The Gravedigger`s Guide to Cardiology
advertisement
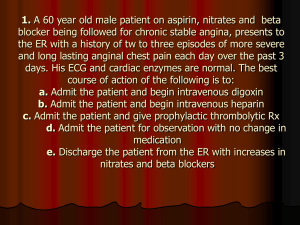
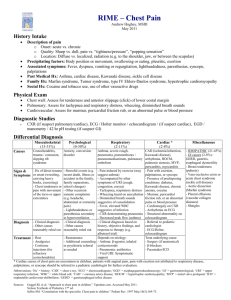
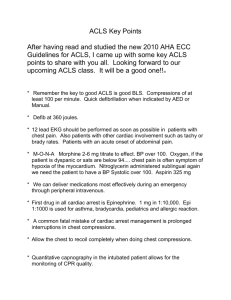
The Gravedigger’s Guide to Cardiology Overview TOC The Evaluation of Chest Pain ................................................................................................................. 2 TIMI SCORE (Thrombolysis in Myocardial Infarction) ....................................................................... 3 Non-ST Elevation Acute Coronary Syndrome ....................................................................................... 3 ST-Elevation Acute Coronary Syndrome ............................................................................................... 6 Reperfusion Therapy .............................................................................................................................. 8 STEMI/NSTEMI Discharge ................................................................................................................ 10 Mechanical Complications of AMI ...................................................................................................... 11 AMI Arrhythmias ................................................................................................................................. 12 Characeristics of MIs ............................................................................................................................ 14 Cardiogenic Shock................................................................................................................................ 15 Intraaortic balloon pump counterpulsation ........................................................................................... 15 Acute Heart Failure .............................................................................................................................. 16 Hypertrophic Cardiomyopathy ............................................................................................................. 17 Restrictive Cardiomyopathy ................................................................................................................. 18 Constrictive Pericarditis ....................................................................................................................... 18 Hyperensive Crisis................................................................................................................................ 18 Radiation-Induced Cardiac Injury ........................................................................................................ 20 Endocarditis .......................................................................................................................................... 20 Mitral Valve Prolapse ........................................................................................................................... 20 Mechanical Valves ............................................................................................................................... 21 Aortic Dissection .................................................................................................................................. 22 Congestive Heart Failure ...................................................................................................................... 22 Bradyarrhythmias ................................................................................................................................. 24 Tachyarrhythmias ................................................................................................................................. 27 Atrial Fibrillation .................................................................................................................................. 29 Atrial Flutter ......................................................................................................................................... 29 Permanent Pacemakers and AICDs ...................................................................................................... 30 Pregnancy Related Cardiology ............................................................................................................. 31 Contrast Nephropathy ........................................................................................................................... 31 Stopping Medications Before Interventions ......................................................................................... 31 Complications of Cardiac Catheterization............................................................................................ 32 Secondary Prevention of CAD at Strong.............................................................................................. 33 Pulmonary Hypertension ...................................................................................................................... 33 Cardiology Trials .................................................................................................................................. 34 ACS ECG Interpretation....................................................................................................................... 34 Cardiac Monitoring and Normal Values .............................................................................................. 35 Laboratory Values ................................................................................................................................ 35 Pharmacology of Inotropes and Vasoactive Medications .................................................................... 36 Cardiac Medications ............................................................................................................................. 39 Ward Lessons ....................................................................................................................................... 41 Patient Checklist ................................................................................................................................... 42 Physical Exam ...................................................................................................................................... 43 Admission Notes .................................................................................................................................. 43 Admission Orders ................................................................................................................................. 43 ACS algorithm ...................................................................................................................................... 53 Orders Set Examples ............................................................................................................................ 53 1 The Evaluation of Chest Pain Rapid Evaluation HPI o Chest discomfort type, location, quality, radiation, duration o Associated symptoms such as nausea, vomiting, diaphoresis, dyspnea, dizziness PMH o Known CAD o Diabetes – assume cardiac disease until proven otherwise o HTN o HLD o Cigarette smoking o Stroke/TIA o PVD o Obesity o Poor physical conditioning Physical Exam o Pulmonary congestion o Tachy or brady o Irregular pulse o S3 or S4 o Listen to carotids and femorals for bruits o Check leg pulses Workup o ECG – 1mm or more elevation in two contiguous leads or new LBBB (compare to an old one) Treatment Call cardiac fellow or page office for “Acute MI team” Start large 1-2 large bore IVs (18-20) guage and start saline IV at KVO Draw stat labs including CPK and isoenzymes Start O2 by nasal cannula NTG (SL or paste) Obtain cath consent Morphine or fentanyl in small doses to relieve pain and anxiety ASA 325mg Anterior MI o Metoprolol 5 mg IV x3 doses approximately 5 minutes apart to total of 15 mg IV. Watch for hypotension or bradycardia. May decide to avoid beta blocker in CHF, LV failure Inferior MI o Do not routinely use beta blocker 2 TIMI SCORE (Thrombolysis in Myocardial Infarction) Non-ST Elevation Acute Coronary Syndrome Definitions Unstable Angina: new angina or departure from previous pattern of angina without ECG changes or biomarker changes NSTEMI: non-Q wave myocardial infarction (biomarker changes) Pathophysiology ACS result from an imbalance between oxygen supply and demand. Either ventricle may be involved but the left ventricle is at higher risk for ischemia due to its greater muscle mass and greater afterload. Factors which may decrease oxygen delivery o Coronary atherosclerosis o Coronary artery vasospasm o Plaque rupture and thrombosis o Anemia o Hypoxemia o Limited diastolic filling time (tachycardia) o Hypotension Factors with may increase oxygen demand o Tachycardia and/or increased metabolic demands (i.e. infection, hyperthyroid) o Heightened LV afterload causing increased transmural wall tension HTN LV cavity dilation Aortic dissection PE or pulmonary HTN in right heart 3 o Increased LV mass (hypertrophy) o Increased contractility Diagnosis History and physical o Substernal tightness, heaviness, squeezing o Autonomic manifestations (nausea, vomiting, diaphoresis) are signs of instability Data o ECG ST elevation or depression T-wave flattening or inversion PVCs Conductive disturbance Normal ECG in up to 15% of those with UA 70% of all ECG documented episodes of ischemia are clinically silent o Cardiac Enzyme Markers