Mandibular tumors
advertisement

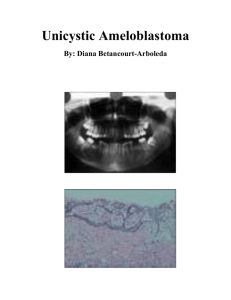
Mandibular tumours Mandibular defect classification Boyd’s HCL classification H defects are lateral and of any length including the condyle and do not cross the midline. L defects are as above but don't involve condyle C defects consist of the entire central segment containing the four incisors and the two canines Combination exist i.e. angle to angle defects LCL o- neither skin nor mucosal defect s - skin defect m - mucosal defect sm - skin and mucosa Challenges Soft tissue Reconstruction Only In the past, L and H defects were reconstructed with soft tissue closure Unopposed muscle pull on unresected remnant causes swing to the resected side, leads to cross bite. This reduces the defect size but also leads to abnormal dental wear, caries, loss of function or concave appearance on the unaffected side Central Segment reconstruction Anterior arch defect - greatest aesthetic and functional problem and difficult surgical challenge Frequently results in lip and chins ptosis in which the soft tissue slides of the reconstructed arch producing eversion of the lower lip and salivary incontinence. Mandible tends to be pulled superiorly, especially in the edentulous which is not limited by occlusion: 1. Unopposed masseter and pterygoid action The C segment has 4 mouth opening muscles (digastrics and geniohyoid) attached to it. When c segment resected these muscle attachment is lost or muscle lost in ablative procedure. . The mandible is then free of its anterior muscular tethering and is pulled upward by the unopposed action of the masseter and the pterygoids. When not possible to preserve the C segment it is occasionally feasible to reattach the submental muscles to the reconstructed mandible 2. Chin Degloving Mentum soft tissue degloving should be reattached to avoid witch’s chin deformity 3. Lower facial nerve paralysis Bilateral neck dissections often result in damage the lower branches of the facial nerve on both sides and exacerbates the lip ptosis. 4. Soft tissue contraction If during reconstruction the floor of mouth dead space is not adequately filled with soft tissue the resulting contracture tends to distort the new bony reconstruction or draw the soft tissue inferiorly thus resulting in inferior displacement. Mandibular pathology Physiology Amoloblasts – secrete enamel Odontoblast – secrete dentin Cementoblasts – secrete cementum Fibroblast – periodontal membrane Neural crest forms nearly all components of teeth - dentin, pulp, periodontal ligament and cementum, except enamel (develops from ectoderm) Enamel o acellular (96% mineral), tapers off at the cementoenamel junction o dependant on underlying dentin for support Dentin o 70% mineral o Occupied by odontoblasts which secrete matrix and also mediate sensation Pulp o Odontoblasts to make dentin o Nutrition o Sensation Cementum o Calcified connective tissue covering the anatomic root o Anchors the periodontal ligament to the root of the tooth o Continuous cementum deposition maintains length of the tooth as compensation for occlusal wear o May be acellular or contain cementoblasts Symptoms and signs 1) Swelling (fibrous dysplasia, cherubim, cysts and cancer) 2) pain (osteoradionecrosis, osteomyelitis and invasive cancer) 3) Numbness (neoplastic invasion of the V3) 4) Loosening of teeth (weakness of the socket by disease processes) 5) Oral mucosal involvement (mandibular sarcomas breaking out, mucosal carcinomas breaking in, osteoraionecrosis causing inflammation breakdown and bone exposure Tumours of the mandible Classification (Kramer) 1) Odontogenic a. Cysts i. Epithelial 1. radicular (periapical) cyst(55%) 2. dentigerous cyst (24%) 3. residual cyst (20%) 4. keratocyst (5%) b. Benign Tumors i. Epithelial 1. ameloblastoma (11%) 2. calcifying epithelial odontogenic tumor 3. adenomatoid odontogenic tumor ii. Mesenchymal 1. myxoma (3%) 2. benign cementoblastoma 3. odontogenic fibroma iii. Mixed 1. ameloblastic fibroma 2. ameloblastic fibroodontoma 3. odontoma c. Malignant Tumors i. Epithelial 1. malignant ameloblastoma ii. Mesenchymal 1. ameloblastic sarcoma 2) Nonodontogenic a. Cysts i. Epithelial 1. fissural median mandibular cyst ii. Nonepithelial 1. traumatic bone cyst 2. aneurysmal bone cyst b. Benign Tumors 1. Fibrous dysplasia 2. cherubism 3. giant cell granuloma 4. osteoma c. Malignant i. Primary 1. osteosarcoma 2. chondrosarcoma 3. central mucoepidermoid carcinoma 4. Burkitt’s lymphoma ii. Secondary 1. metastatic carcinoma 2. SCC Odontogenic tumors radiographic features Radiolucent Lesions 1. ameloblastoma 2. ameloblastic fibroma 3. odontogenic fibroma 4. odontogenic myxoma 5. squamous odontogenic tumor 6. clear cell odontogenic tumor Radiolucent with or without Radiopacity Lesions 1. adenomatoid odontogenic tumor 2. calcifying epithelial odontogenic tumor