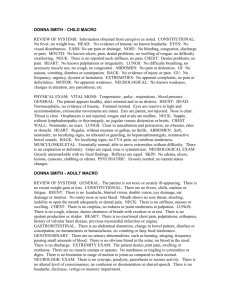
Joseph Gulde Sample
advertisement

Joseph Gulde Sample Date of Visit: 07/27/2003 CHIEF COMPLAINT: Broken tooth. HISTORY OF PRESENT ILLNESS: This is a 32-year-old Caucasian female who states she has pain in the right upper premolar. She states that she missed a step, or the curb edge, and as she came down, struck the outer part of her mouth, I believe, on a light post. She states that she broke off the right upper tooth. This is just prior to presentation. She states she stop and get some Oragel, which is not controlling the pain and she presents on an ambulatory basis. PAST MEDICAL HISTORY: None other than very poor dental hygiene. PAST SURGICAL HISTORY: She has had a tubal ligation. SOCIAL HISTORY: She smokes half-pack of cigarettes daily; denies alcohol or reactional drug use. ALLERGIES: ASPIRIN. MEDICATIONS: None currently. REVIEW OF SYSTEMS: GENERAL APPEARANCE: Not toxic or acutely ill-appearing. Absence of recent weight loss/gain. Her last menstrual period was approximately a week ago. CONSTITUTIONAL: No fever, chills, malaise, fatigue. HEENT: No headache, no blurred vision, double vision, eye drainage, earache, ear drainage or tinnitus. NOSE: No runny nose or nose bleed. MOUTH: No sore throat, drooling, inability to open the mouth adequately, or dental pain. NECK: No neck stiffness, masses or swelling. CHEST: No area of crepitus, redness or point tenderness to palpation. LUNGS: No cough, wheezing, feelings of shortness of breath on exertion or at rest. No sputum production, no stridor. HEART: No exertional chest pain, palpitations, orthopnea, no history of valvular heart disease, previous MI or angina. GI/GU: No abdominal distension, change in bowel patterns such as diarrhea or constipation. No hematemesis or hematochezia, or vomiting, no fatty food intolerance. No urinary abnormalities such as burning, stinging, frequency or passage of small amounts. No obvious blood in the urine. No blood in the stool. No urethral discharge/vaginal bleeding or discharge. No penile discharge. EXTREMITY EXAM: No localized swelling, tenderness. No calf pain at rest or with walking. No dependent edema. NEUROLOGICAL EXAM: No syncope, no paralysis, no paresthesias, no seizure activity. No alteration of level of consciousness, confusion, disorientation, slurred speech. PHYSICAL EXAMINATION: GENERAL: This is a 32-year-old Caucasian female, awake, alert and oriented. VITAL SIGNS: Temperature 97, pulse rate 94, respiratory rate 18, blood pressure 144/104. HEENT: Atraumatic, normocephalic. Pupils equal, round and reactive to light. Extraocular movements are intact. Tympanic membranes clear. Nose clear. Oropharynx: The patient has an upper plate that is intact. There is a very carious, partially fractured right upper bicuspid. There is no evidence of submucosal purulence or dental infection. There may very well be an exposed nerve root as it is significantly fractured. NECK: Flexes without guarding and is without adenopathy. LUNGS: Essentially clear to auscultation. HEART: Regular rate and rhythm. No other obvious complaints forthcoming. ASSESSMENT: Dentalgia secondary to fractured tooth. EMERGENCY DEPARTMENT COURSE: In the department, she was given a Percocet p.o. as she does have a ride. She was given a prescription for Oxycodone and acetaminophen, 7.5/500 or 650, 1 q4-6h p.r.n. pain. She states that she has a dentist to follow-up with in one day and she is advised to do so as soon as possible, and return to the emergency department on an as-needed basis. Joseph Gulde Sample Date of Visit: 08/06/2003 CHIEF COMPLAINT: Syncope, feeling lightheaded. HISTORY OF PRESENT ILLNESS: The patient is a 64-year-old Caucasian female who states while working in the heat and humidity, putting up a new awning on a home with her husband the day prior to presentation, she began to feel dizzy, lightheaded, felt that her vision was becoming blurry. She cried out to her husband, who states he went to find her passed out. He carried her into the lanai, put a cool towel on her, laid her down, and she woke up. She states since that time she has continued to feel some mild lightheadedness, and a feeling that she might pass out. She had actually had a complete annual