Increased trop I/T Increased highly sensitive CRP (hsCRP) Prognostic Factors Short-term mortality o UA: 2-3% o NSTEMI: 5-7% o STEMI: 6-9% Long-term mortality o NSTEMI: 10-12% o STEMI: 9-11% Treatment Algorithm Initial management for unstable angina/NSTEMI ASA (high dose) Heparin or enoxaparin o LMWH is better than UFH BB o Decreases demand and progression to AMI o No decrease in mortality in NSTEMI Nitrates Possibly Glycoprotein Iib/IIIa inhibitor (abciximab) o Decreased mortality, increased bleeding o Most suited for high-risk patients o Give if TIMI 3-4 or above Recurrent angina Elevated Troponin 4 New ST depression Signs or symptoms of congestive heart failure Prior bypass grafting PCI within 6 months Sustained ventricular tachycardia Hemodynamic instability o Has been shown to be beneficial only in those who will undergo PCI and may have increased mortality in those who do not o If no clear indication for PCI a small molecule such as eptifibitide or tirofiban is often selected Clopidogrel o Usually indicated o Hold if angiography is planned within 24 to 36 hours of presentation o Hold if possible CABG PCI? o Low TIMI risk score (0-2) No further meds Stress testing for ischemia and risk stratifications o High TIMI (5-7) Give glycoprotein IIb/IIIa inhibitor Stabilize for coronary angiography o Intermediate TIMI (3-4) and no high risk markers Can undergo stress testing and risk stratification before angiography Cath if Recurrent angina/ischemia at rest or with low-level activities despite medication therapy Elevated Troponin Recurrent angina/ischemia with symptoms of heart failure LVEF < 40% Sustained ventricular tachycardia PCI within 6 months Prior CABG Ischemia during provocative test Reasoning Reduce demand (decrease HR and afterload) o Limit physical activity (bedrest) o Control arrhythmias o Control HTN Increase oxygen supply o Increase hemoglobin saturation or concentration o Nitroglycerin Titrate to relieve chest pain and decrease BP 10-20% o Calcium-channel blockers Revere coronary vasospasm Be careful of preload dependence Antiplatelet Therapy o ASA 325 mg qdaily RISC trial found to reduce the risk of death and acute MI by ~50% in patients with NSTE-ACS 5 Decreases risk of recurrent events by 25% ASA resistance in 5-10% of patients Thienopyridines (Ticlopidine and Clopidogrel) o Evidence Glycoprotein 2b/3a Receptor Inhibitors o Evidence o Large-molecule agents Preferred for PCI with STEMI Continue 12 hours post PCI If CABG is required D/c medication Give 6-12 units platelet transfusion o Small-molecule agents Used with ASA and heparin Initial stabilization of NSTE-ACS Dosing: initial bolus with infusion for 24-72 hours Most beneficial for those at high risk Continue for 12-24 hours post coronary intervention If CABG, d/c at least 4-6 hours prior Antithombotic Therapy o Unfractionated Heparin Heparin Sliding Scale Bolus 60 U/kg Cont infusion at 12 U/kg/hr Continue until revascularization or for 3-5 days if none planned o Low-Molecular Weight Heparin Direct Thombin Inhibitors o Only recommended for those with HIT Fibrinolytic Therapy o May be deleterious in NSTE-ACS ST-Elevation Acute Coronary Syndrome “often troponins are the tip of the iceberg…” Management Strategies for patients with STEMI 1. Quickly screen patients for indication and risk 2. Start thrombolytic therapy or send patient to cardiac catheterization lab for emergency angioplasty and stenting 3. Open the infarct-related artery and its distal microvasculature with minimal incidence of stroke by the fastest and most effective way 4. Prevent left ventricular remodeling (no left ventricular dilation) 5. Prevent another MI in the future (secondary prevention) Factors suggestive of high risk patients 1. Hypotension (SBP < 100) 2. Congestive Heart Failure 3. Sinus Tachycardia (HR > 100) 4. Advanced Age 5. Female Sex 6. Diabetes Mellitus 7. Persistent ST Segment Elevation 6 8. Persistent Chest Pain 9. High BNP Level 10. Anemia 11. High WBC 12. Chronic Kidney Disease The risk of dying within the next 24 hours is low if the SBP is greater than 100 and the HR is less than 100 (but greater than 50 because this may be a sign of an AV block). Thrombolytic Therapy Indications Patient presents for chest discomfort < 12 hours after symptom onset Chest discomfort and ST-segment elevation of at least 1 mm in at least two limb leads and 2mm in 2+ contiguous precordial leads New LBBB Contraindications Absolute o Any prior intracranial bleeding o Known structureal cerebral vascular lesion (AV malformation) o Known malignant intracranial neoplasm o Ischemic stroke within 3 months except ischemic stroke within 3 hours o Active bleeding or bleeding diathesis (excluding menses) o Significant closed head or facial trauma within 3 months Relative Contraindications o History of chronic, severe, or poorly controlled hypertension o Severe uncontrolled HTN on presentation (SBP > 180 mmHg, DBP > 110 mmHg) o History of prior ischemic stroke > 3months o Traumatic CPR (> 10 minutes) or major surgery (< 3 weeks) o Non-compressive vascular puncture o For streptokinase/anistrepplase: prior exposure (more than 5 days ago) or prior allergic reaction to these agents o Active peptic ulcer o Current use of anticoagulants: the higher the INR, the high the risk of bleeding Primary Coronary Intervention Exclusion Criteria 1. Unprotected LM lesion > 60% 2. Infarct-related artery with TIMI 3 flow and lesion morphology extremely high risk for abrupt closure (extremely long or severe angulated lesion) 3. Multivessel disease with TIMI-3 flow in infarct-related artery, now stable and pain free 4. Infarct-related artery supplies a small or secondary vessels supplying a small amount of myocardium, risk may outweigh benefit 5. Inability to clearly identify infarct-related artery Fibrinolytic Therapy o Fibrinolysis should resolve chest pain and ECG changes o Indications Pt presents < 12 hours after symptom onset If transfer to cath lab (at another hospital > 2 hr) unless Contraindication 7 STEMI > 12 hours after onset with residual ST-segment elevation STEMI with hsf CABG Cardiogenic shock o Give within 30 minutes of arrival in the ED o 60-75% reperfusion rate Catheterization o 90-95% reperfusion rate Reperfusion Arrhythmias o Usually a transient accelerated idioventricular arrhythmia o Usually do not require therapy Medical Management o ASA o Beta-blocker o Statin o ACEI o Thienopyridines (Ticlopidine and Clopidogrel) Clopidogrel is a reasonable alternative to aspirin for patients with contraindications to aspirin, but there is no benefit of adding clopidogrel to aspirin therapy in the management of acute myocardial infarction. o Glycoprotein IIb/IIIa blocker An intravenous glycoprotein IIb/IIIa blocker in addition to aspirin and heparin is indicated for patients with continuing ischemia, an elevated troponin level, or with other high-risk features, including angina at rest with ST-segment changes, congestive heart failure, diabetes, or patients in whom catheterization and percutaneous intervention are planned Glycoprotein receptor blockade with such agents as eptifibatide is indicated for patients with acute coronary syndrome who will undergo coronary angiography and intervention. Early treatment likely improves outcomes of percutaneous coronary intervention. Reperfusion Therapy Goals: Early patency of the infarct-related artery with improved ventricular remodeling, electrical stability and myocardial salvage Shortest time to treatment o Lytics: <30 minutes o PCI: <90 minutes door to balloon Thrombolytics Administration Dose Streptokinase Bolus and infusion 1.5 million units over 30-60 minutes TPA Bolus and infusion 15 mg bolus, then 0.75 mg/kg for 30 min, then 0.5 mg/kg over 60 minutes (max dose <= 100 mg) Reteplase Double bolus Tenectaplase Single bolus Two 10 mg boluses given 30min apart Single bolus of 0.5 mg/kg (range 30-50 mg) 8 Half-life (min) IV heparin required 23-29 No 4-8 Yes 15 Yes 20 Yes Mechanism of Action Conversion of plasminogen to plasmin which promotes degradation of fibrin clot Streptokinase has a more systemic lytic effect and is highly antigenic and can only be administered once Adjunctive Agents Heparin: Bolus of 60U/kg (maximum 4000Units) followed by a 12U/kg/hr infusion (goal aPTT 50-70 seconds) Aspirin: improves efficacy of all lytics Indications Typical chest pain for >30 minutes but <12 hours, relieved by sublingual NTG AND ST segment elevation in >= 2 contiguous leads o >=1 mm in limb leads o >= 2 mm in precordial leads OR ST depression in only V1 and V2 or >= 2 mm OR New LBBB Contraindications Major Any previous history of hemorrhagic stroke Stroke, dementia or CNS damage with 1 year Head trauma or brain surgery within 6 months Known intracranial neoplasm Suspected aortic dissection Internal bleeding within 6 weeks Active bleeding or know bleeding disorder Major surgery, trauma, or bleeding within 6 weeks Traumatic CPR within 3 weeks (brief CPR is not a contraindication) Relative Oral anticoagulant therapy Acute pancreatitis Pregnancy, or within 1 week postpartum Active peptic ulceration Transient ischemic attack within 6 months Dementia Infective endocarditis Active cavitating tuberculosis Advanced liver disease Intracardiac thrombi Uncontrolled hypertension (SBP > 180 or DBP > 110) Puncture of noncompressible blood vessel within 2 weeks 9 Factors which are not contraindications Menstruation Non-traumatic CPR lasting < 10 minutes Diabets Post-Lytic Management 1. Has myocardial reperfusion occurred? a. Complete or partial restoration of flow only occurs in 50-60% and rescue angiography may need to be performed b. Evaluation i. Symptoms: Has the patient’s chest discomfort resolved or abated substantially? ii. ECG: Has the degree of ST elevation improved by >50% iii. Reperfusion arrhythmias: has accelerated idioventricular rhythm or sinus bradycardia occurred in concert with symptoms and ECG improvements? iv. Hemodynamics: Is the patient hemodynamically stable? 