ชื่อเรื่องภาษาไทย (Angsana New 16 pt, bold)
advertisement

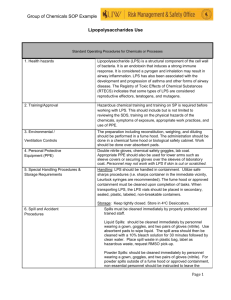
EFFECTS OF LIPOPOLYSACCHARIDE TIME EXPOSURE ON CELL VIABILITY AND PRO-INFLAMMATORY CYTOKINE EXPRESSIONS OF PALMITIC ACID TREATED THP-1 Annette d’Arqom1a,*,2, Voravich Luangwedchakarn1,#, Pinklow Umrod1 1 Department of Immunology, Faculty of Medicine Siriraj Hospital, Mahidol University, Thailand a Graduate programe in Immunology 2 Department of Pharmacology, Faculty of Medicine, Airlangga University, Indonesia *e-mail: annette.dar@student.mahidol.ac.th #e-mail: voravich.lua@mahidol.ac.th Abstract Metabolic endotoxemia is an emerging hypothesis in immunology, refers to increasing of endotoxin plasma in the level that cannot induce sepsis. It has been connected to pathogenesis of chronic inflammation condition in obesity, insulin resistance, and malignancies. In obesity, high level of saturated fatty acids (SFAs), such as palmitic acid (PA) was observed. Moreover, PA can activates pathogen recognition patterns (PRRs) and leads to pro-inflammatory cytokines production. This is also a result from cross-talk of macrophages and adipocytes in adipose tissue. Increasing lipopolysaccharide (LPS) level in the blood also monitored after high fat diet and correlated with low grade chronic inflammation. Aim of this study is to observed effect of LPS time incubation on cells viability and pro-inflammatory cytokine mRNA expression of palmitic acid treated THP-1 cells. Combination of PA and low dose LPS reduce cell viability after 8 hours incubation with LPS 1 ng/ml (82.5 + 2.5%, p < 0.0001). This combination also increases cytokine mRNA expressions with different dynamic for each cytokine. TNF-α (44.045 + 12.851), IL-6 (45.413 + 11.759), and IL-8 (146.836 + 23.385) reach the highest expression at 4 hours (p > 0.05, p < 0.05, p < 0.0001, respectively). While IL-1β mRNA expression increase maximally after 2 hours exposure time of LPS (285.841 + 44.815, p > 0.05). This finding shows exposure to LPS low dose can enhance inflammatory response to PA. Longer exposure time might bring detrimental effect to the cells. Keywords: palmitic acid, lipopolysaccharide, metabolic endotoxemia Introduction Metabolic endotoxemia is a new hypothesis in immunology. It refers to increasing of blood endotoxin (lipopolysaccharide) in subclinical level which lowers than sepsis (2). It has been linked to low chronic inflammatory condition that usually occurs in obesity, insulin resistance, malignancies, etc. Mechanisms on how LPS activate immune system in sepsis or cytokine storms are clearly established. In the other hand, how low dose of LPS induced secretion of cytokines, adipokines, and other mediators is unclear. Furthermore, the causes, effects, and molecular mechanisms still need further investigation. Many studies try to reveal the causes of metabolic endotoxemia, such as smoking, alcohol intake, and high fat diet (3-5). Increasing saturated fatty acids (SFAs), such as palmitic acid (PA) is correlated with obesity marker (6). Several studies discover that SFAs can activate TLRs and further activate NF-κB pathway (7-10). Increasing on pro-inflammatory cytokines, both in mRNA and protein level, are results of this process (9, 11-13). Murine study by Cani, et al shows correlation between fat intake and increase of endotoxin level in the blood and further induces insulin resistance (14). Changes in gut bacteria probably an answer why the LPS can escape to the blood circulation (15). How long this LPS has an effect on the body after fat diet is also still unclear. Thus, this study try to reveal the effect of low dose LPS time exposure on PA treated human monocytic cell line in term of cell viability and pro-inflammatory cytokine mRNA expressions. Methodology Cell culture THP-1 cells (American Type Culture Collection, Virginia, USA) were cultured in ATCC modified RPMI-1640 that contained 4.5 g/L of D-Glucose, 2.383 g/L of HEPES buffer, L-Glutamine, 1.5 g/L of Sodium Bicarbonate, 110 mg/L of Sodium Pyruvate, 0.05 mM of 2-mercaptoethanol (2-ME), 10% heat inactivated Fetal Bovine