Radiopaque with or without Radiolucency Lesions 1. odontoma 2. ameloblastic fibro-odontoma 3. ameloblastic odontoma Odontogenic Cysts Radicular cysts (apical cyst) Most common cyst of jaw (55% of cysts) Response to apical inflammation may have sinus tract to oral mucosa or even skin Radiographic features Pulpless nonvital tooth Small well defined periapical lucency Treatment Extraction, root canal Low recurrence rate Dentigerous cyst 25%of odontogenic cyst Peak incidence in 2nd and 3rd decades Fluid between reduced enamel epithelium and tooth crown Surrounds unerrupted second and third molars. Cysts have epithelial lining and vary from 2cm to expansible mass May cause displacement of teeth and facial asymmetry Can be locally destructive Radiographic features well-demarcated radiolucent lesion attached at an acute angle to the cervical area of an unerupted tooth Treatment and prognosis Enucleation or marsupialization. 6% recur Possible malignant transformation – 20% of ameloblastomas arise from these cysts, also SCC and mucoepidermoid tumor Keratocysts 5% of all jaw cyst third most common odontogenic cyst and belongs in the differential diagnoses of any radiolucency of the jaws. Affect all ages with peak in 2nd 3rd decade M>F 50 % around third molar and ascending ramus different from other cysts; they are aggressive and can be difficult to remove. OKCs can grow quite rapidly, and recurrences are frequent - grow in a multilocular bosselated fashion with daughter cysts that extend into the surrounding bone. cysts are formed with a stratified squamous epithelium 5% have basal cell nevus syndrome, also known as Gorlin syndrome hypertelorism, midface hypoplasia, relative frontal bossing and prognathism, mental retardation, multiple basal cell carcinomas, calcification of the falx cerebri, bifid ribs, palmar pitting (the pits later develop into basal cell carcinoma), and multiple OKCs. Multiple OKCs are diagnostic for basal cell nevus syndrome until proven otherwise. autosomal dominant inheritance and high penetration Radiographic features Mimics many cysts Multiloculated with scalloped radiopaque borders Marked cortical thinning and root resorption Treatment Enucleation with curettage for small cyst aggressive and can be difficult to remove 60% recurrence with incomplete excision Residual cysts Incidence and features Any odontogenic cyst that persists in bone after tooth is removed 20 % of odontogenic cysts Clinical Static or slowly enlarging asymptomatic or painful with inflammation Etiology From epithelial remnant of periapical granuloma (root abscess) Radiol Well circumscribed cyst in endentulous area Treatment Enucleation with low recurrence rate Non-odontogenic Cysts Fissural: median mandibular cyst Rare; nonaggressive thought to be derived from epithelium entrapped in the lines of fusion of the body process that forms the jaw and face Cysts are line with stratified squamous epithelium and respiratory epithelium. Midline symphyseal Controversial from trapped epithelial remnants of mandibular arch fusion vs. peri odontal cyst Nucleation; uncertain of prognosis due to rarity of lesion Traumatic bone cyst Features and incidence Empty or fluid filled cavity associated with jaw trauma(50%) Location Mostly anterior mandible but also molar area Clinical Presentation Size extremely variable aymptomatic and found on routine associated with labial or buccal expansion teeth remaining vital Etiology Trauma with intramedullary hematoma Radiographic Smooth radiolucency with scalloped borders extending roots Treatment and Prognosis May resolve spontaneously curettage with possible bone grafting of low recurrence rate. Aneurysmal bone cyst Incidence Rare in mandible benign expansile lytic lesion Location Body of mandible Clinical presentation Pain and swelling growth rate variable Etiology Possibly traumatic origin with localized alteration in hemodynamics or persistent connection between damaged vessels and hematoma possibly AV fistula Expansile eccentric cyst with thin cortices; soap bubble or honeycomb appearance Large vascular sinusoids (no bruit) Radiographic Multilocular radiolucency with cortical expansion Treatment Curettage or excision. Recurrence rare Odontogenic epithelial tumours Ameloblastoma may develop from any of the epithelial elements (e.g. dentigerous cyst, enamel organ, peridontal membranes) benign but locally invasive most common odontogenic tumor (11%) peak incidence 4th – 5th decade Propensity for rapid disfiguring growth and late recurrence Location 80% in mandible, 20% in maxilla Most commonly in molar area Often associated with unerupted third molar Clinical features Slow growing painless swelling with or without a soft tissue mass Size range from 1-16 cm Large lesions can cause facial asymmetry or displaced teeth and malocclusion Can expand bone erode through it or produce pathological