2. Is there vessel reocclusion? a. Up to 20% of patient may reocclude the vessel with the first few hours b. Evaluation i. Symptoms: resurge of symptoms ii. ECG: worsening of ECG 3. Hemorrhagic complications a. Risk of major bleed with fibrin-selective agents (non-streptokinase) is 1.5-2% b. Intracranial hemorrhage has a 50% mortality i. New-onset HA, seizure, visual disturbance, new focal neuro deficit ii. Order stat head CT and rapid neurosurgical consult iii. Reversal of anticoagulant agents c. GI bleed i. Less common ii. Aggressive supportive treatment Catheterization Patients may have pain post plasty. This can be due to embolic spasm and may be relieved by imdur Bleeding from site Sandbag Call Interventional Fellow May need norepinephrine injection at site STEMI/NSTEMI Discharge Medications o BB o ASA o Plavix 9 months if no stent 1 month post BMS 1-2 years post DES o DM control o Statin o ACEI if CHF 10 Non-medications o Exercise o Smoking cessation o Nutrition/DM planning Mechanical Complications of AMI Essentially all mechanical complications are due to anatomic rupture of infracted tissue. There are 3 subtypes: 1. LV free-wall rupture (RV rupture is very rare) 2. Interventicular septal wall rupture 3. Papillary muscle rupture or dysfunction LV free-wall rupture Type I (slit-like rupture) o Early (within 24 hours) o Anterior MI, single vessel disease Type II (erosion of myocardium) o Early (within 24 hours) o Posterior infarct, multi-vessel disease Type III o Later (after 24 hours) o Large anterior MIs o Severely expanded and thinned myocardium o May by sealed off by pericardium to form a pseudoaneurysm Diagnosis Acute form Beck’s triad Elevated systemic venous pressure Systemic arterial hypotension Small quiet heart Frequently decompensated into EMD or asystole leading to cardiac death Subacute form (tamponade) Transient hypotension Syncope Transient EMD Bradycardia Nausea and agitation ECG with persistent and diffuse ST elevation Echo with effusion, RV/RA compression, “shaggy” intrapericardial echo densitites Management Decompensating patient o Early pericardiocentesis to relieve tamponade Stable o Open surgical drainage Interventricular Septal Rupture First week post-MI in 1-3% of all Mis Results in shunt from left to right heart 11 Clinical Presenation o RV overload o Cardiogenic shock o New load pansystolic murmur with thrill Diagnosis o Echo o Right-heart cath (increased RV oxygen sat) Management o Stabilize Diuretics, vasodilators, inotropes IABP PPV o Surgical repair Acute Papillary Muscle Rupture or Dysfunction Clinical Presentation o Usually 2-7 days after MI o Sudden Onset CHF and/or hypotension o Short systolic murmur in the apical area Management o Temporizing measures Diuretics, vasodilators, intermittent PPV IABP o Surgery AMI Arrhythmias Ventricular Premature Beats A conservative approach is taken to management as their was an increase in mortality with treatment in the CAST and SWORD trials. Correct underlying electrolyte and metabolic disturbances. Treatment only if hemodynamic compromise or serious arrhythmia Ventricular Tachycardia Accelerated Idioventricular Tachycardia Ventricular Rhythm with a rate between 60-125 Usually resolves spontaneously Treat if hemodynamic compromise, increased myocardial oxygen requirement, predisposition to more lethal arrhythmias Treat: overdrive the rhythm with a pacemaker or atropine Non-Sustained and Sustained Ventricular Tacycardia NSVT Definition 3+ ectopic ventricular beats Rate > 120 BPM Lasts less than 30 seconds 12 Classify as monomorphic or polymorphic Monomorphic Thought to be related to myocardial scarring Tx: Require long term anti-arrhythmic and/or AICD Polymorphic May be related to ongoing ischemia Tx: Resolve ischemia (cardiac cath, anticoagulation, decrease myocardial O2 demand) Sustained Venticular Tachycardia Sustained polymorphic V-tach within 48 hours postMI are associated with a hospital mortality of 20% Treat if HD compromise or HR > 150: Cardioversion Correct electrolytes Anti-arrhythmics (lidocaine, procainamide, amiodarone) Ventricular Fibrillation Primary VF Occurs suddenly and unexpectedly in patients with no or few signs of LV dysfunction Occurs early after MI (within first 12 hours?) Secondary VF Occurs in patients with severe cardiogenic shock and LV dysfunction Bradycardia Most often seen early after infarct Likely due to increased vagal tone Most often seen in posterior and inferior MI Management often amounts to observation First 6 hour: if HR < 40 and has ventricular premature beats, give atropine in small doses After 6 hours: likely sinus node dysfunction or atrial ischemia rather than excessive vagal tone If hypotension does occur and the bradycardia is unresponsive to atropine, then a pacemaker is indicated Atrioventricular Block/Intraventricular Block First Degree Block Almost always 2/2 disturbance above bundle of His. Complete heart block can only occur in those with first degree block below the node. Consider stopping beta-blockers if PR interval becomes greater than .24 seconds Second Degree Block – Type I 10% of patients with AMI Usually in inferior MI Usually transient, resolving 3 days post infarction) No treatment required unless other blocks also present or excessively slow rate 13 Second Degree Block – Type II Usually develops below the bundle of His with a widened QRS Block can progress suddenly to complete AVB and asystole Treatment: pacemaker placement Complete Block Inferior block – often slowly progressing through the various degrees of block, usually stable escapre rhythm, may be responsive to methylxanthine. May resolve spontaneously but mortality is high Anterior – sudden, ominous and dramatic. Patients have unstable, wide QRS complex escape rhythm, asystole can occur, Treatment: supportive care, pacemaker insertion RBBB 2% of MI Can lead to complete AVB LBBB 5% of MI High mortality because of amount of myocardial damage needed to produce a LBBB is large Paroxysmal Supraventricular Tachycardia (PSVT) Vagal maneuvers Adenosine (if not hypotension) AV slowing medications (CCB and BB) Atrial Fibrillation/Atrial Flutter Atrial Flutter – rare, usually transient Atrial Fibrillation – 10-15% in MI, may be marker of poor prognosis, treat with cardioversion, AV blocking meds, procainamide and amiodarone Characeristics of MIs Anterior MI 2nd degree block type II Complete heart block Interventricular septal rupture Type I and type III LV free-wall rupture Wait 72 hours before discharge due to higher complication rate 2/2 rhythms Anteroseptal MI RBBB Interventricular septal rupture Wait 72 hours before discharge due to higher complication rate 2/2 rhythms Posterior MI Type II LV free-wall rupture Inferior MI 2nd degree block type I Complete heart block 14 Cardiogenic Shock Diagnostic Criteria BP < 90 mm Hg, or a decrease in the MAP by > 30 mm Hg, for at least 30 minutes, not improved with fluid administration Signs of hypoperfusion (cold extremities), altered mental status (restlessness or agitation) Reduced urine output (<20 cc/hr) Cardiac index of < 2.2 L/min/m2 Management Strategy Overview Identify the patient with cardiogenic shock, even if the blood pressure is not yet low Revascularize the patient with a percutaneous or surgical approach Close follow-up and correct all non-cardiac problems such as respiratory, liver, kidney failure Management in the ED The presence of sinus tachycardia and borderline low BP (<100 mm Hg but >90 mm Hg) should trigger the process of investigating carefully the causes of declining BP. 1. Does the patient still have ongoing ischemia as evidenced by chest pain or angina-equivalent? 2. Are there any rales in the lung ausculatation, suggestive of LV failure with pulmonary congestion? 