Acute infective diarrhoea
advertisement

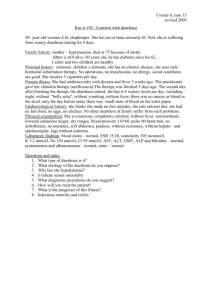
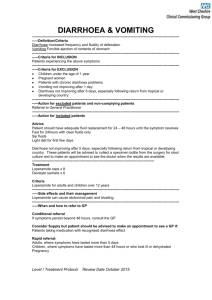
Block 8 Week 8 Acute infective diarrhoea : Gastroenteritis Tutor : Prof DF Wittenberg MD FCP(SA) dwittenb@medic.up.ac.za Objectives: To be able to list the causes and discuss the investigation and management of patients presenting with acute diarrhoea; know and discuss the epidemiology, aetiology, pathogenesis, pathophysiology, clinical features, diagnosis, complications and detailed management of patients suffering from gastroenteritis; Introduction It is estimated that on average every child will suffer from more than 2 attacks of acute diarrhoea per year before her 5th birthday. This means that an estimated 12 million episodes of diarrhoea occur in South African children each year. It is one of the commonest symptoms of disease, and also one of the most important causes of death. Illustrative Case Report : Johnny X, Case 3, p 87 You are asked to see young Johnny X because of a problem of high fever, severe vomiting and acute onset of watery diarrhoea. He is 8 months old and weighs 8.2 Kg. He attends a day care centre, where another child has had diarrhoea in the last week. One day ago he seemed to be well, but had a slight cough. After taking his bottle, he vomited all his feed, then developed a fever. Soon thereafter, his stools became loose, and then became very watery. At first, he was quite chirpy, but vomited after each bottle, even though he seemed to be thirsty and drinking quite fast. Now, he has become lethargic and pale. Mother has noticed that the soft spot on the top of his head is sunken in. His facial expression does not seem right. The stools are frequent, watery and greenish. Mother has not seen blood or slime. She is not sure whether he has any pain. Diarrhoea is a symptom of disease of the gut. Acute onset of diarrhoea as in the patient above is caused by Acute infection of the gut (acute gastroenteritis) Bacterial contamination of stored food (Food poisoning) A constituent of food of which the patient is intolerant eg laxative substance Task Review the causes and mechanisms of infective diarrhoea (C&W p 439 - 450) The most important effect of acute diarrhoea is the loss of water and electrolytes in the watery stools. Dehydration Water loss occurs initially from the circulation and all compartments of the body are affected because water moves instantaneously between compartments according to osmotic gradients. It is important to remember that the stool water in diarrhoea is not primarily derived from the oral fluids which the child may have been drinking. (Therefore it is not appropriate to withhold fluids or food in acute diarrhoea in the belief that the diarrhoea will then stop.) The loss of body water leads to compensatory mechanisms: Thirst Antidiuresis Catecholamine release of stress response Continuing water loss will result in failure of compensation, at which stage the patient enters a state of circulatory insufficiency. The clinical features of dehydration evolve in a continuous spectrum. Notes on the technique of dehydration assessment: 1. Look for signs of shock: Palpate the radial pulses. If they cannot be felt in a child, the blood pressure is most likely to be too low. Proceed to measure the blood pressure. Count the pulse rate. 2. Assess the level of consciousness and mental state, particularly the degree of alertness, apathy, irritability. Determine the muscle tone, especially in the upper limbs. Abnormalities point to decreased cerebral perfusion : consider giving oxygen 3. Assess the degree of clinical metabolic acidosis : rapid, deep breathing without evidence of lung disease. Often the mouth is pursed as if to get more air in : “Kussmaul” breathing. Count the respiration rate. 4. Determine the capillary refill time. On the heel or palm of the hand, squeeze out the skin blood to achieve a pale area of skin. Await and estimate the time to the flush of returning blood. The CFT up to 3 seconds is normal. Prolonged CFT shows that the skin capillaries are vasoconstricted : indicative of compensated shock and severe metabolic acidosis in a warm hand/foot. 5. Determine the skin turgor. Lift a fold of skin between thumb and forefinger perpendicular to the normal skinfold creases and let go, estimating how fast the skin returns to the smooth state. Choose an area of skin with adequate subcutaneous tissue, preferably where there is loose connective tissue. It is usually done on the anterior abdominal wall. Note that the skin turgor may be abnormal in patients with marasmus/wasting (“excess” skin leading to abnormal tension), in very fat babies (too little interstitial fluid between adipose cells, making assessment difficult), and in the presence of oedema. 