physical the day previously and this morning was to go and have outpatient comprehensive laboratory evaluation, but states while she was driving around to the laboratory, she was feeling lightheaded as though she might pass out, and therefore she came to the emergency department on an ambulatory basis for further evaluation. PAST MEDICAL HISTORY: She is known to have hypoglycemia and has been advised to eat smaller, more frequent meals, but in fact has had no breakfast or lunch prior to this episode that occurred at approximately 1 in the afternoon the day prior to presentation. She has had a very minimal amount of breakfast today; only a bite of a banana and a sip of juice. She had been NPO for fasting labs prior to that intake and prior to arrival here. Also, on her own, she stopped Premarin supplementation about six weeks ago due to concerns over cancer risk. She has tried to supplement some herbal therapy, which she feels has not been helping. She was seen by the nurse practitioner in Dr. Burford's office for her examination earlier this week and was advised Estrace vaginal cream, which may give some local improvement in the vaginal area, but no other oral or more systemic form of estrogen was advised or prescribed. She also noted that she had had a urinary tract infection a couple of weeks ago that she believes was treated with Cipro, and those symptoms seem to have resolved. She has no longstanding history of recurrent syncope. She denies any chest pain, palpitations, shortness of breath, there has been no documented abnormal weight loss or weight gain. There has been no unexplained fever, chills or sweats, other than what she calls hot flashes, and a general feeling of not doing as well ever since she stopped the Premarin. She has a past medical history of hypertension, hypoglycemia. PAST SURGICAL HISTORY: Hysterectomy. SOCIAL HISTORY: She states she smokes 8-10 cigarettes a day and has for over 20 years. She denies alcohol or recreational drug use. ALLERGIES: Stated to BACTRIM. CURRENT MEDICATIONS: Diovan; we are uncertain, but we believe it is 80 mg q.d. She had been on Premarin 1.25 mg daily until she stopped it six weeks ago. Recently, as stated, she was prescribed Estrace vaginal cream. No other definite medications. REVIEW OF SYSTEMS: GENERAL APPEARANCE: Not toxic or acutely ill-appearing. Absence of recent weight loss/gain. CONSTITUTIONAL: No fever, chills, malaise, fatigue. HEENT: No headache, no blurred vision, double vision, eye drainage, earache, ear drainage or tinnitus. NOSE: No runny nose or nose bleed. MOUTH: No sore throat, drooling, inability to open the mouth adequately, or dental pain. NECK: No neck stiffness, masses or swelling. CHEST: No area of crepitus, redness or point tenderness to palpation. LUNGS: No cough, wheezing, feelings of shortness of breath on exertion or at rest. No sputum production, no stridor. HEART: No exertional chest pain, palpitations, orthopnea, no history of valvular heart disease, previous MI or angina. GI/GU: No abdominal distension, change in bowel patterns such as diarrhea or constipation. No hematemesis or hematochezia, or vomiting, no fatty food intolerance. No urinary abnormalities such as burning, stinging, frequency or passage of small amounts. No obvious blood in the urine. No blood in the stool. No urethral discharge/vaginal bleeding or discharge. No penile discharge. EXTREMITY EXAM: No localized swelling, tenderness. No calf pain at rest or with walking. No dependent edema. NEUROLOGICAL EXAM: No syncope, no paralysis, no paresthesias, no seizure activity. No alteration of level of consciousness, confusion, disorientation, slurred speech. PHYSICAL EXAMINATION: GENERAL: This is a 64-year-old Caucasian female. She is awake, alert and oriented. Her temperature is 97.4, pulse rate 90, respiratory rate 18, blood pressure 140/75, pulse oximetry is 96% She appears in no distress when seen. She ambulated into the department and to her bed. HEENT: Atraumatic, normocephalic. Pupils equal, round and reactive to light. Extraocular movements are intact. Tympanic membranes clear. Nose clear. Oropharynx moist without lesions. NECK: Flexes without guarding. There is no neck vein distention; no adenopathy or masses, no