Program Effort Index for Maternal and Neonatal
advertisement

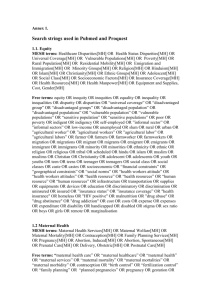
Program Effort Index for Maternal and Neonatal Health (MNPI) Round II - 2002 Maternal mortality continues to be high in many developing countries, reflecting the lack of good, widely available, treatment for emergency complications. Programs to improve these conditions depend upon highly specific measures such as the treatment of hemorrhage and obstructed labor, as well as upon the background factors of policies, training, and logistics. An index of effort that captures these program features, can document the low levels that now exist, and create a baseline to trace future improvements. Such an index, developed for family planning, has been used since the early 1970s and has proven useful to show both levels and trends, as well as regional differences, for different types of effort. It covers policies and regulations, various service arrangements, monitoring and evaluation, and contraceptive provision. It gathers data through questionnaires sent to various types of respondents in about 100 developing countries. A 27 year period has now been covered, in five rounds of investigation (1972, 1982, 1989, 1994, and 1999). Similar to the family planning program effort scores, an index was developed for HIV/AIDs programs. Known as the AIDS Program Index (API), it covers ten features, each with a number of detailed items. The index was applied to 40 countries in 2000, providing profiles of effective international and national program effort and measuring availability of key prevention and care services. In this document we present an overview of the Maternal and Neonatal Program Effort Index (MNPI) used to measure effort levels and program inputs for maternal mortality/morbidity and closely related neonatal health concerns. This index is based on the extensive work during the last two decades on the causes of maternal mortality and the necessary pathways of program action to reduce it. 1 Key sources in the literature include the following: Guidelines for Monitoring the Availability and Use of Obstetric Services, issued in 1997 jointly by UNICEF, WHO, and UNFPA. Indicators for Reproductive Health Program Evaluation: Final Report of the Subcommittee on Safe Pregnancy, issued in 1995 by the EVALUATION Project under USAID support. The Design and Evaluation of Maternal Mortality Programs, issued in 1997 by the Center for Population and Family Health, Columbia University. Estimates of the actual level of maternal mortality have also been refined, with appropriate qualifications for the poor quality of data available, in Revised 1990 Estimates of Maternal Mortality: A New Approach by WHO and UNICEF, issued in 1996 by WHO. The analyses in these publications are the basis for much of the index presented here. The index contains items for the most proximate determinants of maternal survival, those related to emergency obstetric and abortion cases, as well as the less proximate determinants of the policies and institutional arrangements necessary to build up capacities for emergency treatment. Purpose and Uses The purpose of this index is to measure program inputs and strength of effort for the reduction of maternal mortality and morbidity and closely related neonatal items. There are five uses: Description: 1) To measure the level of effort within each country, by type of effort. 2) To measure change over the past three years for each type of effort. Diagnosis: 3) To provide a diagnostic tool, to identify areas of strength and weakness. Planning: 4) To document program effort (by type and level) by country and by geographic region, for planning purposes for national and international agencies. 2 Stimulus: 5) To encourage both policy and program improvements, by showing inadequacies of effort, by type. Conceptual Framework Figure 1 shows the conceptual framework for the relationship between maternal/perinatal health program effort and the improved health outcomes. This framework is taken from “Indicators for Reproductive Health Program Evaluation: Final Report of the Subcommittee on Safe Pregnancy” (The EVALUATION Project, 1995). The inputs (col.1) are the social/cultural and individual factors, political and administrative system, and the organizational structure of safe pregnancy services. Despite the influence that social/cultural and individual factors have on maternal and perinatal mortality, these factors are beyond the control of the program. Therefore, for the purposes of evaluating maternal/perinatal program effort, the index has been designed to assess only the political and administrative system, and the organizational structure of safe pregnancy services. Similarly, for assessing the process and outputs of the program (cols.2 and 3), pregnancy status and service demand are distant determinants of maternal/perinatal health, and are outside of the scope of the program. Therefore, to assess the process and the outputs of the program, only safe pregnancy service operations and service outputs (e.g. quality and access) are measured. Reading across the columns under “Supply”, the political and administrative system and the organizational structure will strongly affect operations and, in turn, service outputs. Those, in turn, will have a direct effect on the health of women and newborns (col.4). The Maternal Neonatal Program Index (MNPI) is intended to measure the effort put into reduction of the maternal/neonatal mortality rate. It does not measure the social/cultural or individual context, nor does it measure the outcomes. The index is designed to assess only the inputs, process and outputs as they relate to the “Supply” or program side of the conceptual framework. 