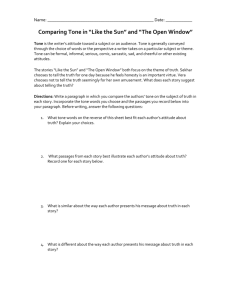
Evaluation of Motor Control and Coordination
advertisement

EVALUATION OF MOTOR CONTROL (Reference: Pedretti 6th ed, pp. 404-421, Trombly 5th ed, pp. ) INTRODUCTION Motor control – ability to make dynamic postural adjustments and direct body and limb movement in purposeful activity. Components necessary include normal muscle tone, normal postural tone and postural mechanisms, selective movement and coordination. Plasticity – anatomical and electrophysiological changes in the central nervous system. This makes motor relearning possible. Unmasking – use of existing neural pathways; believed that seldom-used pathways become more active after the primary pathway has been injured; adjacent nerves take over the function of damage nerves Sprouting – development of new neural connections ; dendrites from one nerve form a new attachment or synapse with another; new axonal processes develop Observation of movements during occupational performance followed by evaluation of specific components: muscle tone, postural tone and mechanism, reflexes, selective movement and coordination – the way to assess motor control UMNS (Upper Motor Neuron System) – includes any nerve cell fiber in the spinal cord (other than anterior horn cells) and all superior structures. These structures include descending nerve tracts and brain cells of both gray and white matter that subserve motor function. LMNS (Lower Motor Neuron System) – includes the anterior horn cells of the spinal cord, the spinal nerves, the nuclei and axons of cranial nerves III through X and the peripheral nerves. Dysfunction in this system results in diminished or absent deep tendon reflexes and muscle flaccidity. PERFORMANCE ASSESSMENTS *OTs are challenged of maximizing client’s ability to return to purposeful and meaningful occupation within his or her physical, cultural and social environment. Evaluating functional performance is primary in helping clients to set realistic goals. OTs can observe client during BADLs, IADLs along with productive and leisure activities. The OT must observe how problems in motor control affect performance. He must also consider the client’s sensation, perception, cognition, and medical status. The Canadian Occupational Performance Measure (COPM) Assessment tool that ensures client-centered therapy Helps prioritize the client’s functional activity goals in the areas of self care, leisure and productivity. The Test d’Evaluation des Membres Superieurs de Personnes Agees (TEMPA) An upper extremity functional activity performance test for clients. Developed to help therapists distinguish between normal and pathological aging in upper extremity performance. Some of the test items include picking up and moving a jar, writing on an envelope, tying a scarf and handling coins. The Graded Wolf Motor Function Test (GWMFT) (please see the attached form on your Pedretti 6th ed, pp. 407) A new assessment developed to measure functional gains after a hemiparetic event from cerebrovascular accident or traumatic brain injury. Based on the Wolf Motor Function Test. Was called “graded”, because there are two levels of difficulty for each task – Level A: more advanced; Level B: easier. A very useful test that can be used on a wide variety of clients with hemiparesis with varying degrees of motor recovery. More research is needed to confirm the validity and reliability of this test. The Wolf Motor Function Test (WMFT) Has been used to quantify the motor abilities of chronic clients from a population of high upper extremity function following CVA or traumatic brain injury. The Functional Test for the Hemiplegic/Paretic Upper Extremity Assesses the client’s ability to use the involved arm for purposeful tasks. Provides objective documentation of functional improvement and includes tasks ranging from those that involve basic stabilization, to more difficult tasks requiring fine manipulation and proximal stabilization. Examples include holding a pouch, stabilizing a jar, wringing a rag, hooking and zipping a zipper, folding a sheet and putting in a light bulb overhead. The Fugl-Meyer assessment Assessment is based on the natural progression of neurological recovery after CVA. Low scores have been closely related with the presence of severe spasticity. A quantitative assessment of motor functions following stroke and measures such parameters as ROM, pain, sensation and balance. The scores of this test correlate with ADL performance. The Arm Motor Ability Test (AMAT) A functional assessment of upper extremity function. Cutting meat, making a sandwich, opening a jar, and putting on a T-shirt are some of the tasks included in this test. The Motricity Index (MI) A valid and reliable test of motor impairment that can be performed quickly. The test