Plans

加護醫學部標準病歷範本
一
.
【
Acute pancreatitis
】
Chief complaint: sudden onset of abdominal pain for 1 day
Present illness:
A 42-year-old woman with no medical history presented to our emergency department complaining of 24 hours of severe nausea and vomiting. She had experienced similar painful episodes in the past, usually in the evening after a heavy meal, which always resolved spontaneously within an hour or two. This time, the pain did not improve and was associated with dyspnea, so she sought medical attention.
On physical examination, she was afebrile and tachycardic with a heart rate 104 bpm, blood pressure 95/74mmHg, and shallow respirations 26 breaths per minute. She shifted around on a stretcher feeling uncomfortable. Her skin was warm and diaphoretic and she had scleral icterus. Her abdomen was soft and mildly distended with marked right upper quadrant and epigastric tenderness to palpation; hypoactive bowel sounds were present; no mass was noted. Her stool was negative for occult blood. Laboratory studies showed total bilirubin
9.2g/dL with a direct fraction of 4.8g/dL, alkaline phosphate 285 IU/L, AST 78 IU/L, ALT 92
IU/L and amylase 1249 IU/L. Her leukocyte count is 16500/mm3 with 82% polymorphonuclear cells and 16% lymphocytes. A plain film of the abdomen showed a nonspecific gas pattern and no pneumoperitoneum. An abdominal CT revealed common bile duct stones and the pancreatic parenchyma was slightly heterogeneous without surrounding fluid accumulation.
Under the impression of acute pancreatitis, she was admitted to our ICU for further treatment and management.
Impression:
-
Acute pancreatitis
-
CBD stone
Plans:
(1) Diagnostic plan:
- Follow up amylase, lipase and liver function profile
(2) Therapeutic plan:
- Temporary NPO with IV hydration to correct hypovolemia
- Pain control and closely monitoring of possible peritoneal signs
- Consider IV form antibiotic use for possible secondary infection
(3) Educational plan:
- Bed rest and avoid over-activity
二
.
【
Acute pulmonary edema
】
主述 Shortness of breath for 2 days
現病史
This 81 year-old man has the history of hypertension, CAD s/p PTCA with regular follow up at our OPD.
According to this patient, he has suffered from shortness of breath after quick or long-distance walking. The shortness of breath became worse and persistent even while sitting in recent two days. Besides, paroxysmal nocturnal dyspnea, orthopnea and decreased urine output were also noted. There was no chest pain, nausea, vomiting, cold sweating or
URI symptoms. He was brought to our ED for help.
At ED, his lower limbs showed obvious edema. Physical examination revealed bilateral basilar rales on auscultation. The Lab data showed elevated BNP levels. The chest X-ray showed cardiomegaly and bilateral pulmonary consolidations, especially centrally distributed and acute pulmonary edema, were impressed. Under the impression of CHF with acute pulmonary edema, he was admitted for further management.
住院主要臆斷
1.
Congestive heart failure with acute pulmonary edema
鑑別診斷 : Pneumonia
住院診療計劃
診斷計畫 :
1. Arrange cardiac echo for heart function survey
2. Record I/O and check body weight qd
3. follow up chest x ray later
治療計畫
1.Oxygen supply and keep SaO2 or SpO2 higher than 90%
2. Diuretic treatment such as IV form Furosemide (Lasix) and monitor electrolytes
3. Nitroglycerin (Millisrol) IV infusion
4. Control blood pressure
衛教與告知計畫
1. Restrict fluid and sodium
2. Inform the risk of respiratory failure and the probability of ventilator support
三
.
【
Acute Stroke
】
Chief Complaint:
Sudden weakness of left limbs within 1 hour
Present Illnese:
The 58 y/o man has regular follow-up at OPD on CAD s/p stent, ESRD on H/D, HTN and DM.
The patient had sudden-onset of left-sided weakness at about 5 pm after taking a shower. Slurred speech and left facial weakness were also noticed. He was sent to our ER for help, where PE revealed left facial palsy of central type, slurred speech, and a decrease in muscle power of 1/1 in the LUL/LLL, compared to 5/5 in the RUL/RLL. The patient also felt numbness on the left side. Brain CT did not show ICH. After being informed of the indication and potential complications of r-TPA, the family agreed to r-TPA therapy. The r-TPA therapy increased the muscle power in the LUL/LLL to 4/4+. Thereafter, the patient was admitted to the ICU for post r-TPA care and further management for acute ischemic stroke.
Impression
1.Acute cerebral ischemic stroke with left-sided hemiparalysis
Plans
1.Diagnostic plan:
1.Stroke risk factors workup, including lipid profile & carotid echography
2.Arrange brain MRI+DWI+MRA for lesion localization
2.Therapeutic plan:
1.Antiplatelet therapy for prevention of recurrent stroke
2.Adequate IV hydation for maintainence of cerebral perfusion
3.Educational plan:
1.Inform the prognosis of acute stroke
2.DM, HTN education
四
.
