EXAMPLE - Acusis
advertisement
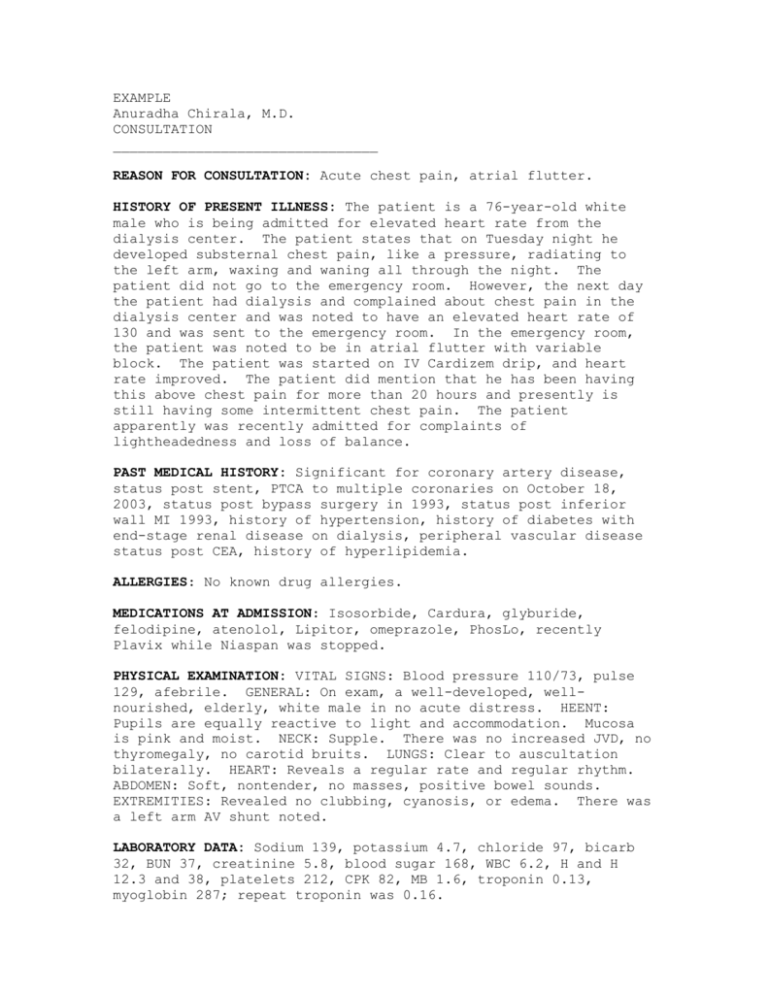
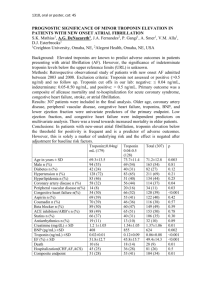
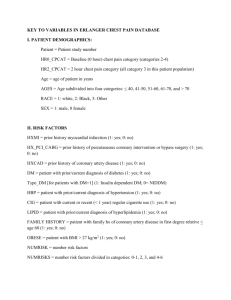
EXAMPLE Anuradha Chirala, M.D. CONSULTATION ________________________________ REASON FOR CONSULTATION: Acute chest pain, atrial flutter. HISTORY OF PRESENT ILLNESS: The patient is a 76-year-old white male who is being admitted for elevated heart rate from the dialysis center. The patient states that on Tuesday night he developed substernal chest pain, like a pressure, radiating to the left arm, waxing and waning all through the night. The patient did not go to the emergency room. However, the next day the patient had dialysis and complained about chest pain in the dialysis center and was noted to have an elevated heart rate of 130 and was sent to the emergency room. In the emergency room, the patient was noted to be in atrial flutter with variable block. The patient was started on IV Cardizem drip, and heart rate improved. The patient did mention that he has been having this above chest pain for more than 20 hours and presently is still having some intermittent chest pain. The patient apparently was recently admitted for complaints of lightheadedness and loss of balance. PAST MEDICAL HISTORY: Significant for coronary artery disease, status post stent, PTCA to multiple coronaries on October 18, 2003, status post bypass surgery in 1993, status post inferior wall MI 1993, history of hypertension, history of diabetes with end-stage renal disease on dialysis, peripheral vascular disease status post CEA, history of hyperlipidemia. ALLERGIES: No known drug allergies. MEDICATIONS AT ADMISSION: Isosorbide, Cardura, glyburide, felodipine, atenolol, Lipitor, omeprazole, PhosLo, recently Plavix while Niaspan was stopped. PHYSICAL EXAMINATION: VITAL SIGNS: Blood pressure 110/73, pulse 129, afebrile. GENERAL: On exam, a well-developed, wellnourished, elderly, white male in no acute distress. HEENT: Pupils are equally reactive to light and accommodation. Mucosa is pink and moist. NECK: Supple. There was no increased JVD, no thyromegaly, no carotid bruits. LUNGS: Clear to auscultation bilaterally. HEART: Reveals a regular rate and regular rhythm. ABDOMEN: Soft, nontender, no masses, positive bowel sounds. EXTREMITIES: Revealed no clubbing, cyanosis, or edema. There was a left arm AV shunt noted. LABORATORY DATA: Sodium 139, potassium 4.7, chloride 97, bicarb 32, BUN 37, creatinine 5.8, blood sugar 168, WBC 6.2, H and H 12.3 and 38, platelets 212, CPK 82, MB 1.6, troponin 0.13, myoglobin 287; repeat troponin was 0.16. DIAGNOSTIC DATA: EKG revealed atrial flutter with variable block, LVH with secondary ST-T changes and intraventricular conduction defect. IMPRESSION: 1. We have a 76-year-old who presents with new onset atrial flutter, most likely secondary to ischemia. 2. Chest pain secondary to acute coronary artery syndrome in view of elevated troponin. 3. Coronary artery disease status post stents, myocardial infarction, and bypass. 4. Hypertension, diabetes, end-stage renal disease on dialysis, hyperlipidemia, peripheral vascular disease. RECOMMENDATIONS: The patient continues to have intermittent chest pain and, in view of increasing troponin, I recommend to consider transferring the patient to ICU. The patient’s heart rate is not controlled with a heart rate in the 120s and 130s presently. I recommend transfer to ICU for IV Cardizem. We will also start patient on IV nitroglycerin for chest pain. Recommend an echo Doppler to assess LVEF. Recommend to start patient on aspirin 81 mg, Lovenox 30 subcutaneous b.i.d. Continue the atenolol for now. Recommend to hold Lasix. Once rate is controlled, will perform a TEE, followed by electrical cardioversion. If no resolution of chest pain and increasing troponin, will consider transfer for emergent catheterization.