assesses pinching a cube with the index finger and thumb, as well as elbow flexion, shoulder abduction, ankle dorsiflexion, knee extension and hip flexion. The Assessment of Motor and Process Skills (AMPS) A standardized test that assesses motor and process skills in IADLs. The test was created by OTs. A five day training course must be met by eligible OTs to become certified in the use of this test. Although the test is not diagnosis specific, it has been widely used with clients who have had a CVA. NORMAL MUSCLE TONE - component of the normal postural mechanism - a continuous state of mild contraction - a state of preparedness in a muscle - When present, a tension between the origin and insertion of a muscle is felt as resistance by the therapist when passively manipulating the limb. - High enough to resist gravity yet low enough to allow movement - Tension is determined partly by mechanical factors such as connective tissue and viscoelastic properties of a muscle and partly by the degree of motor unit activity. - When passively stretched, the normal muscle offers a small amount of involuntary resistance. - Relies on normal function of the cerebellum, motor cortex, basal ganglia, midbrain, vestibular system, spinal cord functions and neuromuscular system (including the mechanical-elastic features of the muscle and connective tissues) and on a normally functioning stretch reflex which is mediated by the muscle spindle. - Varies from one individual to another - Characterized further by the following: 1. Effective co-activation (stabilization) at axial and proximal joints 2. Ability to move against gravity and resistance 3. Ability to maintain the position of the limb if it is placed passively by the examiner and then released 4. Balanced tone between the agonist and antagonistic muscles 5. Ease of stability to shift from stability to mobility and reverse as needed 6. Ability to use muscles in groups or selectively with normal timing and coordination 7. Resilience or slight resistance in response to passive movement. Tone – the resistance felt by the examiner as he or she passively moves a client’s limb. It is dependent on the integrity of the peripheral and CNS mechanisms and the properties of muscle. ABNORMAL MUSCLE TONE Flaccidity - Absence of tone, deep tendon reflexes and active movement. - Results from spinal or cerebral shock immediately after a spinal or cerebral insult (traumatic UMNS lesion) and usually is present initially and then changes to hypertonicity within a few weeks. - Can also result from LMNS dysfunction such as a peripheral nerve injury or a disruption of the reflex arc at the alpha motor neuron level - Muscles feel soft and offer no resistance to passive movement. - If limb is moved passively, it will feel heavy. - If moved to a given position the released, the limb will drop because the muscles are unable to resist gravity. Hypotonus - Considered by many to be decreased of normal muscle tone (low tone) - Deep tendon reflexes are diminished or absent - Less than normal resistance to passive elongation - Van der Meche and Van der Gijn suggested that hyptotonus could be an erroneous clinical concept. They concluded in their study that if a client’s limb feels hypotonic or flaccid, it is the result of weakness and not long-latency stretch relexes. Hypertonus - Increased muscle tone - Can occur when there is a lesion in the premotor cortex, the basal ganglia and descending pathways. Damage to the UMNS increases stimulation of the LMNS, with a resultant increased alpha motor activity. Any neurological condition changing the UMN pathways may result in hypertonicity. Other spinal or brainstem reflexes may become hyperactive, which leads to hypertonus patterns like flexor withdrawal or the reemergence of tonic neck reflexes. - Occurs in synergistic neuromuscular patterns - Synergies are defined as patterned movement characterized by co-contraction of flexors and extensors. - There is a considerable energy cost in moving against hypertonicity and a loss of reciprocal inhibition between spastic and agonists and antagonists arises thus frustration and fatigue are commonly seen. Clients will also have dysfunction in spatial and temporal timing of movements making it uncoordinated. The architecture of hypertonic muscles also changes overtime. The muscles lose their ability to lengthen and shorten because of viscoelastic changes that resulted. - Can increase as a result of painful or noxious stimuli – pressure sores, ingrown toenails, tight elastic straps on a urine collection leg bag, tight clothing, an obstructed catheter, UTI, constipation, head position and fecal impaction. Other triggering factors include fear, anxiety, environmental temperature extremes, heterotopic ossification, and sensory overload. These stimuli can