Table of contents Additional Topic 1: Infection prevention Principles
advertisement

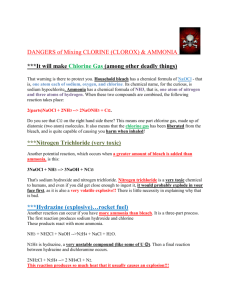
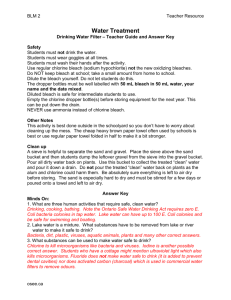
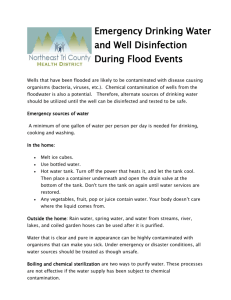
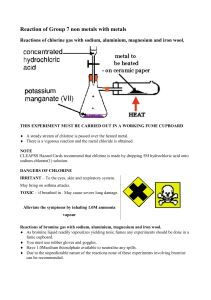
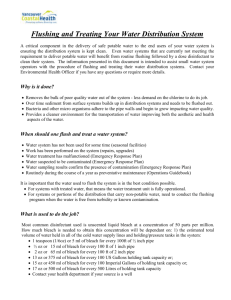
Prevention of Postpartum Hemorrhage: Implementing Active Management of the Third Stage of Labor (AMTSL) A Reference Manual for Health Care Providers Additional Topic 1: Infection prevention Table of contents Additional Topic 1: Infection prevention ........................................................................ 3 Principles of infection prevention ............................................................................ 3 Hand washing ...................................................................................................... 3 Gloves ................................................................................................................ 3 Aprons or gowns .................................................................................................. 4 Handling sharp instruments ................................................................................... 4 Preventing splashes .............................................................................................. 5 Waste disposal ..................................................................................................... 5 The steps of processing instruments ....................................................................... 5 Making a chlorine decontamination solution ............................................................. 7 References .............................................................................................................. 11 List of tables Table 6. Steps and benefits for processing instruments for reuse ..................................... 6 Table 7. Mixing a 0.5 percent chlorine decontamination solution 29 .................................... 9 List of figures Figure 24. One-hand needle-recapping technique ........................................................... 4 2 Prevention of Postpartum Hemorrhage: Implementing Active Management of the Third Stage of Labor Reference manual Additional Topic 1: Infection prevention This section provides guidelines on infection prevention practices to use when providing maternal and newborn services and is adapted from materials developed by JHPIEGO, EngenderHealth, and WHO. 32, 33, 34 Principles of infection prevention Infection prevention practices are based on the following five principles: 1. Every person (client or staff) is considered potentially infectious. 2. Hand washing is the single most important practice for preventing crosscontamination. 3. Wear gloves before touching anything wet—broken skin, mucous membranes, blood, or other body fluids. 4. Use protective gear (aprons, face masks, eye goggles) when splashes or spills of body fluids are expected. 5. Use safe work practices (e.g., do not recap or bend needles), following guidelines for handling and cleaning instruments and disposing of sharps and medical waste. Hand washing The steps in hand washing are: 1. Wet hands with running water and apply soap. 2. Rub together all surfaces of the hands including wrists, between fingers, palms, the back of the hands, and under fingernails. 3. Wash for 15 seconds. 4. Rinse under a stream of running water. 5. Dry hands. Air dry, or use a clean cloth or paper towels. Always wash hands: Upon arrival to and before leaving the health care facility. Before and after examining the woman or baby (or having any direct contact). After exposure to any blood or body fluids, even if gloves are worn. After removing gloves (the gloves may have very small holes). Gloves Wear gloves when: Performing a procedure. Handling soiled items (e.g., instruments and gloves). Disposing contaminated waste. A separate pair of gloves must be used for each woman to avoid cross-contamination. Prevention of Postpartum Hemorrhage: Implementing Active Management of the Third Stage of Labor 3 Disposable gloves are preferred, but when resources are limited, surgical gloves can be reused if they are: Decontaminated by soaking in 0.5 percent chlorine for 10 minutes AND Washed and rinsed AND Sterilized by autoclaving or high-level disinfected by boiling or steaming. Single-use or disposable surgical gloves should