Risk Factors
advertisement

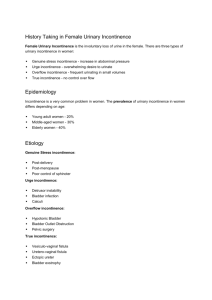
Incontinence Notes: Literature review Definition “Urinary incontinence is defined as leakage of urine which is socially or hygienically unacceptable. In women it is widespread and often debilitating condition, which generally remains well concealed in society. It may have far reaching consequences for women’s social, psychological and medical well being. Women with incontinence may become isolated from friends and family and even partners due to fear of embarrassment. Midwives have a key role to play in the prevention and identification of this condition. Smalldridge J [2000] Incontinence after childbirth. MIDIRS Midwifery Digest. 10[1] Pp79-81 Urinary incontinence is common during pregnancy and is often transient, it is attributed to the enlarged uterus, fluctuating hormone levels, increased glomerular filtration rates and tempory changes in the urethrovesical angle. Unlike antenatal incontinence postpartum incontinence is typically attributed to pathophysiological changes as a consequence of delivery. Burgio K, Zyczynski H, Locher J et al [2003] Urinary Incontinence in the 12 month postpartum period. Obstetrics and Gynaecology. 102[6] Pp 1291-1298 Prevalence. In 2003 a telephone survey conducted in Australia, Canada, France, Germany, Italy, Mexico, Spain, Sweden and UK. The rates of reported stress urinary incontinence was second highest in the UK, only Canada was higher. Women with stress incontinence reported having to change their lifestyles in many ways. In the UK 64 % of women had not received any treatment, only 38% of women with incontinence symptoms had consulted a doctor. More than 60% of the women did not feel it was an important enough to bother a doctor. Haslam J [2004] The prevalence of stress incontinence in women. Nursing Times. 100[20] Pp 71-73 One in every three women will have incontinence during her lifetime and up to 65% of those women will recall that it began either during pregnancy or after childbirth. The first vaginal delivery was the risk factor, subsequent deliveries were not found to further increase the risk. Goldberg R, Kwon C, Gandhi S et al [2003] Urinary incontinence among mothers of multiples. American Journal of Obstetrics and Gynaecology. 188[6] Pp 1447-1453 ¼ of primiparous women and 1/3 of multiparous women with a history of vaginal delivery have an anal sphincter defect. Hence the incidence of anal sphincter damage is much higher than commonly estimated. At least 2/3 of these defects are asymptomatic. Oberwalder M, Conner J and Wexner S [2003] Meta-analysis to determine the incidence of obstetric anal sphincter damage. British Journal Of Surgery 90[11] Pp 13333-1337 When stress incontinence occurs during the first pregnancy the risk of stress incontinence 15 years later is doubled. Even when symptoms resolve postnataly re- occurance is likely. Subsequent pregnancy did not increase this risk. Postnatal exercises were not seen to reduce the incidence of symptoms at 7 and 15 years. This could be due to the motivation and supervision of exercise in the long term. Dolan L, Hosker G, Mallett V et al [2003] Stress incontinence and pelvic floor Neurphysiology 15 years after the first delivery. BJOG: An International Journal of Obstetrics and Gyaenecology. 110[12] Pp 1107- 1114 Risk Factors Vaginal births increased the risk of stress and mixed incontinence, but not urge incontinence or over active bladder. The risk of all types of incontinence was increased in women with high BMI, history of hysterectomy, urinary infection and perineal trauma. Heavy smokers have been shown to have a higher incidence of incontinence though the reasons for this seem unclear. Parazzini F, Chiaffarino F, Lavezzari M et al [2003] Risk factors for stress, urge or mixed urinary incontinence in Italy. BJOG: An International Journal of Obstetrics and Gynaecology. 110[10] Pp 927-933 Perineal trauma during childbirth is a causative factor of urinary incontinence; contributing factors include forceps, episiotomy, large baby or long second stage. Maintaining an intact perineum is not necessarily protective because there can still be hidden nerve damage. Layton S [2004] The Effect of perineal Trauma on Women’s Health. British Journal Of Midwifery 12[4] Pp 231-236 Other factors significant in urinary incontinence include smoking which is thought to be linked to increased pressure from coughing, Obesity and when antenatal incontinence occurs there is greater risk of it continueing into the postpartum period. Burgio K, Zyczynski H, Locher J et al [2003] Urinary Incontinence in the 12 month postpartum period. Obstetrics and Gynaecology. 