3 Figure 1. Conceptual Framework of Safe Pregnancy Program Demand and Supply: Program Impact on Maternal/Perinatal Mortality and Improved Health Demand Societal/cultural and individual factors Education; SES Women’s health status Women’s nutritional status Genetic risk Cultural factors Value for women and newborn Demand for children Pregnancy Status Wantedness Complicated Health related behaviors Costs Transport Service Demand Normal status Complications status (recognition) Family decision-making Reduced maternal & perinatal/neonatal mortality Appropriate Service Use Supply Political & administrative system Political support Resource allocation Legal code and regulations Organizational structuresafe pregnancy services* Service infrastructure Sectoral integration Delivery strategies Public/private partnerships Operations – safe pregnancy services* Management/supervision Training Commodity acquisition/ distribution IEC Research and evaluation Alarm and transport Service outputs Available access (transport) Quality Image/acceptability Efficiency Improved health of women and newborns (Health Impact) INPUTS PROCESS OUTPUTS OUTCOMES *Prenatal care, Essential Obstetric Care (EsOC), Special Neonatal Care (NSC) Source: Indicators for Reproductive Health Program Evaluation: Final Report of the Subcommittee on Safe Pregnancy. The EVALUATION Project. 1995. 4 Methodology The MNPI (Maternal Mortality and Neonatal Program Index) is a composite indicator, made up of individual items grouped into key categories. Each item is scored on a scale of 0-5, by persons conversant with each country program, following the “informed respondent” approach of the family planning and HIV/AIDs methodology. To obtain a range of viewpoints and information these persons are selected from numerous backgrounds and organizations, including the Ministry of Health, other Ministries, NGOs, donor representatives, academic and community-based groups, and others. The rule however is to choose persons who are sufficiently close to the nationwide program to provide valid responses to the questionnaire. To implement the study, a consultant is chosen in each country, who is then instructed to identify 10 to 25 respondents, provide the questionnaire to them with explanations, receive the questionnaires back, and send them to the Futures Group for analysis. To provide a measure of change, each respondent will be asked to rate each item twice, once for the current situation (for 2002) and once for three years ago, i.e., 1999. Results from the API survey mentioned above support the reliability of this retrospective technique. Three years is selected as a compromise: change cannot probably be detected for just one or two years ago, and five years is probably too long. It is important to measure items at the final service level, such as capacity for dealing with hemorrhaging or obstructed labor. However it is also important to measure the less proximate features of policies, resources, training, etc. since they are vital to creating improvements in the field. Scores for the individual items are combined within each category to produce sub-set and total scores. These will provide a profile of program effort for each country. 5 References Graham, W. 1997. “A Question of Survival? A Review of Safe Motherhood.” Ministry of Health, Kenya. Koblinsky, Marge, Katie McLaurin, Pauline Russell-Brown, and Pamina Gorbach. 1995. Indicators for Reproductive Health Program Evaluation: Final Report of the Subcommittee on Safe Pregnancy. The EVALUATION Project. Issued by Carolina Population Center. Maine, Deborah. 1991. Safe Motherhood Programs: Options and Issues. New York: Columbia University Center for Population and Family Health. Maine, Deborah, Murat Z. Akalin, Victoria M. Ward, and Angela Kamara. 1997. The Design and Evaluation of Maternal Health Programs. New York: Columbia University, Center for Population and Family Health. Nunez, Cesar A., Patricio Murgueytio, and John Stover. 1998. “The AIDS Policy Environment score: Measuring the Degree to which the Policy Environment Supports Effective Policies and Programs for HIV/AIDS Prevention, Treatment and Care: 1998 Follow-up Results.” Guatemala City: The Futures Group International. Strong, M.A. 1992. “The Health of Adults in the Developing World: The View from Bangladesh,” Health Transition Review, 2(2):215-224. Tsui, Amy O., J.N. Wasserheit, and John G. Haaga, eds. 1997. “Healthy Pregnancy and Childbearing,” in Reproductive Health in Developing Countries: Expanding Dimensions, Building Solutions. Washington, DC: National Academy Press. UNICEF. 1996. Progress of Nations. New York: UNICEF. UNICEF, WHO, AND UNFPA. 1997. Guidelines for Monitoring the Availability and Use of Obstetric Services. New York: UNICEF. World Health Organization. 1997. “Coverage of Maternal Care: A Listing of Available Information, Fourth Edition.” Geneva: WHO. World Health Organization. 1997. “Mother-Baby Package Costing Spreadsheet” (unpublished), Geneva: WHO. World Health Organization. 1996. Revised 1990 Estimates of Maternal Mortality: A New Approach by WHO and UNICEF. Geneva: WHO. 6