palpable thyroid. CHEST WALL: Nontender without retractions. LUNGS: Perhaps slightly diminished but clear to auscultation. HEART: Regular rate and rhythm. No definite gallop noted. There is a slight I/VI systolic murmur at the right upper sternal border. No ectopy noted. ABDOMEN: Bowel sounds positive, normoactive, without hepatosplenomegaly. Negative costovertebral angle tenderness, soft, nontender, no guarding and no rebound, no distention, no pulsatile masses. MUSCULOSKELETAL EXAM: Pelvis, spine, rib cage, facial bones all nontender to palpation. EXTREMITIES: Free range of motion without hot, red, tender joints. No peripheral edema. Negative calf pain, negative cords, negative Homans'. SKIN: Normal turgor without rash. NEUROLOGIC EXAM: Awake, alert and oriented. Cranial nerves II-XII grossly intact. Motor and sensory are symmetrical. Plantars downgoing. No focal deficits noted. EMERGENCY DEPARTMENT COURSE: In the department, orthostatic vital signs were normal. Nevertheless, she was hydrated with one liter of normal saline. In fact, she was given a meal of normal diet. She had an electrocardiogram that showed normal sinus rhythm at a rate of 85, normal axis, normal QRS and PR intervals. There is no evidence of injury, infarct, or abnormal ST segment changes. She had a urinalysis that was within normal limit. Basic metabolic profile was within normal limits. CBC within normal limits. I spoke to Dr. Burford, who is advising that we institute Premarin 1.25 mg q.d. at her discretion, with the consideration of a slower taper rather than the abrupt stoppage that she had instituted before. She is advised smaller, more frequent meals. She is advised increased fluids. She is of course advised that she needs to stop smoking. Other current medications per previous recommendations. She is advised to follow-up with Dr. Burford in the next 24-48 hours in his office and he has given her an appointment time for re-evaluation and discussion of the advisability of ongoing hormonal replacement therapy. DISCHARGE DIAGNOSES: 1. Syncope. 2. Hypoglycemia by history. 3. Vasomotor symptoms related to hormonal therapy discontinuation. She left the department in good condition. Tomas Jacome Sample Date of Visit: 07/27/2003 HISTORY OF PRESENT ILLNESS: The patient is a 74-year-old who comes in with the sudden onset of shortness of breath that started last night. He has been awake all night. PAST MEDICAL HISTORY: Neuropathy, open heart, chronic obstructive pulmonary disease and gout. MEDICATIONS: Allopurinol, Monopril, isosorbide, Coreg. He takes Coumadin for atrial fibrillation, and Slow-Mag and tramadol. SOCIAL HISTORY: He does not smoke or drink. FAMILY HISTORY: Noncontributory. REVIEW OF SYSTEMS: GENERAL APPEARANCE: Nontoxic, does not look acutely ill. No recent weight gain or loss. CONSTITUTIONAL: No fever, chills or fatigue. HEENT: No drainage from the eyes, ears, nose or throat. No headache, blurred vision or double vision. No eye or ear drainage, no earache or tinnitus. No runny nose or nose bleed. No sore throat, drooling, or mouth ulcers. NECK: Supple, no neck vein distension, trachea is in the midline. CHEST: No tenderness to palpation, no crepitus, no redness. RESPIRATORY: Positive for shortness of breath. No cough or sputum production, wheezing or orthopnea, no stridor. CARDIOVASCULAR: No chest pain, palpitations, ABDOMEN: No distention, no change in bowel pattern. No hematemesis, melena or hematochezia. No nausea, vomiting, diarrhea or constipation. GU: No burning, frequency, urgency or blood in the urine. No problems urinating. No urethral or penile discharge. MUSCULOSKELETAL: No history of arthritis, swelling or tenderness. No calf pain or swelling and no edema. NEUROLOGICAL EXAM: No headaches, syncope or seizures. No confusion, disorientation or altered mental status. No slurred speech. PSYCHOSOCIAL: No history of depression. PHYSICAL EXAM: VITAL SIGNS: Temperature 98, pulse 92, respirations 36, blood pressure 172/107, saturations 92%. GENERAL: He appears pale. HEENT: Normal extraocular movements. No facial swelling. Normal sclerae, pupils are equal, round, reactive to light and accommodation, extraocular movements are intact. Tympanic membranes are clear. Nose is