3. Does the patient have signs or peripheral hypoperfusion (cold extremities, agitation, restlessness, or low-urine output < 20mL/h) 4. Are there any signs of mechanical complications from AMI – new murmur of mitral regurgitation, muffled heart sounds of a pericardial effusion, VSD from ventricular septal rupture Work-up during pre-shock period 1. Frequent monitoring of HR and BP 2. Generous IV fluid challenge 3. Reassessment with ECG 4. STAT echocardiography 5. Comprehensive physical exam 6. Right heart catheterization Electrocardiogram Suspicion of early cardiogenic shock by ECG 1. Anterior wall MI or multisite MI with decreasing SBP (most common) 2. >20 mmHg decrease of BP in patient with history of prior MI 3. >20 mmHg decrease of BP in patient with inferior wall MI 4. Decreasing BP with clear lung due to right ventricular infarction Intraaortic balloon pump counterpulsation Indications for use: Cardiogenic shock Intractable angina Weaning patients from cardiopulmonary bypass Adjunctive therapy in high risk or complicated angioplasty Prophylaxis in patients with severe left main coronary artery stenosis or critical aortic stenosis in whom surgery is pending 15 Hemodynamic Effects A balloon pump works by sitting in the aorta and inflating during diastole and deflating during systole. Inflation during diastole generates a pressure wave causing blood to flow back into the coronary arteries. Deflation during systole generates a vacuum which reduces afterload. Decrease systolic pressure Increases diastolic pressure Reduces heart rate Decreases MCWP Elevates cardiac output Contraindications Aortic regurgitation or significant AV shunting Abdominal aortic aneurysm or aortic dissection Uncontrolled sepsis Uncontrolled bleeding disorder Severe bilateral peripheral vascular disease Bilateral femoral popliteal bypass grafts for severe PAD (can be carried out in patients with aortobifemoral bypass grafts) Complications Vascular Limb ischemia Vascular laceration necessitating surgical repair Major hemorrhage Arterial dissection with balloon placement into a false lumen NonVascular Cholesterol embolization (thrombocytopenia, livedo reticularis, eosinophilia) CVA if balloon migrates proximal to the left subclavian artery Sepsis (rare if used for less than 7 days) Balloon rupture Thrombocytopenia Hemolysis Groin infection Seroma Peripheral neuropathy Acute Heart Failure Clinical Presentation Physical exam: rales, JVP, S3, peripheral edema, weight gain CXR: pulmonary congestion Heart failure may be a much more difficult diagnosis in a person with chronic heart failure without evidence of pulmonary congestion on CXR or physical exam. The history is important and will always include: fatigue, DOE, PND What is the cause of the heart failure? Sodium intake/dietary changes Acute ischemia 16 Medication noncompliance NSAIDs Atrial fibrillation Initiation of beta-blocker therapy Management Dependent upon hemodynamic status Normal blood pressure and predominant fluid overload o Aggressive diuretic therapy Marginal blood pressure o Diuresis o Inotropes o Vasoactive medications Diuretics Lasix bolus Lasix gtt Indications o Better titration to effect Dosing o Bolus half of the usual outpatient dose o Infuse 5-20 mg/hr If there is no response a thiazide diuretic such as diuril, HCTZ or metolazone may augment response Aggressively replete electrolytes. Add acetazolamide (diamox) for extreme contraction alkalosis. Inotropes Empiric therapy with dobutamine/dopamine or milrinone Vasodilators Nitroprusside and nitroglycerin ACEI can be continued but may want to switch to short-acting (captopril) and decrease dose if also using dobutamine and hypotensive response may be greater B-Blockers Decrease beta-blockers or if inotropic support is needed (dobutamine) stop them completely. Hypertrophic Cardiomyopathy Treatments AICD: improves survival Septal myomectomy: improves symptoms of outflow obstruction Avoidance of stenuous exercise 17 Restrictive Cardiomyopathy Cardiac Amyloidosis Epidemiology Clinical Presentation Diagnosis ECG o Low voltage Echo o Increased wall thickness o Right sided heart failure with diastolic dysfunction with restrictive pattern Fat pad biopsy With the combination of a low voltage ECG and interventricular septal thickness is greater than 1.98 cm, the diagnosis of cardiac amyloidosis can be made with a sensitivity of 72% and a specificity of 91% Treatment Constrictive Pericarditis Epidemiology Mediastinal radiation therapy may result in cardiac disease 10-20 years later TB exposure Clinical Presentation Physical Exam Elevated jugular venous pressure Prominent x and y descents Kussmaul’s sign o Paradoxical increase in JVP with inspiration o Rarely seen Diagnosis CT Scan – direct visualization of pericardium Right and left heart catheterization o Would show equalization of diastolic pressures in all four chambers Treatment Pericardectomy o Definitive treatment o Surgical mortality is 6-19% Medical Mangement o Appropriate for those with minor symptoms o Edema Compression stockings Lasix can be cautiously started Patients are preload dependent Hyperensive Crisis Natural course of untreated hypertensive crises are renal failure, stroke, MI and death. 18 Hypertensive Emergency Diastolic pressure >130 mm Hg Evidence of end-organ damage o Group 3 or 4 retinopathy (hemorrhage or papilledema) o Cerebral edema or intracranial hemorrhage o Left ventricular dysfunction o Aortic dissection o Acute renal disease Hypertensive Urgency Diastolic pressure >120 mg Hg Lack of end-organ damage Fundoscopic changes can be seen o Changes Arteriolar narrowing Vasospasm AV crossing abnormalities o Definitions Acute damage to retinal vessels – accelerated malignant hypertension Retinal exudates – malignant hypertension Hypertensive Encephalopathy Clinical Presentation: HA, irritability, alteration in consciousness, central nervous dysfunction Therapy HTN Emergency o Goal: reduce MAP by 20% but not more than 25% in the first hour or the diastolic pressure to 100-110 over several hours o Medications Nitroprusside (DOC) 0.25-10 mcg/kg/min gtt Pathophysiology: direct arteriolar and venous dilator. The arteriolar dilation prevents the expected rise in vascular resistance when cardiac output falls as a result of venodilation Labetalol 2 mg/min gtt or 20-80 mg IV bolus q10min Combined alpha and beta blocker. Use with caution in patients with heart failure Nicardipine 2-10 mg/h IV CCB that provides gradual reduction in systemic pressure with little overshoot Enalapril 1.25-5mg q6h IV ACEI, can be used in patients with acute left ventricular failure Esmolol 200-500 mcg/kg per min for 4 minutes, then 50-300 mcg/kg/min IV Fast on-fast off, used with aortic dissection and in postoperative period Loop diuretics Almost always needed to overcome the tendency for renal sodium retention after MAP is lowered HTN Urgency o Nifedipine 10mg by mouth, repeat in 30 minutes if needed 19 Radiation-Induced Cardiac Injury Complication Constrictive Pericarditis Myocardial Fibrosis Valve Dysfunction Premature Coronary Artery Disease Diagnostic Testing CT scan Diastolic Damage, biopsy? TTE/TEE Coronary angiography or nuclear perfusion The relative risk of cardiovascular death is 3.1 at 10 years in patients with radiation therapy for Hodgkin’s disease, most due to premature coronary artery disease. Endocarditis Epidemiology Presentation Physical Exam Diagnosis Treatment Medical management Surgical management o Paravalvular extension 40% of native valve endocarditis Usually extends near the interventricular septum and AV node and therefore can cause conduction abnormalities o CHF (moderate or greater carries 56% mortality with medical therapy alone) o Severe valvular regurgitation with destruction o Life-threatening instability o Resistant bacterial infection or fungal infection o Vegetations larger than 1 cm o Recurrent distal embolization Mitral Valve Prolapse Epidemiology 2% of population Most common cause of mitral regurgitation Increased prevalence in marfan’s disease Presentation Palpitations or atypical chest pain/tightness/discomfort Symptoms of mitral regurgitation if severe Physical Exam Midsystolic click (sudden tensing of mitral subvalvular apparatus as the leaflets prolapse into the atria Valsalva and standing from squatting move the click closer to S1 20 Diagnosis TTE Treatment For palpitations – stop caffeine and other stimulant use Bicuspid Aortic Valve Epidemiology Presentation Physical Exam Diagnosis TTE Complications Sudden cardiac death Congestive Heart Failure Severe Aortic Stenosis Treatment Medical Management o Serial echocardiograms o Nifedipine – proven to delay need for valve replacement o ACEI – may be beneficial but unproven o Digoxin and diuretics for symptom relief o Beta-blockade is contraindicated in severe aortic regurgitation Surgical Management o Consider surgery in asymptomatic patients when LV end systolic diameter reaches 55 mm or EF < 60% Mechanical Valves May present with either: Thrombotic events o Similar to heart failure behind valve or valve regurgitation Embolic events o Similar to endocarditis Thrombotic events Prophylaxis warfarin dosing goal is based on risk factors o 2.5 to 3.5 for high risk Once thrombosis has occurred o Hemodynamically unstable Surgery Thrombolytic therapy o Hemodynamically stable Long-term medical management with appropriate anticoagulation 21 Warfarin Therapy Goal INR of 2 to 3 Complications o Anemia Check haptoglobin and lactate dehydrogenase as valves can shear RBCs Anemia in a patient who is therapeutic on warfarin usually signifies a gastrointestinal lesion Aortic Dissection Epidemiology 72% of older patients have history of hypertension Bicuspid aortic valve more common in younger patients In marfan’s patients, 50% have family history of dissection Clinical Presentation Classic presentation: chest pain radiating to back 6% are painless Diagnosis TEE CT with contrast MRI Classification Schemes Treatment Ascending: surgical Descending: medical Goals: Lower HR to under 60 Goal MAP of 60-75 BB are first line Esmolol: 200-500 mcg/kg/min x 4 min, then 50-300 mcg/kg/min Labetolol: 20-80 mg iv q10min. total 300 or 0.5-2.0mg/min IV gtt Then add on other agents Nitroprusside: start at 0.25-0.50 mcg/kg/min. Maximum dose is 8-10 mcg/kg/min but no more than 10 minutes at this dosage level. Watch for thiocyanate toxicity Nicardipine 2-10 and up to 15 mg/hour Congestive Heart Failure Treatment Medical o ACEI – proven survival benefit 22 o B-blocker Proven survival benefit for all classes of HF Do not initiate when patient is acutely decompensated or fluid overloaded because there is a transient decrease in cardiac