102[6] Pp 1291-1298 Forceps delivery has been shown to increase the risks of urinary incontinence compared to vaginal delivery or CS. Arya L, Jackson N, Myers D [2001] Risk of new onset urinary incontinence after forceps. American Journal of Obstetrics and Gynaecology. 185[6] Pp 1318-1324 Treatments Pelvic floor exercises are more commonly associated with improvement of symptoms than a total cure. It takes several months of pelvic floor muscle training to effect the physiological muscle change to reduce or stop urinary leakage on exertion. They can also help to avoid or delay the need for surgery and can increase sexual satisfaction. The ability ti identify and contract the correct muscle is essential for pelvic floor exercise success. Breif verbal or written instruction is unlikely to be effective in assisting women in this. Haslam J [2000] Pelvic Floor muscle exercises. Nursing Times plus. 96[42] Pp 24. Non compliance of pelvic floor exercises are due to inconvienience, lack of time, motivation problems and travel time to clinics. Pelvic floor exercises may not be appropriate if significant prolapse and or denervation, or if intrinsic sphincter damage. Wilson P and Herbison G. [1998] A randomised controlled trial of pelvic floor exercises to treat postnatal urinary incontinence. International Urogynecology Journal. 9 Pp 257- 264. Non-surgical treatments for incontinence include: Pelvic floor exercises, electrical stimulation, and vaginal cones. Surgical treatments include: laproscopic, open retro pubic and needle colposuspension. Suburethral slings and anterior vaginal repair. Postnatal pelvic floor exercises appear to be effective in decreasing postnatal urinary incontinence, insufficient evidence exists to support there effectiveness in reducing anal incontinence and prolapse. Harvey MA [2003] Pelvic Floor exercises during and after pregnancy: a systematic review of their role in preventing pelvic floor dysfunction. Journal of Obstetric and Gynaecology Canada 25[6] Pp 487-498 Intensive pelvic floor muscle training during and after pregnancy prevents urinary incontinence and significantly improved pelvic floor strength. Significantly fewer women who practiced antenatal pelvic floor exercises reported symptoms of urinary incontinence. No negative side effects were noted with the exercise regime. Morkved S, Bo K, Schei B et al [2003] Pelvic floor muscle training during pregnancy to prevent urinary incontinence: a single blind randomised controlled trial. Obstetrics and Gynaecology 101[2] Pp 313-319 Supervised antenatal pelvic floor exercises are effective in reducing the risk of postpartum stress incontinence in primigravidae. Clients who performed pelvic floor exercises for 28 days or more were found to suffer less symptoms of stress incontinence. Supervised pelvic floor exercises were more effective than verbal instruction. It is noted that it is antenatal rather than postnatal exercises that were found to be most effective. Reilly E, Freeman R, Waterfield M [2002] Prevention of postpartum stress incontinence in primigravidae with increased bladder neck mobility: a randomised controlled trial of pelvic floor exercises. BJOG: An international Journal of Obstetrics and Gynaecology. 109[1] Pp 68-76 Pelvic floor education begun 2 months postpartum, significantly reduced the incidence of stress incontinence but not anal incontinence. Meyer S, Hohfeild P, Achtari C et al [2001] Pelvic Floor education after vaginal delivery. Obstetrics and Gynaecology. 97[5] Pp 637-677 Women who attended an antenatal programme of pelvic floor exercises and who practised them daily had less risk of urinary stress incontinence. Jones M [2000] Pelvic Floor exercises: a comparative study. British Journal Of Midwifery. 8[8] Pp 492-498 Bladder training enables women to accommodate increasingly greater volumes of urine in the bladder and gradually to extend the interval between voiding. Pelvic floor muscle training increases awareness of function and strengthens these voluntary muscles, promoting continence. Sampselle C [2000] Behavioral intervention for urinary incontinence in women: evidence for practice. Journal of Midwifery and women’s Health. 