clear. Oropharynx is clear, no lesions. NECK: Supple, nontender. Trachea midline. Neck vein distention. CHEST WALL: Tachypnea, retractions. LUNGS: He has some rales. CARDIOVASCULAR: Normal S1, S2. ABDOMEN: No hepatosplenomegaly. EXTREMITIES: Full range of motion. SKIN: No rashes. NEUROLOGICAL EXAM: Alert and oriented x 3. He has a history of neuropathy. Chest x-ray showed congestive heart failure as read by the emergency department doctor. He was put on a nitroglycerin drip and given 80 mg of Lasix. His electrocardiogram shows a right bundle branch block with atrial fibrillation, at a rate of 91, wide QRS, no PVCs as read by the emergency department doctor. DIAGNOSES: 1. Congestive heart failure. 2. Status post coronary artery bypass. 3. Atrial fibrillation. He had normal electrolytes and cardiac enzymes, troponin is pending. His INR was 4.34. His ABG on 3 liters showed saturation of 97%. His white blood cell count was 11,700, hemoglobin 13.9. The electrocardiogram was unchanged from March of 2002. The patient is going to be discussed with Dr. Burford for admission to Dr. Hoffman's service. He may need an Natrecor. Chest x-ray, as I said, showed congestive heart failure, as read by the emergency department doctor. Tomas Jacome Sample Date of Visit: 09/21/2003 CHIEF COMPLAINT/HISTORY OF PRESENT ILLNESS: The patient comes in because he has a history of acid reflux and last night developed acid reflux and she took her Aciphex and took some extra Zantac, and all night was having burning behind the chest and was salivating a lot also. She had a colonoscopy done on Friday, which was apparently okay. She has Crohn's disease. She came in because of the reflux. PAST MEDICAL HISTORY: She has a history of Crohn's, acid reflux and panic disorder. MEDICATIONS: She takes Aciphex once a day, Pentasa, Lomotil, Klonopin, Inderal, Questran, vitamin B12. ALLERGIES: She is not allergic to any medicines. SOCIAL HISTORY: She smokes; does not drink. FAMILY HISTORY: Positive for father dying of myocardial infarction at 60, mother at 80. REVIEW OF SYSTEMS: GENERAL APPEARANCE: Nontoxic, does not look acutely ill. No recent weight gain or loss. CONSTITUTIONAL: No fever, chills or fatigue. HEENT: No drainage from the eyes, ears, nose or throat. No headache, blurred vision or double vision. No eye or ear drainage, no earache or tinnitus. No runny nose or nose bleed. No sore throat, drooling, or mouth ulcers. NECK: Supple, no neck vein distension, trachea is in the midline. CHEST: No tenderness to palpation, no crepitus, no redness. RESPIRATORY: No cough or sputum production, wheezing or shortness of breath, no orthopnea, no stridor. CARDIOVASCULAR: No chest pain, palpitations, No history of heart disease, previous myocardial infarction or angina. ABDOMEN: only positive for epigastric pain. No distention, no change in bowel pattern. No hematemesis, melena or hematochezia. No nausea, vomiting, diarrhea or constipation. GU: No burning, frequency, urgency or blood in the urine. No problems urinating. No vaginal bleeding or discharge. MUSCULOSKELETAL: No history of arthritis, swelling or tenderness. No calf pain or swelling and no edema. NEUROLOGICAL EXAM: No headaches, syncope or seizures. No confusion, disorientation or altered mental status. No slurred speech. PSYCHOSOCIAL: No history of depression. PHYSICAL EXAM: VITAL SIGNS: Temperature 99.3, pulse 98, respirations 16, blood pressure 137/84, pain on a scale of 1/10 is a 3, saturation 99%. GENERAL: She is alert, and really in no distress. HEENT: Normal extraocular movements. No facial swelling. NECK: Trachea in the midline. CHEST WALL: No retractions. LUNGS: Clear to auscultation, no rales, no wheezes. CARDIOVASCULAR: Normal S1, S2, no murmurs or gallops. ABDOMEN: No hepatosplenomegaly. EXTREMITIES: Full range of motion. NEUROLOGICAL EXAM: Alert and oriented x 3. SKIN: No rashes. She had an electrocardiogram read by the emergency department doctor that showed normal sinus rhythm, good R-wave progression, normal PR and QRS and normal axis. She had a rate of 88. Read by the emergency department doctor. Acute abdominal series showed some non-specific fluid levels as read by the emergency department doctor. CK index was negative. CPK was 36, lipase was normal. Amylase was normal and electrolytes were normal. The SGOT is slightly elevated. The INR was normal. White blood cell count was 14.9 with a hemoglobin of 15 and she had a negative troponin. She got a GI cocktail and Pepcid and she feels much better. DIAGNOSES: 1. Crohn's disease. 