6. Determine whether the eyes are sunken into the orbit (loss of water from the surrounding loose connective tissue). The mother is usually the best person to assess this. 7. Determine the moisture on the mucous membranes of mouth and eyes. Ask about urine output. A dehydrated baby has little tears and saliva. Each individual sign is not sensitive or specific, but taken together, one can determine the approximate severity in the following categories: Potential dehydration : Has diarrhoea, not yet clinically dehydrated. Usually no clinical signs Moderate to severe dehydration: Features of dehydration, no signs of shock. Signs 5 – 7 above are present. Severe dehydration, with features of compensated or uncompensated shock. Signs 1 – 4 are present. Management of Hydration If at the beginning of diarrhoea, mothers were to give their children as much fluid extra as they were losing in the stools, the children would not develop dehydration. Hydration management is therefore aimed firstly at maintaining hydration. This is achieved by allowing the child to drink extra clear fluid in small quantities (to avoid stomach distension and vomiting), as much as they want, after each loose stool. As the child has not yet lost much in the way of electrolytes, the specific type of fluid to be given at this stage is not critical: extra water is the issue. However, the presence of glucose and sodium improves water absorption (see C & W p 448). A dehydrated child needs electrolytes sodium, potassium and base (such as bicarbonate or citrate) in addition to glucose and water to replace losses. Now an oral rehydration solution is required. This is given at a rate exceeding the rate of loss, usually at 15 – 25 ml/kg/hour in small quantities at a time to avoid gastric overdistension and vomiting, until the patient is better, passing urine, wanting food. (C & W p 448) Once the child is so dehydrated that there is circulatory insufficiency, the patient must be resuscitated first before rehydration can take place. An isotonic solution such as Ringers Lactate is chosen and given intravenously to correct the circulating blood volume. (C & W p 449) Management of diarrhoea includes management of fluid losses as well as appropriate feeding Remember the sick gut does not tolerate foods in the normal way, or else there would be no diarrhoea. On the other hand, acute infective diarrhoea is a self-limiting condition and food changes are not indicated provided the patient is normally nourished. In general, a child with diarrhoea should receive its normal diet in small easyto-digest quantities and with some attention to short-term exclusion of high fibre, high fat/oil and meat (ie “tea and toast”, chicken soup, mashed potatoes, vegetables, paw-paw, bananas etc) and return to full usual diet within 2 – 3 days. Breastfeeding is the only type of food which can actually be increased during periods of acute diarrhoea, as breast milk has a low solute content and therefore is both food and hydration fluid! Other aspects of acute diarrhoea Task Review the other clinical complications of acute infective diarrhoea (C & W p 446 – 448) Drug therapy of acute infective diarrhoea The symptom of diarrhoea occurs after the infection has already happened and is a manifestation of its effect on the gut. Accordingly, antibiotic therapy does not shorten diarrhoea and is not indicated in the usual case. In any case, the majority of cases of diarrhoea are due to infection with viruses. Antidiarrhoeal medication is not indicated in young babies under 2 years of age, as these have most side effects and the antimotility effect of the drugs delays the rate at which toxins and bacteria are “flushed through”. Anti-emetic drugs have a central mode of action, where the vomiting is due to local factors in the stomach. Dehydrated children have a higher blood level of any drug than anticipated and tend to have more side effects. Case Analysis Johnny has an acute infection of the gut for the following reasons: Previously healthy and well nourished (weight 8.2 Kg at 8 months) Contact history with other children who had a similar disease in the recent past Acute fever with his disease On the basis of frequency and probability, he may have a rotavirus infection. The presence of cough is in support of this