【
Acute myocardial infarction
】
主述
Chest pain since this early morning
現病史
This 50 year-old male patient has history of type 2 DM without regular control. He has developed sudden onset of chest pain with cold sweating when he woke up in the early morning. According to the patient, his chest pain was located in the precordial area with a squeezing and compression sensation and the duration was over 30 minutes. Other associated symptoms included cold sweating and soreness radiating to the lower jaw and left shoulder.
He was brought to our ED this morning at 7:00. On physical examination, a regular heart beat, a systolic murmur of grade 2/6 over apex, and mild basilar rales in the bilateral lower lung fields were heard; blood pressure was 150/80mmhg; heart rate was 100 beats per minute; respiratory rate was 24 per minute. A series of examinations were done at ED. A 12-lead ECG showed sinus rhythm with 2mm horizontal ST-T segment elevation in leads V1-V4. Chest X ray showed cardiomegaly and mild pulmonary congestion. Elevated cardiac enzymes were also noted. He was admitted to the ICU for intensive care under the impression of acute myocardial infarction.
個人病史
1. Alcohol: denied
2. Smoking: 2 PPD for 30 years
3. Drug abuse: no drug abuse
CAD risk factors:
1. HTN(-)
2. DM(+)
3. old Age(+)
4. Family history of premature cardiovascular disease(-)
5. Smoking (+)
6. Male(+)
7. Dyslipidemia(?)
Food or drug allergy:(-)
住院主要臆斷
1.
Acute myocardial infarction, ST elevation type
住院診療計劃
診斷計畫 :
1. Arrange cardiac catheterization for primary PTCA
2. Check lipid profile and HbA1c
3. Follow-up cardiac enzyme and EKG
4. Arrange cardiac echo for heart function survery
治療計畫
1.Anticoagulant therapy with Heparin
2. Dual antiplatelet treatment
3. Nitrate infusion with Millisrol
3. Control heart rate with Propranolol (Inderal) (10mg) 1# tid
4. Control blood pressure with Captopril (Capoten) (25mg) 0.25# tid
衛教與告知計畫
1. Quit smoking
2. DM education
3. Inform the complication of cardiac catheterization
五
.
【
Chronic obstructive pulmonary disease with acute exacerbation and impending respiratory failure
】
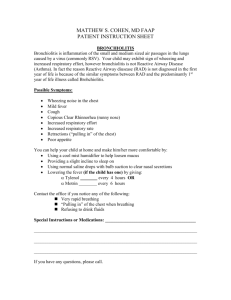
Chief complaint : Progressive shortness of breath and wheezing since this morning
This 62-year-old man, a chronic smoker with a smoking index of 30 pack-years, has history of chronic obstructive pulmonary disease for over 10 years without taking any medication. This patient stated that he has suffered from productive cough, progressive shortness of breath accompanied with wheezing, and an episode of near fainting for the past few days, so he came to our ER for help. In the ER, the patient’s respiratory rate was 32 /min, pulse rate was 136
/min, and blood pressure was 152/96 mmHg. Physical examination showed use of accessory respiratory muscle with the pattern of respiratory muscle recruitment during pursed lip breathing; chest auscultation disclosed bilateral expiratory wheezes; pulse oximetry showed
O2 saturation of 90%; chest film revealed no obvious opacity but showed bilateral emphysematous changes. So the patient received oxygen and inhaled bronchodilator therapy at ER. However shortness of breath and wheezing persisted. With the impression of chronic obstructive pulmonary disease with acute exacerbation and impending respiratory failure, the patient was admitted for further evaluation and treatment.
Impression : Chronic obstructive pulmonary disease with acute exacerbation and impending respiratory failure
Plan :
Diagnostic plan:
1. Collect sputum gram stain and culture, AFS and TB culture
2. Check atypical pneumonia titer
3. Arrange pulmonary function test
4. Survey for possible pneumonia
Therapeutic plan:
1. Oxygenation therapy
2. Bronchodilator inhalation
3.Empirical antibiotics
4. Systemic steroid use
5.Behavioral counseling
6.Diet adjustment to low carbohydrate and high lipid diet
六
.
【
Diabetic Ketoacidosis or Hyperglycemic Hyperosmolar Syndrome
】
Chief complaint: conscious disturbance in this morning.
Present illness:
This 18-year-old girl was brought to our emergency department by her mother because of confusion and queer behavior. The patient has always been healthy and has no significant medical history. However, she has weight loss of 2 kilograms in recent two weeks. Besides, she also has a sensation of thirst, drinks a lot of water, and has nocturia in these two weeks.