not be reused more than three times because invisible tears may occur. Note: Do not use gloves that are cracked, peeling, visibly torn, or contain holes. Aprons or gowns Wear a clean or sterile gown during delivery: If the gown has long sleeves, gloves should be placed over the gown sleeve to avoid contaminating the gloves. Ensure gloved hands are held high above the level of the waist and do not come into contact with the gown. Handling sharp instruments Do not leave sharp instruments or needles (“sharps”) in places other than “safe” zones: Use a tray or basin to carry and pass sharp items. Pass instruments with the handle (not the sharp end) pointing toward the receiver. Announce to others before passing sharps. Needles and syringes Follow these guidelines to ensure safe handling of needles and syringes: Use each needle and syringe only once. Do not recap, bend, or break needles before disposal. Dispose of needles and syringes in a puncture-proof container. Do not take needle and syringe apart after use. Where disposable needles are not available and you must recap the needle, use the “one-hand technique” for recapping (Figure 24).35 Step 1: Place the cap on a hard, flat surface. Step 2: Hold the syringe with one hand and use the needle to “scoop up” the cap. Step 3: When the cap covers the needle completely, hold the base of the needle and use 4 Figure 24. One-hand technique for needle recapping Prevention of Postpartum Hemorrhage: Implementing Active Management of the Third Stage of Labor Reference manual the other hand to make sure the cap is firmly in place. Preventing splashes Wear appropriate protective goggles, gloves, and gown during delivery. Prevent splashes from blood or amniotic fluid by following these guidelines: Avoid snapping the gloves when removing, as this may cause contaminants to splash into the eyes, mouth, or on to skin or others. Hold instruments and other items under the surface of the water while scrubbing and cleaning to avoid splashing. Place items gently into the decontamination bucket to avoid splashes. Avoid rupturing membranes during a contraction. Stand to the side when rupturing membranes to avoid splashes from amniotic fluid. Caution: If blood or body fluids get in the mouth or on skin, wash with liberal soap and water as soon as it is safe for the woman and baby. If blood or body fluids splash in your eyes, irrigate well with water. Waste disposal The purpose of waste disposal is to: Prevent the spread of infection to people who handle the waste. Prevent the spread of infection to the local community. Protect those who handle waste from accidental injury. There is no risk from non-contaminated waste such as office paper, which can be disposed of according to local guidelines Proper handling of contaminated waste (such as items with blood or body fluids) is required to minimize the spread of infection to other staff and the community. Proper handling includes: Wearing heavy-duty gloves. Transporting solid contaminated waste to the disposal site in covered containers. Carefully pouring liquid waste down a drain or flushable toilet. Burning or burying contaminated solid waste. Washing hands, gloves, and containers after disposal of infectious waste. The steps of processing instruments Proper processing involves several steps that reduce the risk of transmitting infections from used instruments and other items to health care workers and clients: 1) decontamination, 2) cleaning, 3) either sterilization or high-level disinfection, and 4) storage. For proper processing, it is essential to perform the steps in the correct order. Table 6 provides an overview of the benefits gained by performing each step when processing instruments and gloves. Prevention of Postpartum Hemorrhage: Implementing Active Management of the Third Stage of Labor 5 Table 6. Steps and benefits for processing instruments for reuse Processing step Benefit Step 1 Step 2 Decontaminate Clean High-level disinfect Step 3 Sterilize Step 4 Store or Use Kills viruses (hepatitis B and C, HCV, HIV) and many other germs. Makes items safer to handle during cleaning. Makes items easier to clean. Common decontamination process: soak in 0.5% chlorine solution for 10 minutes. Removes blood, other body fluids, tissue, and dirt. Reduces the number of germs. Makes sterilization or HLD effective. If blood clot remains on instrument, germs in clot may not