45[2] Pp 94103 RCT’s have found that Electrical stimulation reduces symptoms of stress incontinence compared to no treatment at all. However no significant differences were noted between the effect of electrical stimulation and the effect of pelvic floor exercises or vaginal cones. Pelvic floor electrical stimulation has been associated with a small number of cases of vaginal irritation. Pelvic floor exercises were more beneficial in rates of cure or improvements compared to no treatment but were not any more or less effective than other forms of treatment. While no difference in effects were seen between vaginal cones and pelvic floor exercises at twelve months vaginal cones were less effective at reducing leakage at six months compared to pelvic floor exercises. Vaginal cones were also associated with difficulty maintaining motivation for use and a small number reported vaginitis and abdominal pain. Vaginal cones were also more difficult to use and some women reported an unpleasant feeling, discomfort, and bleeding and vaginal prolapse.. There is little available evidence comparing surgical treatments to no treatment or non surgical treatment, however one review found that laproscopic colposuspension was less effective than open retro-pubic colposuspension in improving objective cure rates at 1 year. Open retro pubic colposuspension increased cure rates at 1-5 years compared with non surgical treatment, anterior vaginal repair or needle colposuspension. But it was also associated with more adverse effects. No significant difference was found in objective cure rates at five years. Suburethral slings were associated with increased perioperative complications including an increased risk of bladder perforation. Bazian Ltd [2004] Stress Incontinence. Clinical Evidence. 11 Pp 2543-2557. Pelvic floor exercises are shown to be effective in maintaining continence, however they need to be explained carefully and practiced daily to be effective. Midwives have an important role in informing women of the importance of practicing PFE. Layton S [2004] The Effect of perineal Trauma on Women’s Health. British Journal Of Midwifery 12[4] Pp 231-236 Managing the problem of urinary incontinence is extremely expensive conservative estimates are in excess of £424 million annually in the UK. Continence Foundation [2000] Incontinence cost NHS £424 million a year. Continence Newsletter 6. Pp 1-2. Conservative therepy including pelvic floor exercises combined with bladder training and biofeedback has been demonstrated to be effective. Surgery is indicated in very few selected patients Lacima G and Pera M [2003] Combined fecal and urinary incontinence: an update. Current opinion in Obstetrics and Gynaecology 15[5] Pp 405-410 Information/ midwives role Many women suffering from stress incontinence do not seek medical advice for various reasons including acceptance that incontinence is just a part of life and the feeling that nothing can be done anyway. The midwife has a unique position that allows her to act as detective, in identifying women with genuine stress incontinence. It may be beneficial to adopt a a score system focused on the risk factors. As midwives are not specifically trained in this area the sytem would need to be easy and standardized. Pelvic floor exercises are a cheap and simple initial treatment Midwives need to initiate this with verbal advice followed by follow up in the clinical setting as verbal instructions alone are insufficient. It is important that the pelvic floor instructor possesses the appropriate skill. Peeker I and Peeker R [2003] Early diagnosis and treatment of genuine stress incontinence. Journal of Midwifery and Womens health.48[1] Pp 60-66 The majority of women asked were not given information about incontinence but said that they wanted professional to warn them that the condition may appear, They also wanted professional to actively ask for information regarding symptoms and not wait for the woman to broach the subject. As the main form of treatment is pelvic floor exercises midwives should actively seek out those experiencing problems and recommend early commencement of a exercise programme. Health professionals need to raise awareness of the condition, the treatment available and be pro active in seeking out hose experiencing incontinence rather than wiat for women to come forward. Reluctance to seek advice also comes from ebarrassment and a feeling that they should not bother health professionals. 