2. Dyspepsia. I will discuss with Dr. Keith for disposition. Robert Sharkey Sample Date of Visit: 09/14/2003 CHIEF COMPLAINT: Fever, sore throat, earache. HISTORY OF PRESENT ILLNESS: This is a 13-year-old black female who denies any major medical problems. She states she has had swelling of feet in the past, has had none recently. The patient says she has been sick for about five days. She had a sore throat. Her throat has gotten so sore that it hurts to swallow There has been no chest pain, palpitations, no fever, no shaking chills. The patient does have some earache. There is no vomiting, no diarrhea, no abdominal pain, no syncope, no other complaints. There is no rash, no discharge. PAST MEDICAL HISTORY: As above. FAMILY HISTORY: No major medical problems. SOCIAL HISTORY: Non-smoker, non-drinker. ALLERGIES: Denies. MEDICATIONS: Denies. REVIEW OF SYSTEMS: There are no eye problems, no cardiovascular, no neurologic, allergic and no psychiatric problems. Other systems reviewed and are negative. PHYSICAL EXAMINATION: VITAL SIGNS: See chart. HEENT: Eye examination is normal; ears, nose, throat is normal, except for the tonsils, which were quite enlarged, almost kissing, with exudates on both. The uvula is midline. There is no stridor. CARDIOVASCULAR: Heart is regular tachycardia, no murmurs. RESPIRATORY: Lungs are clear. GASTROINTESTINAL: Abdomen is soft, nontender. GENITOURINARY/BACK: No costovertebral angle tenderness. NEUROLOGIC: Nonfocal. LYMPHATIC: There is no adenitis. SKIN: There are no raised lesions, no rash. EMERGENCY DEPARTMENT COURSE: The patient is given Tylenol, intravenous fluids. Her temperature has calmed down; her heart rate has calmed down. Dr. Liu is consulted and wishes the patient to get Decadron intravenously followed by prednisone, and the patient is given Bicillin CR IM and he will see the patient in his office on Monday or Tuesday. The patient is discharged in stable condition, well hydrated and non-toxic. Robert Sharkey Date of Visit: 08/31/2003 CHIEF COMPLAINT: Stomach pain. HISTORY OF PRESENT ILLNESS: This is a 72-year-old white female with history of thyroid disease, hypertension, jaw surgery, history of pulmonary embolus and a passive Greenfield filter. The patient states yesterday afternoon she started feeling bad. She had some nausea and vomiting and some stomach pain. It did leave and did occur again in the wee hours of the morning. There has been no fever, chills, headache, sore throat. There is no back pain. She has palpitations. No extremity problems, no recent trauma. No other complaints. PAST MEDICAL HISTORY: As above. FAMILY HISTORY: No major medical problems. SOCIAL HISTORY: Non-smoker, non-drinker. ALLERGIES: Denies. MEDICATIONS: See chart. REVIEW OF SYSTEMS: There are no eye problems, no ears, nose, throat complaints. There is no allergic, skin, no psychiatric problems. Other systems reviewed and are negative. PHYSICAL EXAMINATION: VITAL SIGNS: See chart. HEENT: Eye examination is normal; ears, nose, throat is normal. Mouth and throat are clear. CARDIOVASCULAR: Heart is regular, tachycardia, no murmurs. RESPIRATORY: Bibasilar crackles. GASTROINTESTINAL: Abdomen is soft. There is some diffuse epigastric tenderness, no rebound or guarding. GENITOURINARY/BACK: No costovertebral angle tenderness. NEUROLOGIC: Non-focal. LYMPHATIC: There is no adenitis. SKIN: No open lesions. She is diaphoretic. EMERGENCY DEPARTMENT COURSE: Electrocardiogram shows a sinus tachycardia, left axis, atrial enlargement, left ventricular hypertrophy and Q waves in V2 and V3 with ST changes. DIAGNOSES: Acute anterior septal myocardial infarction. LABORATORY: Did show an elevated troponin at 16. CPK is also elevated in its MB fraction. White blood cell count is normal; hemoglobin and hematocrit is normal. Urinalysis does show hematuria and proteinuria. Acute abdominal series is done, because of the patient's epigastric tenderness. There is no evidence of aneurysm or