output. Carvedilol vs. others o CCB – management of HTN or angina not adequately controlled on ACEI or BB EP o BiVenticular Pacing Indication: NYHA class III, LV enlargement, prolonged QRS complex, LVEF < 35% Surgical o Mitral Valve Repair Improves short and intermediate hemodynamic outcomes in patients with severe mitral regurgitation Not mortality benefit Prognosis EF of 20% carries a one year mortality of 20%? (or one year survival). Same as metastatic carcinoma 23 Bradyarrhythmias Results from either a 1. Failure to initiate an impulse or a 2. Failure to conduct an impulse And so the two most common causes of bradyarrhythmias are: 1. SA node dysfunction 2. AV conduction block SA Node The SA node is cluster of fusiform cells located in the sulcus terminalis on the epicardial surface of the heart at the right atrial-superior vena caval junction Is a relatively heterogeneous group of cells Typically contains fewer myofibrils, no intercalated disks, a poorly developed sarcoplasmic reticulum and no T-tubules Fed by SA nodal artery which arises from the right coronary in 55-60% of people and the left circumflex in 40-45% of people SA Node Dysfunction Broadly classified as extrinsic or intrinsic causes. In acute MI (typically inferior) the sinus abnormalities are usually transient. Causes of SA Node Dysfunction Intrinsic Extrinsic Sick Sinus Syndrome Carotid sinus hypersensitivity CAD Vasovagal stimulation Inflammatory Medications Pericarditis Beta-blockers Myocarditis CCB Rheumatic Antiarrhythmics Collagen vascular disease Adenosine Lyme disease Clonidine Senile Amyloidosis Lithium Congenital heart disease Cimetidine Radiation therapy Amitriptyline Post-surgical Phenothiazines Chest trauma Narcotics (methadone) Non-cardiac congenital diseases Pentamidine Hypothyroidism Sleep Apnea Hypoxia Endotracheal suctioning Hypothermia Increased ICP Clinical Features 1/3 to ½ will also develop a tachyarrhythmia 24 o tachycardia-bradycardia variant of SSS o Require anticoagulation Not associated with increased mortality except when it occurs with comorbidities Electrocardiography Usually defined as HR < 40 but depends on individual characteristics A sinus pause of greater than 3 seconds is indicative of sinus node dysfunction First degree block o Prolonged PR Second degree block o Type I Progressive prolongation of PR until pause o Type II No change in PR interval in beats before pause Third degree block o Complete disassociation Tachycardia-bradycardia syndrome o Brady alternating with tachy (most often atrial fibrillation) Chronotropic Incompetence o Inability of heart rate to increase in response to demand from exercise or stress Diagnostic Testing ECG Telemetry, holter, or event monitor Test for autonomic sensitivity Exercise testing (for ischemia or chronotropic incompetence) EP testing Treatment Exclude extrinsic causes No good chronic medical therapy available Pacemaker AV Conduction Disease Pathophysiology AV node is subendocardial Located in posterior-inferior right atrium Located at the apex of the triangle of Koch o Coronary sinus ostium posteriorly, septal tricuspid valve annulus anteriorly, and the tendon of Todaro superiorly Vascular supply o AV nodal artery o 1st septal perforator of the left descending coronary artery 25 Causes of Atrioventricular Block Autonomic Metabolic/Endocrine Infectious Congenital Inflammatory Infiltrative Neoplastic/Traumatic Degenerative CAD Drug Related Carotid sinus hypersensitivity Vasovagal Hyperkalemia Hypermagnesemia Hypothyroidism Adrenal insufficiency Endocarditis Lyme TB Chagas Syphilis Diptheria Toxoplasmosis Congenital Maternal SLE Others SLE RA MCTD Scleroderma Amyloidosis Sarcoidosis Hemochromatosis Lymphoma Mesothelioma Melanoma Radiation Catheter ablation Lev disease Lenegre disease Acute MI BB CCB Lithium Digitalis Adenosine Antiarrythmics AV conduction dysfunction in acute MI Transiently develops in 10-25% of patients Most commonly first or second degree block Inferior MI o Level of block is AV node o More stable narrow escape rhythms Anterior MI o Level of block is in distal AV nodal complex o Wide, complex, unstable escape rhythms o Worse prognosis, higher mortality Treatment o Inferior MI often produces transient AV conduction problems o Indications for pacing Persistent 2nd or 3rd degree block particularly if symptomatic Transient 2nd or 3rd degree block associated with BBB 26 First degree AV Block Second degree AV Block Mobitz type 1 (Wenckebach) o Progressive lengthening of PR interval until a QRS is dropped o Decremental conduction of electrical impulses in the AV node Mobitz type 2 o Typically occurs in distal or infra-His conduction system o Worse prognostically as may progress to higher grade Paroxysmal AV block o Series of nonconducted p waves o Indication for permanent pacemaker placement High-grade block o Intermediate between 2nd and 3rd degree block Treatment Exclude reversible causes Temporary and permanent pacemaker placement Tachyarrhythmias Atrial Premature Complexes (APCs) Clinic o Typically asymptomatic ECG o APCs reset the sinus node and there is a compensatory pause until the next sinus beat Treatment o Explanation and reassurance o Beta-blockers o Catheter ablation Inappropriate Sinus Tachycardia Etiology o Often postviral dysautonomia which may last 3-12 months and then resolve spontaneously Treatment o Hydration and salt-loading o Careful titration of beta-blockers Atrial Fibrillation Treatment o Acute Rate Control 27 28 Atrial Fibrillation Treatment Medical Therapy o Rate Control o Rhythm Control Antiarrhythmic drug therapy and attempts at restoring sinus rhythm should thus be reserved for patients who are symptomatic and who do not tolerate the rhythm well o Anticoagulation Surgical Therapy Hospitalization and anticoagulation are not indicated in a patient with a brief episode of atrial fibrillation, after spontaneous cardioversion. There is no indication for antiarrhythmic therapy in this clinical situation, but it may be considered if atrial fibrillation recurs with symptoms of dyspnea, fatigue, or intolerable palpitations. Atrial Flutter Diagnosis Saw-tooth waves most prominent in the inferior leads Treatment Radiofrequency catheter ablation is the therapy of choice for recurrent atrial flutter 90% success rate 29 Permanent Pacemakers and AICDs Pacemaker Threshold: An output from the pacemaker at which at which every impulse will stimulate the heart muscle at a time which the heart muscle would not be expected to be refractory. Pacemakers are set to 2-3 times the threshold Ex. Threshold value of 1.5 volts, then pacemaker output set to 3 to 4.5 volts Sensitivity: The voltage above which the pacemaker will consider a sensed electrical event as significant. Indications for permanent pacing: Class I evidence o 3rd degree AVB with either HR < 40 bpm Pauses >3 seconds Required drugs that may cause further bradycardia Post AVJ ablation Neuromuscular disease causing AVB o 2nd AVB with symptoms o Intermittent 3rd degree AVB with chronic bifascicular or trifascicular block o After AMI Transient infranodal advanced AVB with BBB Persistent and symptomatic 2nd or 3rd degree AVB o Symptomatic sinus bradycardia or chronotropic incompetence including if associated with necessary drug therapy exacerbating bradycardia o Pause dependent VT with or without prolonged QT o Syncope with carotid sinus massage induced pause >3 sec Class II evidence o Asymptomatic 3rd degree AVB with HR > 40 bpm o Asymptomatic type II 2nd degree AVB o Asymptomatic type I 2nd degree AVB if EPS documented block below or in His o Symptoms from first degree block o Marked first degree AVB >0.3 sec with impaired LV ad CHF o Syncope with chronic bifascicular or trifascicular block and no clear cause for syncope found o Chronic bifascicular or trifascicular block with HV >100 ms in asymptomatic patient o Chronic bi and trifascicular block with non-physiologic block below His found at EPS o After AMI Persistent 2nd and 3rd degree nodal AVB after MI o Minimally symptomatic but HR <30 bpm o High risk patients with congenital long QT o Prevention of symptomatic, drug refractory atrial fibrillation o Recurrent syncope with no clear cause but abnormal carotid sinus massage or with abnormal sinus or AV conduction incidentally detected on EP study o Neurocardiogenic syncope with significant bradycardia during tilt o Medically refractory HOCM Pacer Codes Chamber being paced A (atrial) Chamber being sensed A Mode of pacing I (inhibited) Rate Modulation 30 V (ventricular) D (dual) O (none) V D O T (triggered) D O Magnet application Turns off sensing and paces at set “magnet rate” ICD Indications Class I o Cardiac Arrest due to VF or VT without reversible cause o Spontaneous sustained VT o Syncope VF/VT at EPS when drug Rx is not tolerated, ineffective or not preferred o NSVT, low EF, prior MI, VT at EPS not suppressed with class I antiarrhymics (from MADIT study) Class II o Cardiac arrest presumed to be VF when EPS is contraindicated o Symptomatic VT in a patient awaiting heart transplant o Familial conditions with high risk of cardiac arrest like LQT or HOCM o NSVT, low EF, prior MI, VT at EPS o Recurrent syncope of unclear etiology with abnormal LV and VT at EPS Magnet Application A magnet placed over the OCD will temporarily or permanently turn the ICD off except for bradycardia pacing. Pregnancy Related Cardiology In young healthy women with cardiac chest pain consider spontaneous coronary artery