This morning, she developed abdominal pain and vomiting and seemed confused, according to her mother’s description.
On physical examination, she was afebrile and had a heart rate of 122 bpm, blood pressure of 125/84mmHg, and respiratory rate of 28 breaths per minute. Her oral mucosa was dry and her neck veins were flat. Her chest was clear on auscultation and her heart was tachycardic with a regular rhythm but no murmur. Her abdomen was soft with active bowel sounds and mild diffuse tenderness but no guarding or rebound tenderness. Her neurological examination revealed no focal deficits.
Laboratory studies showed Na 131mEq/L, K 5.3mEq/L, Cl 95mEq/L, BUN 35mg/dL, creatinine 1.3mg/dL, glucose 475mg/dL and ketone 2+. Arterial blood gas revealed pH 7.12,
PCO2 24mmHg and PO2 95mmHg. Urine drug screen and urine pregnancy test were negative; urinalysis showed no hematuria or pyuria but glucose 3+ and ketones 3+. Chest radiography was normal, and plain film of the abdomen had a non-specific gas pattern without signs of intestinal obstruction.
Newly diagnosed diabetes mellitus with diabetic ketoacidosis was impressed based on the symptoms of unintentional weight loss, nocturia and polyuria with hyperglycemia, ketoacidosis with dyspnea. Hence, she was admitted to our ICU for further treatment and management.
Impression:
1.
Diabetic ketoacidosis
2.
Newly diagnosed diabetes mellitus, probably Type 1
Plans:
(1) Diagnostic plan:
- Survey the precipitating factors of DKA, such as insulin deficiency, infection or inflammation, ischemia or infarction, intoxication and iatrogenic use of steroid.
(2) Therapeutic plan:
- Control ketoacidosis with continuous intravenous insulin infusion
- Hydration to correct hypovolemia
- Correct electrolytes imbalance
(3) Educational plan:
- Diabetes care: recognize symptoms and signs of hypoglycemia, insulin injection, diet control, glucose monitoring etc.
七
.
【
Meningitis
】
Chief Complaint:
Fever and consciousness change in progression for 5 days
Present Illnese:
The 66 y/o man has type-2 DM for which he has been taking oral hypoglycemic agents for 10 years and hypertension with OPD follow up for 15 years. This time, he has fever, headache and progressive change in consciousness for 5 days. The character of headache was throbbing, associated with nausea and photophobia. Due to progressive lethargy, he was brought to our ER.
In our ER, vital signs included a blood pressure of 140/78 mm Hg, a temperature of 38.4
Celsius degree, a pulse rate of 110 beats/minute and a respiratory rate of 16/minute. On neurologic examination, Kernig's and Brudzinski's signs were negative. His neck was stiff.
Fundoscopy showed papilledema. Brain CT scan did not reveal intracranial hemorrhage nor any space-occupying lesion. Blood tests showed leukocytosis and bandemia. Biochemical tests showed elevated CRP level and impaired lever and renal functions. The chest roentgenogram showed increased infiltration over bilateral lung fields. The cerebral spinal fluid (CSF) was obtained by lumbar puncture with an opening pressure of 22 cm H
2
0 and it was cloudy in appearance and yellow in color. Further CSF analysis showed RBCs of 760
/mm
3
, WBCs of 1,632/mm
3
, lymphocytes of 3%; neutrophils of 97%, total protein > 500 mg/dL, and glucose of 118 mg/dL. Gram stain revealed 3+ gram-negative bacilli; CSF acid-fast stain, india ink stain, fungal culture, and cryptococcal antigen were all negative;
VDRL was non-reactive.
The patient was admitted for further treatment and evaluation for bacterial meningitis.
Impression
1.Bacterial meningitis with severe sepsis
Plans
1.Diagnostic plan:
1.Consider brain MRI for identifying brain abscess or encephalitis if any
2.Pending blood and CSF cultures
2.Therapeutic plan:
1.Empirical antibiotics use
2.Hemodynamic support
3.Close monitoring conscious level
3.Educational plan:
1.Inform the possible etiology and prognosis of meningitis
2.Explain the possible etiology of conscious disturbance
八
.
【
Pneumonia with impending respiratory failure
】
Chief Complaint : Progressive shortness of breath and productive cough for 10 days
Present Illness: This 82 year-old man has history of dementia and ischemic cerebrovascular accident and has been bedridden for over 3 years. He lives in a nursing home with complete dependent for daily activities. According to his family and nursing home caregiver, the patient suffered from progressive shortness of breath and productive cough for 10 days. He also developed intermittent fever, chillness and general weakness, was in a drowsy state of consciousness, and had poor digestion and constipation. This morning when he was in the nursing home, low blood pressure (98/43 mmHg) was recorded and his conscious level deteriorated. Therefore the patient was brought to our ER for help. His family and caregiver denied choking, nausea or vomiting. At ER, the patient’s respiratory rate was 32 /min with a rapid shallow respiratory pattern, pulse rate was 135 /min Af with RVR, and blood pressure was 102/53 mmHg. His chest X-ray showed increased infiltration in the right lower lung field; chest auscultation disclosed bilateral crackles; laboratory tests disclosed leukocytosis and revealed band form, acute and chronic renal failure, and hypokalemia. ABG showed a decreased P/F ratio. Therefore with the impression of sepsis with infection focus of pneumonia, the patient was admitted for further evaluation and treatment.