Serum, with 100 U/ml of Penicillin and 100 µg/ml of Streptomycin (pH 7.2-7.4) and incubated at 5% CO2, 37°C. Cells were maintained at a density not more than 1x106 cells/ml. Trypan blue staining was used to determine cell viability. Palmitic acid preparation NaOH 1 N was diluted to final concentration 0.3 N with endotoxin free water and mixed with absolute ethanol (3:7). This solution was used to dissolve 0.01 gram of palmitic acid (Sigma-Aldrich, Saint Louis, USA) until final concentration 0.039 M and heated to 70ºC. Furthermore, 0.039 M palmitic acid were diluted to 50 – 200 µM using complete RPMI containing 10% FBS, and incubated in 37°C for 30 minutes to let palmitic acid bound to albumin in FBS. This solution was prepared freshly prior to experiment. Palmitic acid solution was added to cell suspension at 1:1 ratio. Lipopolysaccharide preparation One mg/ml stock of lipopolysaccharide (LPS) was made by dissolving 1 mg LPS in 1 ml endotoxin free water and stored in -20ºC until used. Further dilutions were performed to reach final concentration 1 µg/ml. For cell stimulation, LPS were added to complete RPMI with 10% FBS to final concentration of 2 ng/ml, and added to cell suspension at 1:1 ratio. PA and LPS stimulation Methods from Schwartz, et al. were adapted . Briefly, cells (5x105 cells/ml) were resuspended in complete media with palmitic acid 100 µM and seeded in 6-well plates (2 ml). After incubated for 4 hours, they were washed with DPBS before LPS stimulation (1 ng/ml) or adding media for 4 hours (13). Furthermore, cells were collected and resuspended with 50 µl DPBS and 350 µl RNAlater™ to preserved RNA. RNA extraction, cDNA synthesize, and qRT-PCR Total RNA of stimulated cells was extracted using Invitrap® Spin Universal RNA Mini Kit (Invitek GmbH, Berlin, Germany) following the manufactured instruction. Briefly, cells were lysed and homogenized before applied in the column. After washing, total RNA was eluted and continuously converted to cDNA by M-MLV reverse transcriptase using the Superscript™ III First-Strand Synthesis System (Invitrogen, Carlsbad, CA, USA). Up to 5 μg of total RNA were converted to cDNA following the manufactured instruction. Reverse transcription reaction was performed in an PCR machine GeneAmp® PCR System 9700. The cDNA were directly used either for conventional and real time PCR or stored in -20ºC. The expressions of gene of interest were determined by semi-quantitative real-time PCR on the CFX96™ Real-Time PCR Detection System. The reactions were performed using 1X Brilliant III Ultra-Fast SYBR® Green QPCR Master Mix containing 2.5 mM MgCl2 and 0.4 μM of each forward and reverse primer, under the following condition: heat-denaturation at 95°C for 3 minutes followed by cycled amplification at 95°C for 5 seconds, 59°C for 10 seconds and 72° for 5 seconds for 40 cycles. Changes on gene expression were measured with ddCt calculation. The individual primer pairs and the expected PCR products were shown below. Table 1. Primer sequences Gene Accession no. GAPDH NM_002046.4 TNF-α NM_00059.2 IL-1β NM_000576.2 IL-6* NM_000600.3 IL-8 NM_000584 Primer (5'-->3') F ACAGCCTCAAGATCATCAGCA R GATGGCATGGACTGTGGTCA F CAGGCAGTCAGATCATCTTC R CTGGTTATCTCTCAGCTCCA F TGGAGCAACAAGTGGTGT R TTGGGATCTACACTCTCCAGC F CGGGAACGAAAGAGAAGCTCTA R GGCGCTTGTGGAGAAGGAG F GCCAACACAGAAATTATTGTAAAGCTT R AATTCTCAGCCCTCTTCAAAAACTT Size (bp) 119 147 157 68 112 * Primers of IL-6 were quoted from previous study (1) Statistical analysis One way ANOVA was used to analyze whether there is a different between each condition and post hoc test (Tukey) was performed. All data were analyzed by GraphPad Prism 3.00. Results Cell viability under PA and LPS low dose influence The results showed cell viability after treated with PA alone in all incubation time were more than 90%. But in the cell that treated with low dose LPS for 8 hour, cell viability (82.5 + 2.5%) was reduced compared to media (p < 0.0001) (Figure 1). Figure 1. Effect of LPS time exposure on PA treated THP-1 cell viability. Cells were treated with PA 100 µM for 4 hours, followed with (white bar) or without (gray bar) LPS 1 ng/ml for several incubation time (0, 2, 4, 8 hours). Cells viability was measured by trypan blue exclusion. Results are presented as mean ± SEM of three independent experiments. * compared to untreated, # compared to before LPS stimulation. *,# P < 0.05, **,## P < 0.01, ***,### P < 0.001. Pro-inflammatory cytokine mRNA expressions qRT-PCR results show PA or LPS low dose itself can induce all pro-inflammatory cytokine mRNA expressions. Moreover, combination of PA and LPS exaggerate their expressions in all incubation time. Each cytokine expressions has different dynamic, but in average, LPS low dose exposure for 4 and 8 hours give the highest different between LPS and PA + LPS (Figure 2). Figure 2. Effect of LPS on PA treated THP-1 cells on pro-inflammatory cytokine expressions. Real-time PCR analyses of pro-inflammatory cytokine expressions: TNF-α, IL-1β, IL-6, and IL-8, after treated with 100 µM of PA for 4 hours, followed with or without LPS 1 ng/ml. Results are presented as mean ± SEM of three independent experiments. * compared to LPS. * P < 0.05, ** P < 0.01, *** P < 0.001. For TNF-α, LPS low dose alone induce cytokine mRNA expression with the peak at 2 hours, reduce at 4 hours, and diminish at 8 hours. Combination of PA and low dose LPS give a different pattern but not significantly different. Its expression starts to increase since the beginning and reach the peak at 4 hours and decline at 8 hours. For IL-1β, both LPS and PA + LPS reach the peak at 2 hours and decrease at 4 and 8 hours, but not significantly different. Interestingly, combination of PA and LPS induce higher mRNA expression than LPS alone. Interleukin 6 and IL-8 have similar pattern in their cytokine gene expressions. LPS low dose alone induce cytokine mRNA expression with the peak at 2 hours and start to reduce. Moreover, LPS stimulation on PA treated THP-1 cells increase the expression on 2 hours, reach peak at 4 hours, and decline at 8 hours (IL-6 p < 0.05, IL-8 p < 0.001). Therefore, the longest LPS exposure time for TNF-α, IL-6, and IL-8 gene expression is 4 hours. This exposure time changes the mRNA expressions (fold change) of TNF-α (44.045 + 12.851), IL-6 (45.431 + 11.759), and IL-8 (146.836 + 23.385). While IL-1β reach the highest expression at 2 hours (285.841 + 44.815) Discussion and Conclusion The source and the cause of metabolic endotoxemia or metaflammation is complex and poorly understood (16). High level of free fatty acid that found in obesity, can promotes cross-talk between macrophages and adipocytes, leads to low grade inflammation. Furthermore, increasing of LPS level post-free fatty acid consumption induces more inflammation (14). In this present study, combination of PA and low dose LPS exaggerate inflammation of THP-1 cells. Longer time exposure of low dose LPS on PA treated THP-1 cells can reduce cell viability, and enhance cytokine mRNA expression. These effects vary between each cytokines, but in a same trend. Two until 4 hours LPS treatment after PA stimulation induce the highest cytokines expression. In line with reduction of cell viability, cytokine mRNA expressions diminish after 8 hours. The mechanisms of how this phenomenon occurs are still under investigation. Enhancement in inflammation induces by PA with LPS, probably caused by TLR-2 and TLR4 activation at lipid raft (7-10, 17-19). This process activate MyD88 dependent and independent pathway, further activate NFB translocation (7). Moreover, PA also induces phosphorylation of kinase family such as MAPK, JNK, ERK1/2, and p38. Their phosphorylations activate inflammation-related transcription factors, such as NF-B, C/EBP, and AP-1 (13, 20). Interestingly, inflammasome might have contribution in inflammation caused by PA, as PA can acts as the second signal for inflammasome activation (21). This activation not only lead to IL-1β and IL-18 processing, but promote activation of NF-B and AP-1, resulted in enhancing transcription of others pro-inflammatory cytokines (22). References 1. Tchernof A, Després J-P. Pathophysiology of Human Visceral Obesity: An Update. Physiol Rev. 2013 January 1, 2013;93(1):359-404. 