dissection 2/2 hormonal and vascular changes Normal Dysfunction A basal systolic murmur is present in 80% of pregnant women owing to increased flow across the pulmonic and aortic valves. The resting heart rate increases by 20% to 30% during pregnancy as compared to before pregnancy An S3 gallop is common because of increased early diastolic ventricular filling. Contrast Nephropathy Prevention Acetylcysteine 1200 mg po q12h x 4 doses, please give at least 1 dose prior to catheterization and 2 doses post catheterization Treatment Stopping Medications Before Interventions PCI o ASA o Clopidogrel 31 o Abciximab o Eptifibatide o Heparin o Enoxaparin o Direct thrombin inhibitors CABG o ASA o Clopidogrel o Abciximab D/C and give 6-12 units of platelets o Eptifibatide D/C at least 4-6 hours prior o Heparin o Enoxaparin D/C 12-24 hours prior to CABG o Direct thrombin inhibitors Complications of Cardiac Catheterization Major o Death Approximately 0.1% High-risk groups NYHA class IV (10-fold increase in mortality) Left main coronary artery disease LVEF < 30% Valvular heart disease DM requiring insulin Cerebrovascular disease Pulmonary insufficiency Preexisting renal disease o MI o Stroke/TIA Especially high in those with AS who undergo retrograde catheterization of the aortic valve Local Vascular Complications o Hemostasis at the access site Devices used o Prior warfarin therapy Ideally INR < 1.5 but procedure is preformed with INRs of 2-3 o Hematoma formation Common, most resolve over days, intervention not usually required o Retroperitoneal extension o Pseudoaneurysm Pulsatile mass with a systolic bruit over catheter site Confirm by duplex US Most occur by day 3 o Arterial Thrombosis Lower extremity pain or paresthesia with reduced or absent distal pulses Urgent vascular surgery or thrombectomy may be required Atheroembolism 32 Secondary Prevention of CAD at Strong Weight control Exercise (30-60 minutes at least 3-4 days/week) Diet modification Alcohol reduction Medications o ASA daily o BB titrate for HR >50 or SBP >100 o Statin for LDL >100, cholesterol >160 o ACEI o Plavix Smoking cessation Blood Pressure Control: <140/90 or <130/85 in DM, HF, or RI Pulmonary Hypertension Classification Primary o Familial and idiopathic Secondary o Chronic venous thromboembolism o Scleroderma o HIV infection o Cirrhosis o Anorexigen use (phen-fen) Presentation DOE Palpitations Pre-syncope/syncope Physical Exam Prominent P2 because of higher pulmonary pressures Tricuspid regurgitation murmur JVP RV heave Ascites/edema Evaluation Pulse oximetry at rest and with exertion ECG CXR Spirometry Exercise Echo Management Referral to a specialist 33 Cardiology Trials RISC: ASA reduces risk of death and acute MI by 50% in patients with NSTEMI Cardiac Resynchronization–Heart Failure (CARE-HF) study has suggested improved survival with BiV pacers in select populations CURE trial (Clopidogrel in Unstable Angina to Prevent Recurrent Events): all TIMI risk score groups had a significant reduction in death, non-fatal MI, and stroke when given aspirin and plavix as opposed to aspirin and placebo ESSENCE trial (Efficacy and Safety of Subcutaneous Enoxaparin in Non-Q-Wave Coronary Events): Risk of death/MI post UA/NSTEMI was reduced in those treated with enoxaparin and aspirin as opposed to UFH and aspirin PROVE IT-TIMI 22 trial (Pravastatin or Atorvastatin Evaluation and Infection Therapy – Thrombolysis in Myocardial Infarction 22): intensive statin therapy (atorvastatin 80mg) decreased death or rehospitalization for recurrent ACS at 30 days as compared to pravastatin 40mg. CAST/SWORD: Trials showing that antiarrhythmics for non-lethal arrhythmias post MI may increase mortality ACS ECG Interpretation I High Lateral II Inferior/Posterior III Inferior/Posterior ECG Leads V1-V2 AVR AVL AVF Inferior/Posterior V1 Septal V2 Septal V3 Anterior Injury Related Artery LAD – septal V3-V4 Area of Damage Septum, HIS bundle, bundle branches Anterior wall LV V5-V6, I, aVL High Lateral Wall Circumflex II, III, aVF Inferior wall LV Posterior wall LV RV, inferior LV, posterior wall LV RCA – PDA Posterior wall LV Either CX or PDA V4R, (II,III, aVF) V1-V4(depression) LAD – diagonal RCA – Proximal V4 Anterior V5 Anterior V6 High Lateral Complications Infranodal block and BBBs LV dysfunction, CHF, BBBs, complete heart block, PVCs LV dysfunction, AV nodal block in some Hypotension, sensitive to nitrates and MSO4 Hypotension, supranodal and infranodal blocks, afib/flutter LV Dysfunction 34 Management of Hemodynamics in the CCU Variables Variable Cardiac Output Cardiac Index Stroke Volume Stroke Volume Index Systemic Vascular Resistance Pulmonary Vascular Resistance Left Cardiac Work Index Arterial Oxygen Content Mixed Venous Oxygen Content Arterio-venous Oxygen Difference Oxygen Consumption ABR CO CI SV SVI Normal Range 4-6 L/min 2.5-3.5 L/min/m2 60-70 mL/beat 41-51 mL/beat/m2 Derivation Meaning SVR PVR LCWI CaO2 CvO2 A-VO2D VO2 Cardiac Monitoring and Normal Values JVP/RA PA systolic PA mean PAWP/LA Cardiac Index SVR AVO2 difference (?) 0-8 cm 15-30 cm 9-16 cm 3-12 cm 2.6 – 4.2 (L/min/m2) 700-1600 2.9 – 5.3 mL/dL Calculations SVR = ((MAP – CVP)x79.9)/CO MAP = DBP + 1/3 (PP) AVO2 difference = (8.5 x 1.36 x Hgb x SaO2) – (1.36 x Hgb x Svo2) Laboratory Values Cardiac markers Non-MI causes of elevation of Troponin 35 1. 2. 3. 4. 5. 6. 7. 8. Defibrillator charge Renal Insufficiency LVH failure Tachy-arhythmias Myocarditis Pericarditis Pulmonary embolism Assay interference (heterophil antibodies, RF, excess fibrin) Pharmacology of Inotropes and Vasoactive Medications Catecholamines Derivatives of dopamine precursor Act on: Alpha receptors o Located in peripheral vessels o Cause vasoconstriction Beta receptors o Beta 1 Located on cardiac tissue Increased intracellular cAMP => increased intracellular calcium =>positive inotropic and chronotropic effects o Beta 2 Located in peripheral tissues and bronchial tree Increased intracellular cAMP => increased intracellular calcium =>relaxation of smooth muscle => vasodilation Dopaminergic receptors o Located primarily in splanchnic and renal circulation o Vasodilation Dopamine Low dose (1-3 micrograms/kg/min) o Dopaminergic receptor stimulation o Increases renal and splanchnic blood flow o Often used in cardiac failure in order to augment renal blood flow and facilitate diuresis with lasix 36 Intermediate dose (3-10 micrograms/kg/min) o Stimulates beta receptors by being a partial agonist itself and causing release of norepinephrine from cardiac nerve terminals o Commonly used in heart failure complicated by hypotension o Results in an increase in cardiac output and increases heart rate and myocardial oxygen demand which may worsen myocardial ischemia High dose (>10 micrograms/kg/min) o Alpha receptor stimulation o Causes systemic vasoconstriction o Supports blood pressure in shock states Administer via a central catheter as extravasation will lead to skin necrosis. If this occurs promptly inject phentalamine 10mg locally (alpha-adrenergic antagonist) Dobutamine Net effect o Increased myocardial contractility o Increased heart rate o Varying degree of peripheral vasodilation Use o To increase CO in patients with depressed left ventricular function and clinical heart failure and impaired cardiac output o Frequently combined with other agents Low dose dopamine to augment renal perfusion Nitroprusside for venodilation Dosing o Initial 2 micrograms/kg/min o Titrate to 10-15 micrograms/kg/min (target dose in CHF is 10) o Tolerance develops after several days of continued use Adverse Effects o Arrhythmia o Ischemia Norepinephrine Net effect o Increases cardiac contractility o Vasoconstriction Use o Profound hypotension and shock Dosing o 2-10 micrograms/min Adverse Effects o Arrhythmia Epinephrine Net effect o Increased cardiac contractility o Vasoconstriction Use o Cardiopulmonary arrest 37 o Shock o Cardiopulmonary bypass Dosing Adverse Effects o Arrhythmia o Tachycardia o Vasoconstriction o Cardiac Ischemia o Metabolic Acidosis that resolves with discontinuation Isoproteronol Phosphodiesterase Inhibitors Pathophysiology Inhibit break down of cAMP by membrane bound phosphodiesterase enzymes Milrinone Net effect o Increased CO via positive inotropy and vasodilation Use Dosing Adverse effects Vasodilators Nitroprusside Net effect in CHF o Fall in right atrial and pulmonary wedge pressure o Decrease in systemic vascular resistance Use Dosing o Start with lowest dose and titrate up Adverse effects o Cyanide toxicity in patients with underlying hepatic and/or renal disease who receive prolonged infusions Nitroglycerin Net effect o Venodilation Use o Ischemic heart disease o Acute pulmonary edema Dosing o Drip: 10 microgram/min o Paste o 0.4 mg SL Adverse effects o Headache 38 o Flushing o Hypotension (response quickly to d/c and fluids) Cardiac Medications Atropine Mechanism: Anticholinergic that increases firing of SA node and increases conduction through AV node Dosing Asystole, PEA: 1.0 mg IVP q3-5min to a total of 3.0 mg Bradycardia, symptomatic: 0.5-1.0 mg atropine q3-5min to total of 0.04mg/kg (approximately 3.0 mg in a 70kg patient) Third degree block: do not use Adverse Effects Notes: Heart transplants do not respond to atropine (lack parasympathetic innervation Nitroglycerin Mechanism: vasodilation Dosing Initial 5-15 mg/min Titrate as necessary by 5 mg/min q5min to relieve pain with a maximum of 200 mg/min Adverse Effects Headache: use Tylenol