fracture Radiology Classic appearance – multilocular (soap bubble) radiolucency of posterior mandible 3 types 1. Unilocular (13%) o Round or ovoid appearance with no calcified or radioopaque components distinct border with slight marginal sclerosis, may have scalloped margins ; no periosteal reaction. o Often confused with odontogenic cysts 2. Multilocular (86%) o Honeycomb or soap bubble appearance ; marked expansion with cortical thinning and bony destruction 3. Peripheral (extraosseous – 1%) Treatment Curettage or enucleation not recommended due to 90 % recurrence partial mandibulectomy or segmental resection with margins of normal bone recommended( recurrence rate -5% ) Radiotherapy palliative for unresectable tumours Mets rare Calcifying epithelial odontogenic tumours(Pindborg tumour) Incidence /Features Rare, locally aggressive tumour; 2% of odontogenic tumours Bimodal incidence Occurs in third to fourth decades Location Usually in Premolar and Molar area (in contrast to ameloblastoma) Many associated with unerupted teeth Radiology Chief sign is cortical expansion in all directions Radiolucent; poorly defined, noncorticated borders Unilocular, multilocular, or “moth-eaten” Driven-snow” appearance from multiple radiopaque foci Treatment Similar to ameloblastoma Up to 14% recurrence reported Adenomatoid odontogenic tumour A well-circumscribed lesion derived from odontogenic epithelium that usually occurs around the crowns of unerupted anterior teeth of young patients consists of epithelium in swirls and ductal patterns interspersed with spherical calcifications. Incidence Rare nonaggressive tumour F>M 2:1 age <20 Location anterior to canines and frequently associate with impacted or unerupted teeth may be associated with cortical expansion Clinical Presentation low growing asymptomatic mandibular swelling small 1.5 - 3 cm painless anterior tumour Radiology well-demarcated mixed radiolucent / opaque lesion often surrounds the crown of an impacted tooth Treatment and prognosis Conservative excision; low recurrence rate Odontogenic mesenchymal tumours Myxoma (fibromyxoma) Locally aggressive - 3% of odontogenic tumours primarily consisting of a mucoid ground substance with widely scattered undifferentiated spindled mesenchymal cells. Peak incidence in second and third decades Painless slow jaw enlargement Location Usually posterior mandible but rarely in condyle progressive swelling with bony expansion; can cause malposition of teeth Radiology Margins variably demarcated multilocular radiolucency soap bubble or honeycomb appearance Treatment and prognosis En bloc excision; recurrence rate - 25% Odontogenic mixed tumours Odontoma Features and incidence composed of aberrant tissue of all the dental elements likely a harmartoma Common All ages but mostly second decade Location Posterior mandible Usually less than 1cm +/- larger Clinical Most are symptomatic but swelling may interfere with tooth eruption From odontognic apparatus(i.e. Enamel, dentin and cementum) Radiology solid unilocular radiopaque mass surrounded by a thin radiolucent zone Treatment Early enucleation to prevent interference with tooth eruption Low recurrence rate Compound Odontoma Malignant Epithelial odontogenic tumors Compound Odontoma Malignant ameloblastoma Incidence and features Rare tumour classified as an odontogenic carcinoma Any age after first decade Most commonly in men >50 years Location Generally same as ameloblastoma Clinical Presentation History of multiple unsuccessful treatments of benign but persistent odontogenic epithelial lesion Pain swelling ulceration and paresthesia Regional lymphadenopathy with mets to lung, liver vertebrae Etiology Arises from residual odontogenic apparatus or from transformation of an odontogenic cyst or ameloblastoma Radiology Poorly defined radiolucency with gross expansion and thinned cortices Treatment Full ontological screening, radical excision Rare tumour thus ideal treatment difficult to define radiorx and chemo rx are used Poor prognosis Non Odontogenic Benign tumors Fibrous Dysplasia Found in membranous facial bones of younger individuals and becomes less active with maturity Incidence Uncommon First and second decades Features Fibro osseous lesion Developmental derangement due to undiffentiated mesenchymal bone forming cells replacing normal lamellar by woven bone Monostotic and polyostotic variants Polyostotic associated with Albrights Syndrome Location Common in maxilla Angle of mandible Usually progressive unilateral swelling with variable facial asymmetry Pain and decreased function with progressive deformity Dentition can be shifted Burns out after puberty Radiology Ground glass or orange peel appearance Poorly circumscribed with diffuse borders Pagetoid or cyst like appearance Treatment If required, definitive reconstruction when disease has burned out Earlier