be reduced with good medical care and therapeutic intervention should be designed to reduce, eliminate and cope with these extrinsic factors. o Cerebral Hypertonia - Caused by TBI, stroke, anoxia, neoplasms (brain tumors), metabolic disorders, cerebral palsy and diseases of the brain. - Tone fluctuates continuously in response to intrinsic and extrinsic factors - Occurs in definite patterns of flexion and extension, causing the limb to be pulled in one direction - Typically the pattern occurs in the anti-gravity muscles of the upper and lower extremities (flexors=UE; extensors=LE) - The re-emergence of primitive reflexes and associated reactions alters postural tone. When the individual is lying supine, muscle tone is less than when the individual is sitting or standing. Tone is highest during ambulation. Thus attention to postural tone is important when positioning a client for splinting or casting. A cast or splint fabricated on a client in a supine position may not fit when the client is sitting up, because of the influence of gravity and posture on increasing muscle tone. o Spinal Hypertonia - Results from injuries and diseases of the spinal cord. - In slow-onset spinal diseases (e.g. spinal stenosis or tumors), there is no period of spinal shock. - In traumatic spinal cord injury, spinal shock occurs and is characterized by flaccidity. With time, the flaccidity diminished and hypertonus develops. The affected extremities first develop flexor and adductor tone. Overtime, extensor tone develops and becomes predominant in the lower extremities. - Can lead to muscle spasms severe enough to cause an individual to fall out of a wheelchair, off a gurney or out of bed. - The degree of hypertonicity in incomplete spinal cord lesions varies, depending on the degree of damage to the spinal cord. The tone tends to be more severe in incomplete spinal cord lesions than in complete lesions. Spasticity - Definition according to Lance: “a motor disorder characterized by a velocity-dependent increase in tonic stretch reflex (muscle tone) with exaggerated tendon jerks resulting from hyperexcitability of the stretch reflex as one component of the UMN syndrome.” - Little and Massagli believe that pure spasticity is a subset of hypertonia - 3 characteristics are as follows: 1. Hyperactivity of the muscle spindle’s phasic stretch replex with hyperactive firing of the IA afferent nerve 2. Velocity dependence, meaning the stretch reflex is only elicited by the examiner’s rapid passive stretch. 3. The “clasp-kinfe” phenomenon. This means that when the examiner takes the extremity through a quick passive stretch, a sudden catch or resistance is felt, followed by a release of the resistance. What actually happens is that the initial high resistance of spasticity is suddenly inhibited. - In a spastic muscle, there is a range of free movement, then a strong contraction of the muscle in response to stretch (i.e. stretch reflex) and free movement again when the muscle suddenly relaxes. This is the “claspkinfe” phenomenon or reflex. - Spasticity is not synonymous with hypertonicity. These two conditions are similar because they pull the limb into a unilateral direction. They are different in the following ways: 1. Hypertonia is typically not velocity-dependent; that is, rapid movement does not evoke it, rather, slowly joint movement elicits them. The hypertonus persists as long as the muscle stretch is maintained because of the firing of group II muscle spindle afferents (tonic stretch reflex) 2. During passive movement, there is no catch felt with hypertonia, as there is with clasp-knife phenomenon of spasticity. It is objectively measured with EMG. - In Trombly 5th ed, it was specifically pointed that Hypertonia is due to both neural and mechanical factors. The neural factor is spasticity which is due to hyperactive stretch reflexes. The mechanical factors of hypertonus are the elastic properties of connective tissue and the viscoelastic properties of muscle. The mechanical factors change if a muscle is immobilized in a shortened of lengthened position (i.e. there is increased or decreased resistance to passive elongation). The neural changes after CNS damage- spasticity – contribute to abnormal positioning of the limbs, which causes secondary changes in the mechanical factors. Together, the neural and mechanical factors account for increased resistance to passive elongation – hypertonus – that is seen after CNS damage. Clonus - A specific type of spasticity and is often present in clients with moderate to severe spasticity. - Characterized by repetitive contractions in the antagonistic muscles in response to rapid stretch. - There are recurrent bursts of IA afferent activity which result in a cyclical oscillation of phasic stretch reflexes. - Most commonly