be completely killed by sterilization or HLD. Wash items with soap and water and rinse with clean water. Kills all germs except some endospores. Use for items that have contact with broken skin or intact mucous membranes. If sterilization is not possible, HLD may be the only other choice. Can be done by boiling or steaming items for 20 minutes or chemical disinfection using 0.1% chlorine solution for 20 minutes. Kills all germs including endospores. If items are stored properly they will not become contaminated after processing. Proper storage is as important as proper processing. Store or use items properly after completing the first three steps to prevent contamination for up to one week in HLD container. May not be possible in all settings. Can be done by dry (oven) or wet heat (autoclave). HLD High-level disinfection 6 Prevention of Postpartum Hemorrhage: Implementing Active Management of the Third Stage of Labor Reference manual Making a chlorine decontamination solution The ability to decontaminate instruments is a critical step in infection prevention. The most common decontamination process is to soak instruments in a 0.5% chlorine solution for 10 minutes. Chlorine solutions made from sodium hypochlorite are usually the most inexpensive, fast-acting, and effective for decontamination. A chlorine solution can be made from: Liquid household bleach (sodium hypochlorite). Chlorine-releasing tablets (sodium dichloroisocyanurate).30 Bleach powder or chlorine compounds available in powder form (calcium hypochlorite or chlorinated lime). Chlorine-containing compounds contain a certain percentage of "active" (or available) chlorine. Active chlorine in these products kills microorganisms. The amount of active chlorine is usually described as a percentage and differs among products, an important fact to ensure preparation of a chlorine solution with 0.5 percent "active" chlorine that can be used to decontaminate gloves, instruments, etc. Note that: Different products may contain different concentrations of available chlorine and the concentration should be checked before use. In countries where French products are available, the amount of active chlorine is usually expressed in "degrees chlorum." One degree chlorum is equivalent to 0.3 percent active chlorine. Household bleach preparations can lose some of their chlorine over time. Use newly manufactured bleach if possible. If the bleach does not smell strongly of chlorine it may not be satisfactory for the purpose and should not be used; Thick bleach solutions should never be used for disinfection purposes (other than in toilet bowls) as they contain potentially poisonous additives. When preparing chlorine solutions for use note that: Because of their low cost and wide availability, chlorine solutions prepared from liquid or powdered bleach are recommended. Organic matter destroys chlorine, and freshly diluted solutions must therefore be prepared whenever the solution looks as though it needs to be changed (such as when it becomes cloudy or heavily contaminated with blood or other body fluids). Chlorine solutions gradually lose strength, and freshly diluted solutions must therefore be prepared daily. Calculate the ratio of water to liquid bleach, bleach powder, or chlorine-releasing tablets (see the calculations below) Clear water should be used to make the solution because organic matter destroys chlorine. Use plastic containers for mixing and storing bleach solutions as metal containers are corroded rapidly and also affect the bleach. Prepare bleach solutions in a well ventilated area because they give off chlorine. Label the container with “___ (o.1 or 0.5) percent chlorine decontamination solution,” and note the day and time prepared. Prevention of Postpartum Hemorrhage: Implementing Active Management of the Third Stage of Labor 7 0.5% bleach solution is caustic. Avoid direct contact with skin and eyes. Calculating the water to liquid household bleach ratio to make a 0.5% chlorine solution Chlorine content in liquid bleach is available in different concentrations. You can use any concentration to make a 0.5 percent chlorine solution by using the following formula: [% chlorine in liquid bleach divided by 0.5%] minus 1 = parts of water for each part bleach Note: "Parts" can be used for any unit of measure (e.g., ounce, liter, or gallon) and do not have to represent a defined unit of