Impression : Pneumonia with impending respiratory failure
Plan :
Diagnostic plan:
1. Collect sputum gram stain and culture, AFS and TB culture
2. Check atypical pneumonia titer
3. Collect urine for analysis
4.Follow up ABG and electrolyte
5.Check cortisol level
Therapeutic plan:
1. Empirical antibiotics
2. Close monitor respiratory pattern and homodynamic change
3. Fluid hydration
4. Mucolytic agents use
5. Chest physical therapy and postural drainage
6. Steroid use
九
.
【
Upper gastrointestinal bleeding
】
Chief complaint: passage of tarry stools for 1 day
Present illness:
This 37-year-old man with a history of hypertension presented to our emergency department due to passage of tarry stools for 1 day. He complained of an increase in frequency and severity of burning epigastric pain, which he had experienced occasionally for more than 3 months. The pain occurred 2-3 times per week, usually when he had an empty stomach and it was relieved within minutes by food or antacids. Because of increased amount of tarry stools associated with dizziness and palpitations, he came to our emergent department for help.
On physical examination, he was afebrile and had a heart rate 121 bpm, blood pressure
99/74mmHg, and respiratory rate 24 breaths per minute. His conjunctiva was pale, oral mucosa was dry and her neck veins were flat. His chest was clear to auscultation and his heart was tachycardic with a regular rhythm and no murmur. His abdomen was soft with active bowel sounds and mild tenderness in the epigastric region without muscle guarding or rebound tenderness. Laboratory studies revealed normocytic anemia with Hb 7g/dL, platelet
135K/uL, Na 138mEq/L, K 4.2mEq/L, BUN 34mg/dL, creatinine 1.3mg/dL, glucose
98mg/dL. Blood transfusion was given to correct the anemia and the panendoscopy was also arranged for further evaluation.
Under the impression of upper gastrointestinal bleeding, the patient was admitted to our ICU for further treatment and management.
Impression:
3.
Upper gastrointestinal bleeding
Plans:
(1) Diagnostic plan:
- Arrange the panendoscope for further evaluation
(2) Therapeutic plan:
- Fluid hydration to correct hypovolemia
- Temporary NPO with PPN
- PRBC transfusion to correct anemia
- PPI agent use, if PUD diagnosed by panendoscope
(3) Educational plan:
- Bed rest and avoid over-activity
十
.
【
Urosepsis
】
Chief complaint: Fever and conscious disturbance since last night
Present illness:
This 84-year-old woman, a bedridden nursing home resident with history of cardiovascular accident, was brought to our emergency department due to confusion and fever since last night. Her Glasgow Coma Scale was E2V3M5 and vital signs were as follows: temperature 38.5 degree Celcius, heart rate 130 beat per minute, blood pressure 76/32mmHg, respiratory rate 26 breaths per minute, and oxygen saturation 95% on room air.
On physical examination, she was lethargic but agitated when disturbed, her neck veins were flat, her lung fields were clear and her heart rhythm was tachycardic but regular with no murmur or gallops. Abdominal examination was unremarkable and her extremities were cold with poor skin turgor.
After administration of 2L of normal saline for more than 1 hour, her blood pressure increased to 90/57 mmHg. The initial laboratory studies revealed white blood cell count of
14000/mm3 with 78% neutrophils, 5% bands and 13% lymphocytes; no other abnormalities were noted. No abnormality was noted on Chest x-ray. Urinalysis showed pyuria, bacteria 2+, leukocyte esterase 2+ and nitrite +.
Under the impression of urosepsis, the patient was then admitted to our ICU for further intensive care and management.
Impression: Urosepsis
Plans:
(1) Diagnostic plan:
- Collect blood and urine cultures
- Arrange abdominal echography to exclude any renal stones or
hydronephrosis
(2) Therapeutic plan:
- hemodynamic support with intravenous fluids or vasopressors as necessary
- broad-spectrum antibiotic with Fortum for infection control
- stress ulcer prophylactic treatment with proton pump inhibitor for 3 days
- closely follow up consciousness, respiratory pattern and oxygen saturation
(3) Educational plan:
- Bed rest and fall prevention. Prevention of unplanned removal of catheters.