Nausea: Hypotension: volume expansion Tachycardia: volume expansion +/- alpha agonist Aspirin Mechanism: inhibits COX-1 platelet aggregation with 15 minutes Dosing: ASA 81-325mg qdaily Adverse Effects: Reversal: None Thienopyridines Mechanism Noncompetitive inhibition of ADP binding to type 2 purinergic receptor Inhibits activation of glycoprotein Iib/IIIA complex Ticlopidine Dosing: Requires 3-6 days of use for full effect Ticlopidine 250 mg po BID Adverse Effects 2.5% risk of neutropenia 39 1 in 1500 – 5000 develop TTP-HUS within first 12 weeks of therapy o Treatment is drug d/c and possible plasmaphoresis Clopidogrel Dosing Initial loading: Clopidogrel 300 mg Maintenance: Clopidrogrel 75 mg qdaily Adverse Effects 3-5% risk of major bleeding, esp in elderly Glycoprotein IIB/IIIA Receptor Inhibitors Mechanism: GPIIB/IIIA receptor binds fibrogen and is the mechanism for cross-linking platelets and therefore the antagonists inhibit platelet aggregation Classes Large-molecule agents (irreversible binders) o Abciximab (ReoPro) Small-molecule agents and non-peptides (reversible binders) o Eptifibatide (Integrilin) o Tirofiban (Aggrastat) Abciximab Used with ASA and heparin Dosing Adverse Effects o Bleeding from vascular access sites o Severe thrombocytopenia (< 50000) seen in 0.5-1.5% Monitoring o Check platelet counts within 4 hours of starting transfusion and again at end of transfusion Eptifibatide Tirofiban Unfractionated Heparin Mechanism: inhibits soluble clotting factors Dosing Adverse Effects Bleeding HIT o DX: 40 o TX: Low-Molecular-Weight Heparins Mechanism: increase factor Xa activity and decrease IIa activity compared to UFH Enoxaparin Dosing CrCl > 30 ml/min: 1 mg/kg SQ BID Adverse Effects Dalteparin Dosing Adverse Effects Direct Thrombin Inhibitors Mechanism: bind factor IIa, not dependent on ATIII Names Hirudin Lepirudin Argatroban Bivalirusin Adverse Events Increased risk of bleeding Statins Except for lipitor and crestor, statins should be taken at night. Intensive statin therapy should be used to ACS Ward Lessons Dr. Bis: Spironolactone is a bad diuretic and only acts as a diuretic at high doses. At low doses it is purely hormonal. Atenolol is renal excreted. Use metoprolol for Cr 1.5 and up Easiest way to create asystole is to give a patient with renal disease atenolol and diltiazem. In patients with heart failure consider whether or not to give them a regular or heart-healthy diet. In older patients who are not likely to change their diet after leaving the hospital it might be prudent to 41 give them a regular diet and adjust medications for it instead of having them discharged with a mismatched regimen. Beta-stimulant of choice is isoproterenol. Dobutamine is 2nd line. New cardiomyopathy just about always buys itself a cardiac cath to r/o reversible disease (such as left main disease). Heart failure patients – old, frail, unchangeable, may be better on a regular diet than a heart healthy diet Rewarming often overshoots the temp. So if they are febrile, it doesn’t mean they are infected unless there is also some other indication. Patient Checklist ACS Risk Stratification Medications o ASA o Beta blocker o Plavix o Statin o ACEI o Heparin Procedures o Fibrinolysis o Echo o Coronary angiography Heart Failure Underlying reason for CHF Reason for CHF exacerbation Timing of hospitalizations Home weight Medications o Beta-blocker o ACEI/ARB No benefit in using both If ACEI/ARB can not be tolerated (such as hyperkalemia) try a Hydralazine/Nitrate combination o Calcium-channel blocker If HTN not controlled by ACEI + beta-blocker o Spironolactone Reduces mortality in Class III-IV heart failure and EF < 35% o Digoxin Reduces symptoms and hospitalizations but not mortality 42 Physical Exam Right sided MI - hypotension, clear lung fields, and elevated jugular venous pressure Admission Notes STEMI NSTEMI back from cath CV: NSTEMI anterior ACS: BB, ASA Symptom management: morphine, nitro To cath: NPO, premeds (heparin gtt, infiximab, plavix) NSTEMI/UA Chest Pain ECHO/ETT in AM Admission Orders Cardiology ST-Elevation MI Admit to: CCU Diagnosis: STEMI Vital Signs: Unit routine, continuous telemetry Activity: Bedrest Nursing: O2 2L, increase as necessary to maintain oxygen saturation > 93% Guaic all stools FSBG ACHS Diet: NPO for prior to cardiac catheterization, then Heart Healthy Diet IV Fluids: NaHCO3 3 Amps in 1 Liter D5W – administer 250 ml/H x 1 hour, then 80 mL/h x 6 hours, then saline lock. HO: Call for SBP < 100 or >180 Call for HR < 50 or > 100 Medications: ASA 81 mg po qday Clopidogrel 75 mg po qday (for stents) Metoprolol 50 mg po q12h (begin in AM). Hold for SBP < 100, HR < 50 and call MD Eptibatide 2 microgram/kg/min for 18 hours post-stent placement Enalapril 2.5 mg po q12h – begin in AM. Hold for SBP < 100 Nitroglycerin 0.4 mg SL prn chest pain; may repeat in 5 minutes Morphine Sulfate 1-4 mg IV q5minutes prn chest pain, not to exceed 10 mg/h. Hold for sedation, RR < 10 breaths/min, or SBP < 90. 43 Labs ECG on admit and for recurrent chest pain Troponin I CBC now and qday (keep Hct > 30) Chem 7 now and qday Mg now and qday PT, INR, PTT Lipid panel UA Type and screen Discharge Planning: Meet with nutritionalist Smoking cessation Advice on activity and when it is safe to return to work Review of medications Discharge meds: BB, ASA, ACEI, Statin, Plavix UA/NSTEMI Admit to: CCU Diagnosis: UA and NSTEMI Vital Signs: Unit routine, continuous telemetry Activity: Bedrest Nursing: O2 2L, increase as necessary to maintain oxygen saturation > 93% Guaic all stools FSBG ACHS House Officer: Call for SBP < 100 or >180 Call for HR < 50 or > 100 Diet: NPO for prior to cardiac catheterization, then Heart Healthy Diet IV Fluids: Saline lock. Hydrate if going for cardiac catheterization with HCO3 3 amps in 1 L D5W and run at 3ml/kg in hour prior to catheterization and 1 mL/kg for 6 hours postcath. Medications: ASA 81 mg po qday Clopidogrel 300 mg po now and then 75 mg po qday Enoxaparin 1 mg/kg SQ q12h Metoprolol 50 mg po q12h – first dose now. Hold for SBP < 100, HR < 50 and call MD Nitroglycerin 0.4 mg SL prn chest pain; may repeat in 5 minutes Morphine Sulfate 1-4 mg IV q5minutes prn chest pain, not to exceed 10 mg/h. Hold for sedation, RR < 10 breaths/min, or SBP < 90. Labs ECG on admit and for recurrent chest pain Troponin I CBC now and qday (keep Hct > 30) Chem 7 now and qday Mg now and qday PT, INR, PTT Lipid panel UA 44 Discharge Planning: Meet with nutritionalist Smoking cessation Advice on activity and when it is safe to return to work Review of medications Discharge meds: BB, ASA, ACEI, Statin, Plavix 45 Atrial Fibrillation Admit to: Telemetry Diagnosis: Atrial fibrillation Vital Signs: Vitals q2h x 4, then decrease to q4h, continuous telemetry Activity: As tolerated, teach patient to sit at side of bed for several minutes before standing Nursing: O2 2L per NC if oxygen saturation < 93% House Officer: Call for SBP < 100 or >180 Call for HR < 60 or > 140 Diet: If cardioversion is planned NPO 8 hours prior, else Heart Healthy Diet IV Fluids: Saline lock. Medications: ASA 81 mg po qday (if warfarin is not going to be prescribed) Rate control medications (see table) Warfarin (for CHAD2 score > 2) 5 mg po tonight, dose of warfarin to be adjusted daily based on PT/INR Medication Dosing Metoprolol/atenolol Diltiazem Digoxin CHADS2 CHF HTN Age >= 75 Diabetes H/O stroke or TIA 1 1 1 1 2 Labs ECG on admit and for chest pain TSH, T4 Troponin I Iron panel CBC TTE/TEE Chem 7 PT, INR, PTT CXR Lipid panel Mg Discharge Planning: Cardioversion or rate control at 60-80 at rest and up to 115 with exercise Smoking cessation Advice on activity and when it is safe to return to work Review of medications Assessment for OSA 46 FU with cardiology Discharge meds: Warfarin or ASA 47 Congestive Heart Failure Admit to: Telemetry Diagnosis: Congestive Heart Failure Vital Signs: Vitals on admit and q4h, then decrease to q4h, weight upon admission, orthostatic BP each morning (to assess diuresis), continuous telemetry Activity: Bedrest with bathroom privileges, up only with assistance. Fall precautions. Nursing: O2 per NC to maintain oxygen saturation > 92% Daily weights Strict I/Os House Officer: Call for SBP < 100 or >180 Call for HR < 60 or > 140 Diet: 2 g sodium restriction, heart healthy diet, nutrition consult for teaching on lowsodium diet IV Fluids: heparin lock. Medications: ASA 81 mg po qday (if warfarin is not going to be prescribed) Lasix 80 mg IV now, then 60 mg IV BID (depends on home dose, may try bumetanide or torsemide if lasix restistant) Chlorothiazide if not reaching goal diuresis (monitor potassium) Spironolactone for patients with NYHA class IV HF or renal insufficiency ACEI or ARB for HF with reduced LVEF Digoxin 0.125 mg po qday (consider if already on BB, ACEI, diuretic and symptomatic) Hold BB until after resolution of volume overload Morphine may improve vascular resistance and symptoms in patients with significant pulmonary edema, increased anxiety and work of breathing ABX if pneumonia is suspected Labs NYHA CLASSIFICATION OF HEART FAILURE Class I: patients with no limitation of activities; they suffer no symptoms from ordinary activities. Class II: patients with slight, mild limitation of activity; they are comfortable with rest or with mild exertion. Class III: patients with marked limitation of activity; they are comfortable only at rest. Class IV: patients who should be at complete rest, confined to bed