69% of women studied had not received any advice or information on Stress incontinence. Women requested information on this condition during pregnancy as they said that it was quite a shock when it occurred. Knowledge of the condition could lesson the taboo and the embaressment enabling women to more readily seek help. Incontinecne is often viewed as a social problem rather than a medical one. The lack of control over a bodily function taught as a child is socially unacceptable. Another reason for not seeking help was that women didn’t feel they new which Health professional to approach and felt that they had lost touch with the midwives too early. For many women ten days is too early to identify persistent problem such as incontinence. Mason L, Glenn S, Walton I et al [2001] Women’s reluctance to seek help for stress incontinence during pregnancy and following childbirth. Midwifery. 17[3] Pp 212-221 Childbirth is a major influence on stress incontinence. Pelvic floor exercises have been shown to be effective in preventing or reducing symptoms of stress incontinence. Midwives need to be taking opportunity to promote the correct practice of pelvic floor exercises to women at antenatal classes and in the wider community. Parker C [2001] Do midwives really promote pelvic floor exercises? Professional care of mother and child. 11[3] Pp 73-75 Pp 73-75 In order to reduce the risk of incontinence after childbirth improvements in several areas of care are needed. Improved information giving, improved professional communication and improved recognition and management of third degree tears. Clarkson J, Newton C, Bick D et al [2001] Achieving sustainable quality in maternity services – using audit of incontinence and dyspareunia to identify shortfalls in meeting standards. BMC Pregnancy and Childbirth. 1[4] Pp 5-10 Mediolateral episiotomy does not protect against urinary and anal incontinence and is associated with lower pelvic floor strength compared to spontaneous perineal lacerations and with more dyspareunia and perineal pain. Sartore A, De Seta F, Maso G,et al [2004] The effects of Mediolateral Episiotomy on Pelvic Floor Function After Vaginal Delivery. Obstetrics and Gynaecology. 103[4] Pp 669-673 The midwives decision regarding whether to suture 1st and 2nd degree tears was not found to affect the incidence of urinary incontinence. As perineal damage is significant when looking at anal incontinence this decision should only be reached after careful assessment of damage. Layton S [2004] The Effect of perineal Trauma on Women’s Health. British Journal Of Midwifery 12[4] Pp 231-236 Health care professionals who come into regular contact with women during and after pregnancy do not appear well-informed about the subject. Women are not receiving the information they deserve to allow them to take control of the problem. Many women are dissatisfied with the information on incontinence. Women believe the problem to be part of being female and that nothing can be done. Midwives suggest barriers to the introduction of the topic of PFE’s including lack of knowledge, insufficient time, early discharge of mothers, poor quality information leaflets, and women not attending parentcraft. There is no agreed national standard to which instructors of PFE’s should work. Logan K [2001] Audit of advice provided on pelvic floor exercises. Professional Nurse. 16[9] Pp 1369-1372 Cure or improvement rates were usually higher in women who had more frequent contact with Health professionals this was thought to be due to an increased compliance rate with pelvic floor exercises. BO K [1999] Single blind randomised controlled trial of pelvic floor exercises, electrical stimulation, vaginal cones and no treatment in management of genuine stress incontinence in women. British Medical Journal. 318 Pp487- 493 Motivation is critical prerequisite for influencing the ultimate success of pelvic floor exercises. Health professional must develop an understanding of factors that influence motivation if they are to optimise clients chances of successfully incorporating pelvic floor exercises into their lives. Gallo L and Saskin D [1996] Cues to action: pelvic floor muscle exercise complience in women with stress urinary incontinence. Neurology and Urodynamics 16 Pp167-177. Nurses can play a crucial role in influencing compliance and are ideally placed to work in partnership with women to explore imaginative approaches that will assist women in maximising and maintaining compliance with pelvic floor exercises. Paddison K [2002] Complying with the pelvic floor exercises: a literature review. Nursing Standard. 