diagnosis. His symptoms suggest the presence of dehydration: Thirsty, drinking fast Lethargy Sunken fontanel He has acute gastroenteritis (possibly rotavirus infection) with dehydration He must be offered oral rehydration fluid, 120 – 150 ml per hour given by teaspoon in 10 – 15 ml quantities every 5 minutes. If he tolerates that and wants more, he can be given more. Once he passes urine, he can be offered about half his usual bottle of milk and a little porridge. Continue offering extra fluids after stools and for thirst. Review his clinical state in 4 – 6 hours for the presence of dehydration or other complication. Advise the mother on reasons to return or complications Chronic diarrhoea and malabsorption Objectives: To be able to list the causes and discuss the principles of investigation and management of patients suffering from chronic diarrhoea; know and discuss an approach to the diagnosis and management of patients presenting with chronic diarrhoea, failure to thrive and food intolerance; know and discuss the clinical features and principles of diagnosis and management of allergic enteropathy, coeliac disease, chronic enteropathy, malabsorption and cystic fibrosis. Illustrative Case report 4, page 88 You are asked to assess Baby Melissa N aged 5 months, with a problem of diarrhoea lasting longer than 2 weeks. Baby N had been a normal baby at birth with a weight of 3.2 Kg. She had been breastfed and had thrived beautifully. At 3 months her weight was 6.1 Kg. There had been no symptoms of disease. At 3 months Mrs N had to return to work and weaned Melissa onto a commercial formula feed recommended by her neighbour. She also placed Melissa into the Day Care Centre at the company where she works Some 4 or 5 weeks later, Mrs N was told that several infants at the Day care Centre had taken ill with diarrhoea and vomiting. The following day, Melissa also became ill. She started to vomit after feeds, developed a mild pyrexia and then proceeded to have very profuse watery stools. Unable to keep anything down, she became listless and weak. The anterior fontanel was visibly sunken in, her mouth was dry and the doctor admitted her to the Private Hospital for an intravenous drip. By the next day, she seemed to be much better and was discharged with advice regarding oral rehydration. Melissa’s diarrhoea did not settle. Mrs N gave her the recommended oral rehydration fluid, which she took, but the stools remained watery, turning green. She developed a red shiny nappy rash. Her appetite for the milk formula and her baby cereal remained very poor and she vomited occasionally. The fever seemed to return intermittently. On examination, she is an unhappy little girl with a nappy rash. Her weight is now only 5.7 Kg. The hydration state is reasonable, but mother is giving her approximately 3 bottles fluid extra per day. Her abdomen seems to be somewhat distended. There is no obvious tenderness, resistance or guarding, and there is no organomegaly. The stool in the nappy is very liquid, yellow-green, granular in appearance, with some strands of mucus being present also. Introduction If diarrhoea lasts longer than 2 weeks, it cannot be called gastroenteritis. Now the main issue is the function of the gut in digestion and absorption of food and in its motility rather than a disorder due to an acute infection. The problem of chronic diarrhoea is therefore different to that of acute diarrhoea in diagnosis and management. A detailed history of the patient’s disease is mandatory. This will frequently point the way to the diagnosis. Was the onset of the disease acute as in acute gastroenteritis in a previously quite normal child with normal stools? If that is the case, the following options must be explored: 1. Acute infection persisting. This may apply to situations with immune deficiency (eg severe malnutrition or HIV) where the patient cannot clear infections in a normal way. 2. New infection superimposed. This is often the case where patients with acute gastroenteritis have been admitted to hospital for rehydration and then develop nosocomial infection in the ward 3. Post-infectious damage to the intestinal mucosa eg lactose intolerance 4. Intraluminal bacterial overgrowth and deconjugation of bile salts with secondary bile acid secretory diarrhoea Was the onset of the disease an insidious beginning after a period of normal stools and normal thriving? This may point to 1. Allergic enteropathy. The gut must be exposed to the foreign antigen before sensitisation occurs. Typically symptoms develop gradually after a period of about 4 weeks exposure to the protein to which the patient has become allergic 2. Coeliac disease. The patient must be exposed to wheat protein first, before the auto-immune gluten enteropathy can occur. 