or chair; any physical activity brings on discomfort and symptoms occur at rest. ECG on admit and for chest pain Troponin I 48 CBC Chem 7 CXR Mg TSH, T4 Iron panel TTE/TEE UA Lipid panel BNP Discharge Planning: Obtain copy of prior echo Cardiology consult – repeat echo if significant decline or echo was remote How many exacerbation in past year? Counciling of monitoring daily weights Nutrition consult Smoking cessation Advice on activity Review of medications Assessment for OSA FU with cardiology Discharge meds: 49 Syncope Admit to: Telemetry Diagnosis: Syncope Vital Signs: Vitals on admit and q4h, if severe volume depletion is suspected consider vitals q2-4 hours over first 12 to 24 hours to monitor volume repletion. continuous telemetry Activity: fall risk, up with assistance only Nursing: O2 per NC to maintain oxygen saturation > 92% Daily weights House Officer: Call for SBP < 100 or >180 Call for HR < 60 or > 140 Diet: Regular IV Fluids: heparin lock. Medications: Heparin 5000 U SQ TID Docusate 250 mg po bid prn (hold for loose stools) Labs ECG on admit Troponin I CBC Chem 7 CXR Mg TSH, T4 UA Tox screen bHCG Other possible o EEG o BNP o Stress test o Holter monitoring o EP studies o Tilt-table test Discharge Planning: Advance activity after first 24 hours Cardiology consult if warranted Neurology consult if warranted Pysch consult if warranted If orthostatic: education about sitting at side of bed, script for compression hose Discharge meds: 50 Hypertensive Emergency Admit to: ICU Diagnosis: HTN Emergency Vital Signs: Vitals on admit and q1h, BP q30 minutes (call HO with result) possible continuous BP monitoring with an arterial line if refractory to initial management or nitroprusside to be used. Activity: bedrest Nursing: O2 per NC to maintain oxygen saturation > 92% I/Os Neuro checks q2h House Officer: Call for SBP >190 or DBP > 110 Call for HR < 60 or > 140 Call HO for nausea, vomiting headache, tinnitus, seizure, muscle spasm, delirium while nitroprusside infusion is running Diet: Low-sodium diet IV Fluids: ½ NS TKO. Medications: Sodium nitroprusside IV infusion. Begin at 0.1 microgram/kg/min and titrate q15m to achieve 25% reduction in MAP within first 3-4 hours Docusate 250 mg po bid prn (hold for loose stools) Alternatives to Nitroprusside Labetalol 20 (40,60) mg IV bolus q 10-15 minutes or as continuous infusion Fenoldapam IV infusion Nicardipine IV infusion Hydralazine IV Contraindicated in CHF, bradycardia, heart block, RAD Dopamine antagonist, can be used in RI but can raise intraocular pressure (CI in glaucoma) Vasodilator Reflex tachycardia (CI in MI, increased ICP and aortic dissection) Nitroglycerin IV infusion Labs ECG on admit Troponin I CBC with smear Chem 7 CXR Mg TSH, T4 UA Tox screen BHCG CT of head Discharge Planning: 51 Graph planned BP goals for first day Assess each organ system for damage and recovery over time Consider assessment for secondary causes of HTN Neuro consult for stroke or intracranial hemorrhage Discharge meds: Aortic Dissection Admit to: ICU Diagnosis: Aortic Dissection Vital Signs: Vitals on admit and q1h, Continuous BP monitoring via arterial line Activity: absolute bedrest Nursing: O2 per NC to maintain oxygen saturation > 92% I/Os Neuro checks q1h Check pulse in LE q1h and call if change House Officer: Call for SBP >120 or DBP > 80 Call for HR < 50 or > 80 Call for UO < 30 ml/h Diet: NPO IV Fluids: ½ NS TKO. Medications: Labetalol 5-10 mg IV now, then 1 mg/min continuous infusion. Titrate up to achieve SBP 95-110 mmHg over first hour. Call HO if SBP goal can not be reach (may add nitroprusside at 0.3 microgram/kg/min and titrate q15min until goal achieved) Esmolol is an alternative to labetalol Morphine sulfate 1-4 mg IV q1h prn pain (hold for sedation or RR < 11) Docusate 250 mg po bid prn (hold for loose stools) Labs ECG on admit Troponin I CBC now and qday Coag panel now and qday Chem 7 now and qday CXR LFTs Mg TSH, T4 UA Tox screen BHCG CT of chest & abd with contrast TEE 52 Discharge Planning: Possible surgery Assess each organ system for damage and recovery over time Assessment for causes of dissection FU with cardiology Discharge meds: ACS algorithm Is this cardiac? Proper meds History Risk stratification with TIMI score Review ECG Where part of the heart is this occurring in? What is the suspect vessel? What are the complications? Review trops and cardiac markers Orders Set Examples Patient with chest pain from afib, no ECG changes, no positive trops Went to cath for unstable angina 4 days later DIAGNOSIS 1. CHEST PAIN DVT PROPHYLAXIS NOT INDICATED NRT NOT INDICATED PATIENT CONDITION SATISFACTORY VITAL SIGNS Q4HRS DAILY UNTIL D/C OXYGEN: NASAL CANNULA HEART HEALTHY-4GM NA, MOD FAT FOR CHEST PAIN : FOR CHEST PAIN CALL HO/MLP : TEMPERATURE > 38.5 C CALL HO/MLP : RESPIRATIONS < 10 > 30 CALL HO/MLP : PULSE < 50 > 110 CALL HO/MLP : SBP < 100 > 180 CALL HO/MLP : OXIMETRY < 92.0 TELEMETRY ACETAMINOPHEN 650. MG PO Q4H PRN DOCUSATE SODIUM 100. MG PO BID PRN NITROGLYCERIN 0.4 MG SL Q5M PRN ELECTROCARDIOGRAM Q8HRS DAILY X 24 HOURS TROPONIN I, ULTRASENSITIVE STAT FUROSEMIDE 20. MG PO ONCE EACH DAY DIGOXIN 125. MCG PO ONCE EACH DAY 53 WARFARIN SODIUM 2.5 MG PO ONCE EACH DAY CALCIUM CARBONATE/VITAMIN D 1. TAB PO BID MAALOX 30. ML PO Q6H PRN DIGOXIN 125. MCG PO ONCE EACH DAY FUROSEMIDE 20. MG PO ONCE EACH DAY NITROGLYCERIN 0.4 MG SL Q5M PRN MAY REPEAT X3 DOSES DOCUSATE SODIUM 100. MG PO BID PRN ACETAMINOPHEN 650. MG PO Q4H PRN CALL HO/MLP : OXIMETRY < 92.0 COMPLETE BLOOD COUNT W/ PLTCNT ONCE DAILY X 3 DAYS TROPONIN I, ULTRASENSITIVE CK, SERUM PROTIME, BLOOD LIVER PROFILE, SERUM LIPID PROFILE ASPIRIN, ENTERIC COATED 325. MG PO ONCE EACH DAY ACTIVITY AS TOLERATED ELECTROCARDIOGRAM ONCE DAILY X 3 DAYS METOPROLOL TARTRATE 12.5 MG PO BID Pre-Cath Orders NPO AFTER MIDNIGHT COags Post-Cath CALL CARDIAC CATH FELLOW FOR: Y CONT DAILY UNTIL D/C N/V, CHEST PAIN/ANGINA, RESPIRATION RATE < 12, UNCONTROLLED BLEEDING AT SITE, HEMATOMA FORMATION, MENTAL STATUS CHANGES, SEVERE BACK PAIN IF PULSE DROPS 10 BEATS/MIN FROM BASELINE OR < 50 BEATS/MIN: 54 Y FROM BASELINE OR < 50 BEATS/MIN: AND BP DROPS 20MM FROM BASELINE, GIVE 0.5MG ATROPINE AND NOTIFY CARDIAC CATHETERIZATION FELLOW IF BP DROPS 20MM FROM BASELINE OR SBP < 100 Y BASELINE OR SBP < 100 GIVE 250CC NS BOLUS, PUT PATIENT IN TRENDELENBURG POSITION AND NOTIFY CARDIAC CATHETERIZATION FELLOW CHECK CATH INSERTION SITE CHECK WITH EACH VS FOR BLEEDING, HEMATOMA OR PULSE LOSS VITAL SIGNS DAILY Q15MIN FOR 1H Q30MIN FOR 1H Q1HR FOR 1H Q4HRS UNTIL D/C HOB NO MORE THAN 30 DEGREES BEDREST - STRICT RESUME DIET AND MEDICATIONS ENCOURAGE PO INTAKE MORPHINE SULFATE 2. MG IV X 1 NSTEMI went to cath PANTOPRAZOLE 40. MG PO ONCE EACH DAY NITROGLYCERIN 2% OINT. 1. IN. TRANSDERM. ONCE EACH DAY 55 NITROGLYCERIN 0.3 MG SUBLINGUAL Q5M PRN DIPHENHYDRAMINE HCL 25. MG PO QHS PRN ACETAMINOPHEN 650. MG PO Q4H PRN ALPRAZOLAM 0.25 MG PO Q8H PRN X 7 DAYS CLOPIDOGREL BISULFATE 600. MG PO X 1 STAT CLOPIDOGREL BISULFATE 75. MG PO ONCE EACH DAY ATORVASTATIN 40. MG PO ONCE EACH DAY LISINOPRIL 10. MG PO ONCE EACH DAY ASPIRIN, ENTERIC COATED 325. MG PO ONCE EACH DAY METOPROLOL TARTRATE 25. MG PO Q12HRS DOCUSATE SODIUM 100. MG PO BID SENNA 1. TAB PO BID Admission STEMI A/P 81 yo F with no significant PMH developed CP while walking 1. CVS – STEMI a. Will place on metoprolol 6.25 BID, asa 325 QDAY, Plavix 75 QDAY, zocor 80 QDay b. Telemetry c. CXR d. Trend cardiac enzymes e. NTG prn CP f. Check fasting lipid profile and LFTs g. Avoid ACEI until renal function known h. Other recs (integrillin and acetylcysteine) per cath protocol from cath fellow 2. Renal – FU creatinine 3. PPX – heparin SQ when? 4. PMH/Home meds 5. Dispo RAD CHEST SINGLE VIEW NS IV CONT ACETYLCYSTEINE 1200. MG PO BID X 48 HOURS EPTIFIBATIDE DRIP 750. MCG/ML IV CONT I&O FOR CHEST PAIN : FOR CHEST PAIN CALL HO/MLP : SBP < 100 CALL HO/MLP : PULSE > 110 CALL HO/MLP : TEMPERATURE > 38.0 C CHECK CATH INSERTION SITE VITAL SIGNS Q15MIN FOR 1 H , Q30MIN FOR 1H , Q4HRS DAILY UNT TELEMETRY 56 HOB NO MORE THAN 30 DEGREES BEDREST - STRICT ELECTROCARDIOGRAM ONCE DAILY X 3 DAYS PROFILE 8 (BASIC METABOLIC) ONCE DAILY X 3 DAYS CBC, PLT AND DIFF ONCE DAILY X 3 DAYS LIVER PROFILE, SERUM SIMVASTATIN 80. MG PO ONCE EACH DAY CLOPIDOGREL BISULFATE 75. MG PO ONCE EACH DAY NITROGLYCERIN 0.3 MG SUBLINGUAL Q5M PRN METOPROLOL TARTRATE 6.25 MG PO BID ACETAMINOPHEN 650. MG PO Q4H PRN ASPIRIN, ENTERIC COATED 325. MG PO ONCE EACH DAY PROTIME, BLOOD APTT, BLOOD LIPID PROFILE NEXT AM COMPLETE BLOOD COUNT W/ PLTCNT PROFILE 8 (BASIC METABOLIC) TROPONIN I, ULTRASENSITIVE Q8HRS DAILY X 24 HOURS *CK ISOENZYME, SERUM Q8HRS DAILY X 24 HOURS OXYGEN: NASAL CANNULA WEIGHT MAY BE OFF TELEMETRY FOR TESTS TELEMETRY I&O HEART HEALTHY-4GM NA, MOD FAT CALL HO/MLP : FOR CHEST PAIN CALL HO/MLP : OXIMETRY < 91 CALL HO/MLP : SBP < 100 > 160 ; DBP > 100 CALL HO/MLP : RESPIRATIONS < 8 > 22 CALL HO/MLP : PULSE < 55 > 95 CALL HO/MLP : TEMPERATURE < 35 C > 38 C VITAL SIGNS Q4HRS DAILY UNTIL D/C PATIENT CONDITION SATISFACTORY ADMIT PATIENT TO 736 ; DELEHANTY, JOSEPH M FULL CODE DIAGNOSIS 1. STEMI ORDERS BB are first line Esmolol: 200-500 mcg/kg/min x 4 min, then 50-300 mcg/kg/min Labetolol: 20-80 mg iv q10min. total 300 or 0.5-2.0mg/min IV gtt Then add on other agents 57 Nitroprusside: start at 0.25-0.50 mcg/kg/min. Maximum dose is 8-10 mcg/kg/min but no more than 10 minutes at this dosage level. Watch for thiocyanate toxicity Nicardipine 2-10 and up to 15 mg/hour 58