16[39] Pp 33-38 While it is recognised that pelvic floor exercises are beneficial in eliviating symptoms they are usually not taught in a manner intensive enough to achieve significant results. Health professionals need to be more robust in detecting at risk groups and implementing an intensive programme of pelvic floor exercises. Burgio K, Zyczynski H, Locher J et al [2003] Urinary Incontinence in the 12 month postpartum period. Obstetrics and Gynaecology. 102[6] Pp 1291-1298 There should be a muti-disciplinary approach which is of interest to at least three professional disciplines. Cases who had received supervised pelvic floor exercise programmes showed fewer symptoms of stress incontinence. No single profession appeared to take responsibility for this and as a result the information in some cases was replicated and in other completely absent. Mason L [2001] Guidelines on the teaching of pelvic floor exercises. British Journal of Midwifery 9[10] Pp 608-611 Anal Incontinence Flatus and fecal incontinence is increased with age, birth weight greater than 4kg and history of anal sphincter tears. Age was more of a risk factor then type of delivery alone. Hojberg K, Salvig J, Winslow N Et al [2000] Flatus and Faecal incontinence: prevalence and risk factors at 16 weeks of gestation. BJOG: An International Journal of Obstetrics and Gynaecology. 107[9] Pp 1097-1103 Mothers of multiples reported substantial rates of fecal and flatus incontinence. Rates were further increased with age. CS alone was not significantly protective alone. Though the study did not look at separating elective Cs with Cs following labour. Goldberg R, Kwon C, Gandhi S [2003] Prevalence of anal incontinence among mothers of multiples. American Journal of Obstetrics and Gynaecology. 189[6] Pp 1627-1631 Caesarean section No difference in stress incontinence between women who had vaginal delivery versus CS following labour and CS with no labour therefore CS was not found to be protective. Reilly E, Freeman R, Waterfield M [2002] Prevention of postpartum stress incontinence in primigravidae with increased bladder neck mobility: a randomised controlled trial of pelvic floor exercises. BJOG: An international Journal of Obstetrics and Gynaecology. 109[1] Pp 68-76 Vaginal delivery may cause maternal bowel and urinary symptoms which may perist 5 years after delivery. Carter J, Johanson R, Heycock E et al [2001] Long-term health after childbirth. British Journal of Midwifery. 9[12] Pp 748-753 Caesarean section was associated with a decreased risk of urinary incontinence; there was no association with reduced risk of fecal incontinence. Chaliha c, Digesa A, Hutchings A et al [2004] Caesarean section is protective against stress incontinence: analysis of women with multiple deliveries. BJOG: An international journal of obstetrics and Gynaecology. 111[7] Pp 754-755 Severe incontinence can occur even after elective caesarean section and current evidence does not support the use of elective CS for prevention of urinary incontinence. Mode of delivery should be depicted by obstetrics consideration. Lal, M [2003] Prevention of urinary and anal incontinence: role of elective caesarean delivery. Current Opinion in Obstetrics and Gynaecology. 15[5] Pp 439-448. Women who have experience previous anal sphincter rupture are at increases risk of anal incontinence. CS is protective and women should be seriously counselled on this when making a choice for type of delivery. McKenna D, Ester J, Fischer J [2003] Elective caesarean delivery for women with a previous anal sphincter rupture. American Journal of Obstetric and Gynaecology. 189[5] Pp 1251-1256 Planned Cs for breech presentation at term can be protective against incontinence with no other problems found at three months postpartum. Though longer-term effects were not analysed. Hannah M, Hannah W, Hodnett E et al [2002] Outcomes at three months after planned Caesarean vs. planned vaginal delivery for breech presentation at term: the international randomised term breech trial. Journal of the American Medical Association. 