measure (e.g., pitcher or container). For example: To make a 0.5 percent chlorine solution from a 3.5 percent chlorine concentrate, use one part chlorine and 6 parts water: + [3.5% divided by 0.5%] minus 1 = [7] minus 1 = 6 parts water for each part chlorine Calculating the water to bleach powder ratio to make a 0.5% chlorine solution When using bleach powder to make a decontamination solution, calculate the ratio of bleach to water using the following formula: [% chlorine desired divided by % chlorine in bleach powder] times 1,000 = grams of powder for each liter of water. Note: When bleach powder is used, the chlorine solution will likely appear cloudy or milky. For example: To make a 0.5 percent chlorine solution from calcium hypochlorite powder containing 35 percent available chlorine, use the following formula: [0.5% divided by 35%] times 1,000 = [0.0143] times 1,000 = 14.3 Therefore, dissolve 14.3 grams of calcium hypochlorite powder in one liter of water in order to get a 0.5 percent chlorine solution. Calculating the water to chlorine-releasing tablet ratio to make a 0.5% chlorine solution Follow the manufacturer's instructions when using chlorine-releasing tablets because the percentage of active chlorine in these products varies. If instructions are not available with the tablets, ask for the product instruction sheet or contact the manufacturer. Table 7 provides details on how to mix a decontamination solution with chlorine. 8 Prevention of Postpartum Hemorrhage: Implementing Active Management of the Third Stage of Labor Reference manual Table 7. Mixing a 0.5 percent chlorine decontamination solution29 Liquid bleach (sodium hypochlorite solution) Type or brand (by country) % or grams active chlorine Water to chlorine = 0.5% solution 8º Chlorum* 2.4% 10 ml bleach in 40 ml water. 1 part bleach to 4 parts water. JIK (Kenya, Zambia), Robin Bleach (Nepal) 3.5% 10 ml bleach in 60 ml water. 12º Chlorum 3.6% 1 part bleach to 6 parts water. Household Bleach (Indonesia, USA), ACE (Turkey), Eau de Javel (France) 5% 10 ml bleach in 90 ml water. 1 part bleach to 9 parts water. 15º Chlorum, Lejia (Peru), Blanquedor, Cloro (Mexico) 6% 10 ml bleach in 110 ml water. 1 part bleach to 11 parts water. Lavandina (Bolivia) 8% 10 ml bleach in 150 ml water. 1 part bleach to 15 parts water. Chloros (United Kingdom) 10% 10 ml bleach in 190 ml water. 1 part bleach to 19 parts water. Chloros (United Kingdom), Extrait de Javel (France), 48º Chlorum 15% 10 ml bleach in 290 water. 1 part bleach to 29 parts water. % or grams active chlorine Water to chlorine = 0.5% solution Dry powders Type or brand (by country) Calcium hypochlorite 70% 7.1 grams per liter. Calcium hypochlorite 35% 14.2 grams per liter. Sodium dichloroisocyanurate (NaDCC) 60% 8.3 grams per liter. Tablets Type or brand (by country) Chloramine tablets* Sodium dichloroisocyanurate (NaDCC-based tablets) % or grams active chlorine 1 gram chlorine per tablet. 1.5 grams chlorine per tablet. Water to chlorine = 0.5% solution 20 grams per liter (20 tablets per liter). 4 tablets per liter. *Chloramine releases chlorine slower than hypochlorite. Before using solution, be sure the tablet is completely dissolved. Prevention of Postpartum Hemorrhage: Implementing Active Management of the Third Stage of Labor 9 10 Prevention of Postpartum Hemorrhage: Implementing Active Management of the Third Stage of Labor Reference manual References JHPIEGO. Infection Prevention Learning Resource Package [CD-ROM]. Baltimore, MD: JHPIEGO; 2004. 33 EngenderHealth. Online course for Infection Prevention. Available at: www.engenderhealth.org/IP/ instrum/in4a.html. Accessed April 2, 2007. 34 World Health Organization (WHO). Managing Complications in Pregnancy and Childbirth. Geneva: WHO; 2000. Available at: http://www.who.int/reproductive-health/impac/Clinical_Principles/ General_care_C17_C22.html. Accessed April 2, 2007. 32 World Health Organization and the US Centers for Disease Control and Prevention in partnership with the Francois-Xavier Bagnoud Center at the University of Medicine & Dentistry of New Jersey (UMDNJ) and JHPIEGO. Infection Prevention Guidelines for Healthcare Facilities with Limited Resources. Baltimore, MD: JHPIEGO; 2003. Available at: www.womenchildrenhiv.org/wchiv?page=pi60-00. Accessed April 2, 2007. 35 Prevention of Postpartum Hemorrhage: Implementing Active Management of the Third Stage of Labor 11