases are almost completely depleted as well. The mouth is a very common place for infection during this time. Small cuts from brushing teeth are a doorway for many bacteria. It is common for patients to get sours in the gums. These can be very painful while eating. Another area that is a common place of infection is the skin, especially where the shunt or central line is placed. These infections can be irritating and also painful. Other places for common infection are the intestines and the bladder and can cause pneumonia. Still it is very likely that if treated on time the patient will survive most of the possible bacterial infections. Fungal and Viral: With fungal infections, things are a little different. Fungal infections generally occur in a three month time period after the transplant. They are harder to find and kill than a bacterial infection. This is mainly because the fungi causing the infection is generally kept in check by bacteria on or in your body. Candida and Aspergillus are the most common of fungal infections posttransplant. Candida is a fungus that is generally not harmful in your body with a normal immune system. It lives in the mouth, intestines, and vagina and can generally be found in most humans. Due to the treatment, however, the bacteria that keeps Candida in check is killed per it could cause infection. This allows the fungus to multiply and spread out of control to many parts of the body. The other, Aspergillus, is found generally on construction sites or in houses being remodeled. It infects the sinus or lungs of the patient and can cause phenomena. Due to the fact that few effective anti-viral medications exist a viral infection can be devastating. Generally viral infections come about from a dormant virus that was in the patients body before the transplant. With nothing to stop it, it spreads through the body without a problem. The medications that treat certain viral infections work rather well but since they only treat few viruses in many cases they are useless. Herpes Simplex is the most common viral infection after the transplant. Others include Vericella Zoster Virus and Cytomegalovirus. The most common time for a viral infection to occur is up to twelve months after the transplant. However, in some cases it can occur up to two years post-transplant. Graft Versus Host Disease(GVHD) Around 50 percent of patients will most-likely develop GVHD. This is when the transplant attacks the patients body. The transplanted marrow sees its new home as a threat and starts to attack it. This is dangerous because the new home’s defenses have been severely compromised by chemo or radiation therapy. An older patient with a transplant is more likely to develop GVHD than a younger. Also if the the donor was not related or a perfect match this can higher the risk. Luckily most cases of GVHD are mild and not life threatening. If caught early and handled correctly it will be a minor issue. Although, it can become a life threatening disease either if not caught early or if other complications occur during the transplant. GVHD occurs in with an allogenic transplant due to the fact that the donor was most likely a stranger. Acute GVHD: This type of GVHD occurs within the first three months after the transplant. Generally to reduce the likelihood of developing GVHD the patient is given drugs that suppress the immune system. This is another part of the transplant that makes it easy for patients to get an infection. Acute GVHD affects the skin, liver, stomach, and intestines. It is rated on severity by how many organs it is effecting at once. A Lifethreatening case of Acute GVHD would have peeling or blistering skin and severe liver, stomach and intestinal issues. Chronic GVHD: Usually after the third month is when chronic GVHD may begin. This type may stick around with the patient for many years to life. In most cases it is not as severe as acute GVHD. It has common symptoms such as: dry or itching skin, rashes, partial hair loss or early greying, dry mouth, itching eyes, inability to absorb nutrients properly, or weight loss. On occasion some patients will experience difficulty to move arms or legs from tightening of tendons. Also it can affect the lungs causing pneumonia. Emotional Stress The procedure can have other affects on the patient besides physical. One of the biggest issues is the long periods of time spent alone. Being in a clean room away from normal society. The patient must be in appropriate gear before leaving the clean room. Visitors must wear appropriate gear as well. Physical touch from anyone other than a nurse or doctor is not recommended and that can make it hard as well. Depression can occur. The thought of never being able to leave the hospital. If the patient has a girlfriend or spouse this can be hard on the relationship as well. For the patient all they want is to be with their partner in an comfortable environment. For the healthy member never getting to spend quality time with their partner can emotionally detach them from that person and even make them lose interest. The patient can get angry and irritable. Sick of his or her surroundings and just wanting to go home. Then they are told they may not leave, this can create helplessness also. Adding such an emotional procedure onto an emotional sickness can be more difficult on the patient than the physical aspects. So Is It Worth It? Depending on the reason for the transplant most would say yes. Generally the alternate option means waiting for an almost certain death. When a transplant is offered the chances of survival without one are generally less than 10 percent. After the transplant, depending on many circumstances, it can raise that to in many cases 80 percent or higher. Of course their are many things that go into the likelihood of success but it most cases it is worth the risks to try and live than sit and wait for death. Work Cited "Bone Marrow Transplants -- Table of Contents." BMT InfoNet Homepage. BMTinfonet. Web. 15 Feb. 2010. <http://www.bmtinfonet.org/bmt/bmt.book/toc.html>. "BMT and Peripheral Blood Stem Cell Transplant - National Cancer Institute." National Cancer Institute - Comprehensive Cancer Information. U.S. National Institutes of Health, 29 Oct. 2008. Web. 16 Feb. 2010. <http://www.cancer.gov/cancertopics/factsheet/Therapy/bonemarrow-transplant>. "History of bone marrow transplant treatment -." National Bone Marrow Transplant Link. 2010. Web. 16 Feb. 2010. <http://www.nbmtlink.org/resources_support/rg/rg_intro.htm>. "Anatomy of a bone, showing blood cells used in pediatric bone marrow transplants." Packard Children's Hospital at Stanford LPCH: Northern California Children's Hospital. Web. 15 Feb. 2010. <http://www.lpch.org/DiseaseHealthInfo/HealthLibrary/oncology/0062-pop.html>.