seen in the finger flexors and ankle plantar flexors. - OTs should educate clients and their families about how to bear weight actively because this usually will stop the clonus. - Can be recorded by counting the number of beats. A three beat clonus can be rated as mild and is less likely to interfere with ADLs than a clonus that is 10-beat or more. - May be elicited during quick stretch tone evaluation or may be apparent during the assessment of occupation (e.g. grasping or ambulation). - If clonus greatly interferes with ADLs, the client may be a candidate for a referral to a physiatrist or neurologist for oral medication, Botox injection, Myobloc injection or alcohol or phenol motor point block. Rigidity - An increase in muscle tone of agonist and antagonist muscles simultaneously (i.e. muscles on both sides of the joint). Both groups of muscles contract steadily, leading to increased resistance to passive movement in any direction and throughout the ROM. - Signals involvement of the extrapyramidal pathways in the circuitry of the basal ganglia, diencephalon and brainstem. - Occurs in isolated forms in disorders such as Parkinson’s disease, TBI, some degenerative diseases, encephalitis, tumors and after poisoning from certain toxins and carbon monoxide. It is also seen in conjunction with spasticity in those with stroke and TBI. Rigidity is not velocity dependent. - The four types are commonly seen: 1. Lead pipe rigidity – constant resistance is felt throughout the ROM when the part is moved slowly and passively in any direction. Feels similar to the feeling of bending solder or a lead pipe thus its name. 2. Cogwheel rigidity – a rhythmic give occurs in the resistance throughout the ROM, much like the feeling of turning a cogwheel. DTRs for both lead pipe and cogwheel are normal or mildly increased in Parkinson’s rigidity. 3. Decorticate rigidity – appears as flexion hypertonus in the UE and as extension tone in the LE. 4. Decerebrate rigidity – results from lesions in the bilateral hemisphere of the diencephalon and midbrain. Appears as rigid extension posturing of all limbs and the neck. Supine positioning increases the abnormal tone and with either type of decerebrate or decorticate rigidity, it may be extremely difficult to position the clients in sitting. MUSCLE TONE ASSESSMENT *Objective assessment of muscle tone in the client with cerebral spasticity is difficult because the tone fluctuates continuously in response to extrinsic and intrinsic factors. The postural reflex mechanism, the position of the body and head in space, the position of the head in relation to the body, and stereotypical reflexes and associated reactions all influence the degree and distribution of abnormal muscle tone. Guidelines for Muscle Tone Assessment 1. It is helpful to rate spasticity and hypertonia with the client in the same position, preferably at the same time of the day to enhance reliability, because the body and head positions influence cerebral hypertonus. 2. UE muscle tone is usually evaluated with the client sitting on a mat table when possible. 3. Trunk posture (e.g. the seated client bearing weight symmetrically versus slumped or leaning to one side) will affect the results of tone evaluation. 4. Tone fluctuates from hour to hour and day to day because of intrinsic and extrinsic factors that influence it. 5. Grasp the client’s limb proximal and distal to the joint to be tested and move the joint slowly through its range to determine the free and easy ROM available. 6. Note the presence and location of pain. 7. If there is no active movement and if the limb feels heavy, record the limb as flaccid or “0” in strength. 8. If the limb has some active movement and no evidence in increased tone, the effected muscle group may be labelled as “paretic” instead of hypotonic and may be graded in strength as it provides more objective clinical information than merely labelling the muscles as hypotonic. 9. Hold the limb on the lateral aspects to avoid giving tactile stimulation to the muscle belly of the muscle being tested. 10. Clinical assessment of spasticity involves holding the client’s limb as just described and moving it rapidly through its full range while the client is relaxed. Label tone “mild”, “moderate” or “severe” (refer to tone rating scales) 11. Clinical assessment of rigidity and hypertonia involves moving the limb slowly during the range, noting the location of the first tone or resistance to movement in degrees and labelling it as “mild”, “moderate” or “severe”. Some physicians find goniometric measuring of the location of the first tone helpful pre and post long acting nerve block, also pre and post injection. MANUAL RATING SCALES FOR SPASTICITY AND HYPERTONICITY The Ashworth Scale and Modified Ashworth Scale (MAS) – two