3. Fat malabsorption from pancreatic insufficiency (cystic fibrosis), chronic liver disease 4. Inflammatory bowel disease Is there evidence of excess water loss in the stools? Such patients commonly have a severe form of small intestinal mucosal injury. Is there failure to thrive or loss of weight? A patient who is thriving despite a history of chronic diarrhoea usually has a motility problem such as toddler diarrhoea rather than malabsorption. If the patient is not thriving, the condition is associated with significant malabsorption or loss of nutrients. Is the patient’s appetite normal, increased or decreased? Patients with pancreatic malabsorption often have an increased appetite, while patients with small intestinal disease usually are anorectic. Chronic diarrhoea With failure to thrive and excessive stool water losses : small intestinal mucosal injury; With failure to thrive but without excessive water loss : malabsorption syndromes’ without failure to thrive : motility disorders Task Review the causes, mechanisms and management of chronic diarrhoea ( C & W p 440 – 442, 451 - 454) Analysis of the above case: This girl’s diarrhoea started as an acute episode of probably infective gastroenteritis. She had been in contact with other children with a similar disease, she had a fever, and she had acute dehydrating gastroenteritis for which she was admitted to hospital. When the diarrhoea did not settle, her disease could not be described as gastroenteritis any more. She still needed extra oral fluids to prevent dehydration. She was losing weight. She had a nappy rash. No additional features of illness were observed. This case needed investigation to identify the reason for persistence of dehydrating diarrhoea after acute gastroenteritis with failure to thrive. Stool analysis showed a low pH and reducing sugars. This is typical of acquired lactose intolerance after severe gastroenteritis. Removal of lactose from her diet quickly stopped the diarrhoea and allowed her to start regaining her weight again. This is an example of damage acquired due to the initial infection. This outcome is more likely in the following circumstances: Young age under 6 months Malnutrition : such patients have a degree of mucosal atrophy which is aggravated by infection Inappropriate feeding during acute gut infection, especially if high volume feeding is continued during severe dehydration During acute gastroenteritis, watery stools should be tested with a Clinitest ® for the presence of reducing sugars. If this is strongly positive and the diarrhoea is persisting at high purging rates, a change of diet to lactose-free is indicated. An urine dipstix can also be used to test stool water and may show the presence of unabsorbed glucose. Glucose is the product of carbohydrate digestion in the lumen of the gut and is absorbed from the small gut by active transport mechanisms (sodium and amino-acid-linked glucose cotransporters). If much glucose is found in the stools, it indicates significant mucosal damage to active transport systems. In such situations, abnormal tests of absorption may also be found. D-Xylose is an inert sugar which is absorbed like glucose, but then excreted via the urine. An abnormally low D-Xylose absorption test is found in cases of damage to the gut mucosa with mucosal atrophy, such as in coeliac disease. Such patients will usually have a number of deficiencies secondary to the gut damage interfering with nutrient absorption. Illustrative Case report 6, page 90 : SN is a girl aged 11 years 5 months. She is referred to the hospital because she has begun swelling up over the last week or so, particularly in her legs and face. Her abdomen is also very distended, and she has vomited a few times. Her mother states that she was admitted to hospital in early 1995 with similar complaints, but was discharged without treatment or advice. On further questioning, mother explains that S was a normal baby at birth. From early on, she has had episodes of diarrhoea alternating with constipation. She has always had very smelly stools. She has also never grown well and is the smallest child in her class by far. She has a poor appetite, eating only small amounts at a time. She cannot eat tomatoes, but gets bread for breakfast and school lunch. She is not a