287[14] Pp 1822- 1831 Only stress incontinence was associated with the mode of delivery. The risk was higher in women who had CS compared to women who had not had a baby but was even higher in women who had a vaginal delivery. 8.4% higher prevalence of incontinence among women who had had vaginal deliveries than among those who had had cs deliveries. Though as incontinence still occurs in the CS group it is suggested that part of the risk factors for incontinence may be pregnancy itself and the effects of hormones. Recommending Cs as protective may be unrealistic as it only reduces the risks for women who deliver all their babies by CS and the reduced risk only occurs at a younger age, no difference is found in the over 50 age group. Rortveit G, Daltveit A, Hannestad Y et al [2003] Urinary incontinence after vaginal delivery or caesarean section. New England Journal of Medicine. 348[10] Pp 900- 907 Multiple pregnancy puts greater strain on the pelvic floor and CS can offer a significant reduction in the risk of stress incontinence. This protective effect is less profound in women with singleton pregnancy so the findings should not be generlisable. Goldberg R, Kwon C, Gandhi S et al [2003] Urinary incontinence among mothers of multiples. American Journal of Obstetrics and Gynaecology. 188[6] Pp 1447-1453 Incontinence symptoms are also seen in women who have had a Cs therefore CS is not wholly protective against urinary stress incontinence. Chaliha C, Khullar V, Stanton S et al [2002] Urinary symptoms in pregnancy: are they useful for diagnosis? British Journal of Obstetrics and Gynaecology. 109[10] Pp 1181-1183 Episiotomy/ Perineal trauma Mediolateral episiotomy is associated with weaker pelvic floor strength and increased dyspareunia and perineal pain. It was not found to be protective against either urinary or fecal incontinence. Sartore A, De Seta F Maso G Et al [2004] The effects of Mediolateral episiotomy on pelvic floor function after vaginal delivery. Obstetrics and Gynaecology. 103[4] Pp 669- 673 Anal Sphincter damage at delivery has been linked with an increased risk of anal incontinence. Zetterstrom J, Lopez A, Holmstrom B et al [2003] Obstetric sphincter tears and anal incontinence: an observational follow-up study. Acta Obstetricia et Gynecologica Scandinavica. 82[10] Pp 921-928 Training in perineal anatomy and repair is poorly taught and there is wide variation in classification of perineal trauma, consequently many anal sphincter tears are missed or inappropriately managed. Anal sphincter damage is significantly linked to anal incontinence and this risk is further increased when trauma is unrecognised or miss managed. Sultan A, Thaker R [2002] Lower genital tract and anal sphincter trauma. Best practice and research clinical obstetrics and gynaecology. 16[1] Pp 99-115 Risk factors When compared to women who had not had a vaginal delivery, CS increased the risk of incontinence, as did instrumental and vaginal delivery. Offer risk factors also include History of urine infections, Hysterectomy, High BMI and history of perineal trauma. Parazzini F, Chiaffarino F, Lavezzari M, Et al [2003] Risk factors for stress, urge or mixed incontinence in Italy. BJOG: An International Journal of Obstetrics and Gynaecology. 110[10] Pp 927-933 Mothers with multiple pregnancy were found to be at increased risk of fecal incontinence, this increased risk was also associated with maternal age, CS was not found to be significantly protective. Goldberg R, Kwon C, Gandhi S et al [2003] Prevalence of anal incontinence among mothers of multiples and analysis of risk factors. American Journal of Obstetrics and Gynaecology. 189[6] Pp 1627-1631 The causes of postpartum urinary incontinence may not only be associated with pelvic floor trauma but also a deficiency in urethral resistance caused by drugs, such as prostaglandins. Pregazzi R, Sartore A, Troiano L et al [2002] Postpartum urinary symptoms: prevalence and risk factors. European Journal of Obstetrics and Gynaecology and Reproductive Biology. 103[2] Pp 179-182 In first time mothers incontinence persisted longer following a forceps delivery than a normal or ventous extraction. Arya L, Jackson N, Myers D Et al [2001] Risk of new-onset urinary incontinence after forceps and vacuum delivery in primiparous women. American Journal of Obstetrics and Gynecology. 185[6] Pp 1318-1324