most widely used scales to manually rate spasticity. The scales were not designed to differentiate between pure spasticity and hypertonic stretch reflexes. These scales are used to quantify the degree of the hypertonus. There is controversy in literature about the validity and reliability of the scales. Ashworth Scale Grade Description 0 no increase in ms tone 1 slight increase in ms tone, catch when limb is moved 2 more marked increase in ms tone but limb easily moved 3 considerable increase in ms tone 4 limb rigid in flexion or extension Modified Ashworth Scale (MAS) Grade Description 0 no increase in ms tone 1 slight increase in ms tone manifested by a catch and release and by minimal resistance at the end of ROM when affected part is moved in flexion or extension 1+ slight increase in ms tone, manifested by a catch followed by minimal through the remainder (less than half) of the ROM 2 more marked increase in ms tone through most of ROM, but affected parts easily moved 3 considerable increase in ms tone, passive movement difficult 4 affected parts rigid in flexion or extension Tardieu Scale and Modified Tardieu Scale (MTS) – both measure spasticity. The Tardieu Scale is in French, and was not reviewed. The MTS was shown to be more reliable than the aforementioned MAS. Mild-Moderate-Severe Spasticity Scale – some therapists and physicians find this scale easier to use than the aforementioned. Mild-Moderate-Severe Spasticity Scale Grade Description Mild The stretch reflex (palpable catch) occurs at the muscle’s end range (i.e. muscle is in a lengthened position) Moderate The stretch reflex (palpable catch) occurs in midrange Severe The stretch reflex (palpable catch) occurs when the muscle is in a shortened range. Preston’s Hypertonicity Scale – This scale is a suggested guide for estimating hypertonicity. Preston’s Hypertonicity Scale Grade Description 0 No abnormal tone detected during slow, passive movement 1 or Mild First tone or resistance is felt when the muscle is in a lengthened position during slow passive movement 2 or Moderate First tone or resistance is felt in the midrange of the muscle during slow passive movement 3 or Severe First tone or resistance is felt when the muscle is in a shortened range during slow passive movement COORDINATION The ability to produce accurate, controlled movement. Characteristics of coordinated movemement are smoothness, rhythm, appropriate speed, refinement to the minimum muscle groups needed and appropriate muscle tension, postural tone and equilibrium. Under the control of the cerebellum and influenced by the extrapyramidal system. For coordinated movements, all elements of the neuromuscular mechanism must be intact. - Depends on the contraction of correct agonist muscles with simultaneous relaxation of the correct antagonist muscles, together with the contraction of the joint fixator and synergist muscles. In addition, proprioception, body scheme, and the ability to judge space accurately and to direct body parts through space with correct timing to the desired target must be intact. Incoordination Errors in the rate, rhythm, range direction and force of mov’t Stems from either cerebellar and extrapyramidal disorders Cerebellar Disorders Ataxia Delayed initiation of movement responses, errors in range and force of movement and errors in rate and regularity of movement. Results in jerky, poorly controlled mov’ts Gait Ataxia – has a staggering wide-based gait with reduced or no arm swing. Step length may be uneven, and the client may have the tendency to fall and further results in poor postural stability. A client with a cerebellar dysfunction isolated to one cerebellar hemisphere will have the tendency to fall on the side of the lesion. Dysdiadochokinesia/Adiadochokinesis Inability to perform rapid alternating movements such as pronation and supination or elbow flexion and extension Count how many cycles a client can perform in a 10 second time frame. A cycle consists of one full repetition of supination and pronation. It is best to test the unaffected side first then compare with the affected side. Dysmetria Inability to estimate the ROM necessary to reach the target of the movement. Hypermetria VS Hypometria Asynergy/ Dyssynergia Literally known as decomposition of mov’t Voluntary mov’ts are broken up into their component parts and appear jerky Can also cause problems in articulation and phonation Rebound phenomenon of Holmes Lack of check reflex: inability to stop a motion quickly to avoid striking something Example: if the client’s arm is flexed against the resistance of the examiner and the resistance is released suddenly, the client;s hand will hit the client’s face or body. Nystagmus Involuntary mov’ts of eyeballs in an up-and-down, back and forth or rotating direction. It