NEONATAL PSEUDOHYPOALDOSTERONISM TREATED WITH
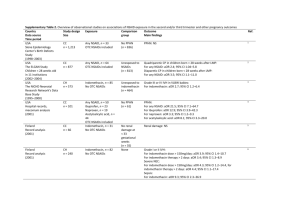
advertisement

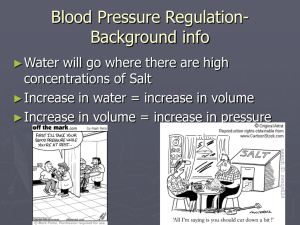
P45 NEONATAL PSEUDOHYPOALDOSTERONISM TREATED WITH INDOMETHACIN Wright IMR1, Cutfield W2 Departments of Neonatology1 and Paediatrics2, The University of Auckland, Private Bag 92019, Auckland, New Zealand. Neonatal pseudohypoaldosteronism (PHA), McKusick 264350, is a defect in the epithelial sodium channel mechanism of the aldosterone receptor. Aldosterone levels are markedly increased in blood and urine, usually with increased renin levels. There are frequent episodes of hypovolaemic shock, secondary to the severe diuresis, with a high mortality. We describe an infant with fulminant PHA in whom treatment with indomethacin resulted in a complete resolution of symptoms. Case Report: A male, non-consanguineous infant was born at 32 weeks gestation, following severe polyhydramnios from 23 weeks gestation. The infant was morphologically normal, normally grown and required no resuscitation. At 80 hours of age he had a cardiovascular collapse, secondary to salt wasting polyuria, requiring volume and salt replacement. PHA was diagnosed because of massive natriuresis and diuresis, mild hypertension, normal corticosteroid response, high aldosterone level and high renin level. Diuresis and natriuresis progressed until the baby was passing a volume of urine greater than his body weight (2500mLs) per day. Loss of central venous access for only 20 minutes led to hypovolaemic collapse. At thirty days of age, after full discussion with his parents, a trial of indomethacin, 3 mg/kg/day in three divided doses, was commenced. There was a dramatic response, with a reduction in urine output of approximately 80% within a few days. Urine output stabilised at 3-400 mL/day with a remaining oral sodium replacement of 3 mmols/kg/day. The indomethacin dose was gradually reduced, stopping at 62 days of age. Electrolytes remained normal with no recurrence of the diuresis. Sodium supplements were stopped at 2 months-corrected age. He is currently well, on no supplements or medication. Discussion: PHA has a variety of clinical presentations, but the presence of severe hypovolaemia and severe electrolyte disturbances in the neonate has been previously associated with a high infant mortality. Treatment has been sodium and water supplementation, until the gradual reduction in levels of salt wasting occurs, which may take up to 2 years. During this time the infant is at risk of hypovolaemic crises. In our case, an initial period of recovery was followed by further increase in salt wasting and fluid dependence. It is postulated that mechanism of this was increased kidney Prostaglandin E2 production, in response to the persistent diuresis. Primary hyperprostaglandin E syndromes may be controlled with the administration of long-term indomethacin. We considered it reasonable to use both the antiprostaglandin and renal blood flow effects of indomethacin, to treat this life threatening diuresis. Indomethacin has previously been used in older survivors of infantile PHA with hypercalciuria and nephrocalcinosis, but has not for early severe diuresis. We have demonstrated the use of indomethacin to allow control of torrential diuresis in an infant presenting with pseudohypoaldosteronism. This allowed time for the natural history of resolution of symptoms. As it is not clear at what stage the apparent hyperprostaglandin E symptoms occur in PHA, we do not know at what stage treatment would be most effective. If there is a significant contribution from prostaglandin E present in the polyuric fetus, then it may be possible to treat with maternal indomethacin. It may be that earlier use may have avoided several life-threatening events and we would suggest that this treatment be considered earlier in future cases, including possible antenatal use in confirmed cases.