2. Chang S, Li L. Metabolic Endotoxemia: A Novel Concept in Chronic Disease Pathology. J Med Sci. 2011;31(5):191-209. 3. Hasday JD, Bascom R, Costa JJ, Fitzgerald T, Dubin W. BActerial endotoxin is an active component of cigarette smoke*. CHEST Journal. 1999;115(3):829-35. 4. Parlesak A, Schäfer C, Schütz T, Bode JC, Bode C. Increased intestinal permeability to macromolecules and endotoxemia in patients with chronic alcohol abuse in different stages of alcohol-induced liver disease. J Hepatol. 2000 5//;32(5):742-7. 5. Laugerette F, Vors C, Peretti N, Michalski M-C. Complex links between dietary lipids, endogenous endotoxins and metabolic inflammation. Biochimie. 2011 1//;93(1):39-45. 6. Warensjo E, Margareta O, Bengt V. Fatty acid composition and estimated desaturase activities are associated with obesity and lifestyle variables in men and women. Nutrition, Metabolism & Cardiovascular Diseases. 2006;16:128-36. 7. Huang S, M. RJ, G. SR, Ono-Moore K, Schneider DA, Newman JW, et al. Saturated fatty acids activate TLR-mediated pro-inflammatory signalling pathways. J Lipid Res. 2012;53:2002-13. 8. Lee JY, Plakidas A, Lee WH, Heikkinen A, Chanmugam P, Bray G, et al. Differential modulation of Toll-like receptors by fatty acids: preferential inhibition by n-3 polyunsaturated fatty acids. J Lipid Res. 2003;44:479-86. 9. Weatherill AR, Lee JY, Zhao L, Lemay DG, Youn HS, Hwang D. Saturated and Polyunsaturated Fatty Acids Reciprocally Modulate Dendritic Cell Functions Mediated through TLR4. J Immunol. 2005;174:5390-7. 10. Shi H, Kokoeva MV, Inouye K, Tazameli I, Yin H, Flier JS. TLR 4 links innate immunity and fatty acid-induced insulin resistance. J Clin Invest. 2006;116(11):3015-25. 11. Erridge C, Samani NJ. Saturated Fatty Acids Do Not Directly StimulateToll-Like Receptor Signaling. Arterioscler Thromb Vasc Biol. 2009;29:1944-9. 12. Laine PS, Schwartz EA, Wang Y, Zhang W-Y, Karnik SK, Musi N, et al. Palmitic acid induces IP-10 expression in human macrophages via NF-kB activation. Biochem Biophys Res Commun. 2007;358(1):150-5. 13. Schwartz EA, Zhang W-Y, Karnik SK, Borwege S, Anand VR, Laine PS, et al. Nutrient Modification of the Innate Immune Response: A Novel Mechanism by Which Saturated Fatty Acids Greatly Amplify Monocyte Inflammation. Arterioscler Thromb Vasc Biol. 2010 April 1, 2010;30(4):802-8. 14. Cani PD, Amar J, Iglesias MA, Poggi M, Knauf C, Bestelica D, et al. Metabolic Endotoxemia Initiates Obesity and Insulin Resistance. Diabetes. 2007;56:1761-72. 15. Manco M, Putignani L, Bottazzo GF. Gut Microbiota, Lipopolysaccharides, and Innate Immunity in the Pathogenesis of Obesity and Cardiovascular Risk. Endocr Rev. 2010;31(6):817-44. PubMed PMID: 20592272. 16. Gregor MF, Hotamisligil GS. Inflammatory Mechanisms in Obesity. Annu Rev Immunol. 2011;29(1):415-45. PubMed PMID: 21219177. 17. Dasu MR, Jialal I. Free Fatty Acids in the presence of High Glucose Amplify Monocyte Inflammation via Toll-like Receptors. Am J Physiol Endocrinol Metabol. 2010 October 19, 2010. 18. Samuvel DJ, Jin J, Sundararaj KP, Li Y, Zhang X, Lopes-Virella MF, et al. TLR4 Activation and IL-6Mediated Cross Talk between Adipocytes and Mononuclear Cells Synergistically Stimulate MMP-1 Expression. Endocrinology. 2011 December 1, 2011;152(12):4662-71. 19. Wong SW, Kwon M-J, Choi A, M.K, Kim H-P, Nakahira K, Hwang D. Fatty Acids Modulate Toll-like Receptor 4 Activation through Regulation of Receptor Dimerization and Recruitment into Lipid Rafts in a Reactive Oxygen Species-dependent Manner. J Biol Chem. 2009;284(40):27384-92. 20. Hotamisligil GS, Erbay E. Nutrient sensing and inflammation in metabolic diseases. Nat Rev Immunol. 2008;8:923-34. 21. Wen H, Gris D, Lei Y, Jha S, Zhang L, Huang MT-H, et al. Fatty acid-induced NLRP3-ASC inflammasome activation interferes with insulin signaling. Nat Immunol. 2011 05//print;12(5):408-15. 22. Barker BR, Taxman DJ, Ting JPY. Cross-regulation between the IL-1β/IL-18 processing inflammasome and other inflammatory cytokines. Curr Opin Immunol. 2011 10//;23(5):591-7.