happy child, often moody or aggressive. On examination, she weighs 24 kg and is 125.6cm tall. She looks chronically ill. She has a puffy face and some peripheral oedema. She has gross abdominal distension, which also shows shifting dullness to percussion and a succussion splash but no fluid thrill. Her liver is enlarged 3 cm, firm, smooth and non-tender. On rectal examination, her rectum is loaded with offensively smelling faeces. The other systems seem to be normal. Investigations show her to have : Hypoproteinaemia, hypo-albuminaemia, low levels of serum potassium, phosphate, magnesium, zinc, copper, vitamin A, red cell folate; a much increased loss of faecal fat, very low absorption of D-xylose, and increased appearance of lactose and sucrose in the urine. Her stool contains some glucose. A duodenal biopsy shows severe mucosal atrophy. A diet is prescribed and within one month she has lost her oedema, is asymptomatic and the blood tests have normalised. She is advised to continue on this diet for the rest of her life and to be followed up regularly. Because chronic diarrhoea is sometimes so much part of his/her daily life, the patient may not emphasise this symptom and may complain of a more acute development instead. It is very important to enquire very carefully into all intestinal symptoms and particularly their relationship to any food constituents and any changes. Remember also that many symptoms may be wrongly attributed to particular foods, and that responses after food changes are equally subjective. The timing, frequency and intensity of exposure to any food must be documented. Task Review the meaning and definitions of the following terms: Intolerance : the development of symptoms on exposure to a food. In itself, this does not define the pathology Allergic : Sensitisation to foreign protein, symptoms on re-exposure : immune-mediated Biochemical : Deficiency of an enzyme, symptoms because of maldigestion or –absorption Chemical : due to a chemical constituent exerting an effect eg laxative, salicylate It is thus possible for a person to have milk intolerance symptoms because of milk protein allergy, lactose maldigestion, malabsorption as a result of cystic fibrosis or because of a chemical substance in milk derived from the food the cow was eating…. Malabsorption : Failure to absorb one or more nutrients from the gut. May be associated with diarrhoea. Results in nutrient deficiencies. Maldigestion : Inability to digest a specific nutrient eg lactose, in the lumen of the gut. Does not always have to be associated with diarrhoea or failure to thrive. Symptoms because of unabsorbed food constituent in the gut lumen. In a patient with suspected malabsorption, tests are done to confirm the fact of malabsorption. This includes the D-Xylose test, estimation of faecal fats, blood levels of vitamin A and B12, red cell folate and serum albumen. One can next do tests to identify the gut pathology. This would include imaging studies and a gut biopsy. Thereafter, tests must be done to identify the aetiology of malabsorption. This includes microbiological studies, sweat test and DNA analysis for cystic fibrosis, allergy tests and antibody tests for coeliac disease (anti-endomysial antibody, anti-gliadin antibody, tissue transglutaminase). Analysis of the above case The girl presented at age 11 years with severe malnutrition and hypoproteinaemia, growth failure and specific deficiencies. From analysis of the child’s height age (the age at which her present height corresponds to the 50th percentile) it can be seen that she has had a chronic problem which has interfered with her growth. The intestinal symptoms of intermittent diarrhoea with foul-smelling stools point to malabsorption. Malodorous stools occur with fermentation of unabsorbed fats especially. She was shown to have severe malabsorption of D-Xylose and fats. There were a large number of nutrient deficiencies pointing to malabsorption of these also. She was next shown to have duodenal mucosal atrophy. She has a condition which damages her small intestinal mucosa. The most important condition to consider in this context is coeliac disease, although her intolerance of tomatoes may suggest an allergic basis of her condition. However, voluntary tomato exclusion from her diet has not made a difference and she has persistent exposure to wheat products. Accordingly, she was tested for coeliac disease and this was confirmed. On a strict gluten-free diet, she improved remarkably and proceeded to grow at an accelerated pace