interferes with the head control and fine adjustments required for balance. Can result of vestibular system, brainstem or cerebellar lesions. Dysarthria Explosive or slurred speech caused by an incoordination of the speech mechanism Client’s speech may also vary in pitch, seem nasal and tremulous or both Extra-pyramidal Disorders Chorea Irregular, purposeless, involuntary, coarse, quick, jerky and dysrhythmic mov’ts of variable distribution that may occur during sleep. Tardive Dyskinesia: a drug induced disorder often associated with neuroleptic drug use and often seen in psychiatric settings. Huntington’s Disease: an inherited, autosomal dominant disease characterized by having ataxic gait with choreoathetoid mov’ts; as the disease progresses rigidity develops. Athetosis Slow, writhing, arrhythmic movements affecting the face & extremities distal musculature more affected; spooning of the hands movt’s occur in the same pattern of the same subject and are not present during sleep Mov’t patterns include alternating extension and flexion of the arm, supination and pronation of the forearm and flexion and extension of the fingers Athetosis that occurs with chorea is termed Choreoathetosis Dystonia Persistent posturing of the extremities often with concurrent torsion of the spine and associated twisting of the trunk Are often continuous and are often seen in conjunction with spasticity rhythmic twisting distortions and tone changes affecting the trunk & proximal parts of the limbs slow uncontrolled movements with fixed postures Ballismus/Ballism Rare symptom that is produced by continuous, abrupt contractions of the axial and proximal musculature of the extremity Causes the limb to fly out suddenly Occurs on one side of the body (hemiballism) coarse wide amplitude flailing or flinging movements affecting mostly the extremities damage in the subthalamic nucleus Tremors 1. Intention Tremor – associated with cerebellar disease, occurs during voluntary mov’t. It is intensified at the termination of the mov’t and is often seen in multiple sclerosis. Clients will have trouble performing tasks that require accuracy and precision of limb placement (e.g. drinking from a cup or inserting a key in a lock) 2. Resting Tremor – occurs at rest and subsides when voluntary mov’t is attempted. It occurs as a result of damage or disease of the basal ganglia and is seen in Parkinson’s disease. 3. Essential familial tremor- is an inherited autosomal dominant trait. It is most visible when the client is carrying out a fine precision task. ASSESSMENT OF COORDINATION Medical Assessment of Coordination - Observation is the most important element in clinical examination - Neurological examinations include: Nose-finger-nose test, the finger-nose test, the heel-knee test, the knee pat (pronation and supination) test, the hand pat and the foot pat tests, finger wiggling and drawing a spiral. Such tests can reveal dysmetria, dyssynergia, adiadochokinesis, tremors and ataxia. - Usually, neurologist or physiatrist performs these examinations - MRI and CT scans may also be ordered - Tremor frequency are rated with EMG which helps physician actually diagnose tremor type OT Assessment of Coordination - Selected activities and specific performance tests can reveal the effect of incoordination on function. - The therapists can prepare simulated tasks that require coordinated muscle function such as writing, opening containers, tossing and catching a bean bag or ball or playing a board game - OT must observe for irregularities in the rate of mov’t and for sudden, corrective mov’ts in an attempt to compensate for incoordination. - General guidelines are as follows: 1. Assess muscle tone and joint mobility first in sitting position 2. Observe for ataxia, proximal to distal during functional upper extremity mov’t 3. Stabilize joints proximally to distally during the functional task and note differences in client performance, as compared with performance without stabilization 4. Weighted cuffs may be applied to the extremity during task performance to determine if weighting or resistance decreases tremor (use caution). Note the amount of resistance provided. Observe whether the weights make the coordination worse. Sometimes the use of weights increases tremor. 5. Observe for tremor 6. Perform an occupational profile as well as performance pattern interviews asking about the client’s roles, routines, goals, and environment to determine which functions are important to the client. - Some standardized tests for coordination: a. The Purdue pegboard b. The Minnesota rate of Manipulation Test c. The Lincoln Oseretsky Motor Development Scale d. The Pennsylvania Bimanual Work Sample e. The Crawford Small Parts Dexterity Test f. The Jebsen Taylor Hand Function Test g. The 9-hole peg test