intervention with partial resection, ,curettage or bony contouring indicated for pain and functional loss. Rare malignant change post radio rx - thus not recommended Prognosis generally good Cherubism Features and incidence autosomal-dominant disorder of variable penetrance (100% penetrance in males) Bilateral symmetrical maxilla and mandible swelling Usually begins with eruption of secondary dentition (age 2-4) stabilizes after the growth period, usually leaving some facial deformity and malocclusion. Location Entire body and ramus with sparing of condoles Extends into alveolar process Clinical presentation Painless rapid early growth Alveolar involvement causes shedding of deciduous teeth Delayed eruption and malocclusion maxillary fullness produces retraction of the lower eyelids increasing scleral show causing “cherubic Appearance” Radiographic features Bilateral well defined multilocular expansile radiolucenices Becomes ground glass at end of growth Cortical thinning or absence Treatment Generally resolves with age Treatment individualized on amount of regression or deformity Good prognosis if limited to mandible Giant cell granuloma Incidence and features Uncommon 3-5% of benign jaw tumours Neoplastic like reactive proliferation - locally aggressive Multinucleated giant cells on histology Younger age groups Location Typically symphyseal and bicuspid regions Clinical Intermittent variable growth Pain may be dominant symptom Radiology Unilocualted or multiloculated well circumscribed Treatment Curettage of excision Recurrence rare with complete excision Osteoma exophytic nodular growth of dense cortical bone on or within the mandible or maxilla in locations other than those occupied by exostoses. benign skeletal neoplasm of unknown etiology that is composed of osteoid and woven bone. hamartomatous proliferation restricted to the craniofacial skeleton located either superficially or intraosseously classic presentation is that of focal bone pain at the site of the tumor. The condition worsens at night and increases with activity, and it is dramatically relieved with small doses of aspirin. often associated with Gardner syndrome Treatment surgically reducing osteoma to the level of the surrounding bone Gardners Syndrome Autosomal dominant with multiple osteomas, epidermal cysts, colon polyposis and pigmented lip macules Location Commonly lingual surface of mandibular body Attached to cortical bone by a stalk Treatment and prognosis Usually not required If symptomatic , local excision is sufficient with no risk of recurrence Non odontogenic Malignant (Primary) Burkitts Lymphoma Features and incidence Poorly differentiated B cell lymphoma Most common childhood malignancy in east Africa Mean age 7-9 yrs Rare in north America with mean age 11-12 yrs Fastest growing neoplasm Location 80% of tumours found in all four jaw quadrants Jaw less commonly involved in north American cases Clinical presentation Enlarges very rapidly shifting and exfoliating the teeth Associated with adrenal , kidney and gonadal masses Lymphadenopathy rare Aetiolgy Related to EBV Genetic association Link to malaria Treatment and Prognosis Chemotherapy 50 % relapse rate Poorer prognosis if gonadal involvement Non odontogenic malignant(secondary) Squamous cell Carcinoma Features and Incidence 30 % of head and neck cancers M:F 2:1 Increasing female incidence due to smoking Morphology 1. exophytic (best prog) 2. Ulcerative 3. Mixed Histological variants 1. Basiloid (worst variant) 2. Verrucous - 5% of oral SCCs (better prognosis) Location Commonly arises in mucosa of posterior alveolar ridge, but can spread from any part of the oral cavity including the lips 35 -50 % have bone invasion histologically and radiographically at the time of diagnosis Spread is through occlusal surface (gingiva and tooth socket) since the periosteum is considered an effective barrier to tumor spread May extend along inferior alveolar nerve 10 %of oral sccs arise at alveolar ridge Clinical 1. May present as an incidental finding or as advanced disease 2. Present with non healing ulcer, pain, loose tooth, poorly fitting dentures, difficulty with mastication or numbness in the inferior alveolar region 3. Weight loss common Risk factors 1. Smoking 6x risk 2. Betel chewing increased risk when combined with tobacco 3. Alcohol 6x risk 4. Alcohol plus tobacco 15x risk 5. Malnutrition, iron, vitamin a and C deficiencies 6. Solar exposure - lips 7. Viral 8. Poor dentition 9. Genetic Treatment Initial screening Hx and Ex Bx CXR and LFT Ct for nodal and distant disease MRI useful for soft tissue and perineural involvement Bone scan if bone pain Pan endoscopy Consultation 1. H and N team 2. Oncologist 3. Nutritionalist Modalities of treatment 1. Surgery 2. Radiotherapy 3. Chemotherapy 4. 50 % reduction in cure rate with nodal involvement 5. Prognosis generally poor