perforation. There is a Greenfield filter in place. DIAGNOSIS: Anterior septal myocardial infarction. PLAN: Since the patient is from out of town, Cogent was consulted. Dr. Liccini was consulted. The patient will be moved to Health Park for possible intervention. Critical care time: 1 hour and 5 minutes. Edward Salko Sample Date of Visit: 09/21/2003 CHIEF COMPLAINT/HISTORY OF PRESENT ILLNESS: This is a 69-year-old Caucasian female seen in the emergency department with the chief complaint of shortness of breath. The patient has had progressively worsening dyspnea for the past four days. Minimal sputum production. She is increasingly weak. She is also having altered mental status. She is quite somnolent but responsive. She appears acutely ill. PAST MEDICAL HISTORY: Significant for end-stage chronic obstructive lung disease. In addition, she has osteoporosis. Her last admission was 06/23/2003. At that time she was found to have an abnormal chest x-ray. The patient has a history of tobacco abuse. PAST SURGICAL HISTORY: Includes cataractectomy and back surgery as well as an open reduction internal fixation of her right hip. MEDICATIONS: Fosamax, Theo-24, Aciphex, Zyrtec, Nasarel, Foradil, Pulmicort, albuterol, Xanax, Ultracet, Singulair, prednisone, Lasix, Humibid, Flexeril and oxygen. ALLERGIES: CODEINE INTOLERANCE. SOCIAL HISTORY: The patient does reside with her husband. She is an ex-smoker, as noted. She uses alcohol socially. FAMILY HISTORY: Noncontributory with no evidence of any familial pulmonary disease. REVIEW OF SYSTEMS: As noted, the patient is extremely weak, with poor appetite. No real change in bowel or bladder habits. She wears corrective lenses. No melena, hematemesis or hematochezia reported. The patient has had some weight loss. Abnormal chest x-ray showing a right apical volume loss, possible mass lesion. Full review otherwise negative. PHYSICAL EXAMINATION: VITAL SIGNS: Temperature is 97.6, blood pressure 140/90, heart rate 83, respirations 24, O2 saturation initially were 56% on oxygen. On a non-rebreather, she improved to 100%. Weight was 145 pounds. HEENT: She is normocephalic. Ears: Clear. Nose and throat are clear. Sclerae anicteric. Extraocular muscle function full. NECK: Supple. Trachea appeared midline. No carotid bruits, no thyromegaly. CHEST: Revealed marked thoracic kyphosis with increased AP diameter. Markedly diminished breath sounds. Minimal air exchange. HEART: Irregular. No murmurs or gallops. ABDOMEN: Scaphoid, no masses. EXTREMITIES: Negative for cyanosis or clubbing. No peripheral cyanosis. NEUROLOGIC EXAM: Revealed the patient to be lethargic. She moved all extremities. Integument was negative for any stigmata of internal disease. PERTINENT LABORATORY AND X-RAY FINDINGS: A 12-lead electrocardiogram demonstrated what appeared to be a sinus arrhythmia versus frequent premature atrial contractions. She had left ventricular hypertrophy by electrical criteria. She also had what appeared to be right atrial enlargement. Her QRS axis appeared normal. Her chest x-ray showed persistent volume loss in the right upper lobe. Findings suggestive of a need to review previous films. Her initial ABG on a non-rebreather revealed pH of 7.239 with pCO2 of 85.2, pO2 of 353.5. Follow-up gas on 3 liters FIO2: pH of 7.233, pCO2 of 90.5, pO2 of 77.9. Repeat ABG on BiPAP at 14 and 5, pH of 7.309, pCO2 of 73.9, pO2 of 65.8 with % saturation of 94.1%, with supplemental oxygen at 6 liters per minute. Theophylline level was 16.2, white blood cell count 19,200 with hemoglobin and hematocrit of 13.6/40.4. Differential on the white count was 86% neutrophils, 0 lymphs. PT/aPTT were normal. Electrolytes were normal. Glucose 133, BUN and creatinine were 10 and 0.7. Liver function tests normal. Amylase and lipase normal. Total CK was 43, CK-MB was 9.2 nanograms/ml. CK-MB index was at 21.4. Troponin was 0.5. CLINICAL IMPRESSION: 1. Respiratory failure. 2. Exacerbation of chronic obstructive pulmonary disease. 3. History of osteoporosis. EMERGENCY DEPARTMENT TREATMENT AND DISPOSITION: As noted, the patient did have the above evaluation. In full discussion with the patient's husband and the patient herself, there was no desire for intubation. We did proceed with BiPAP at 14 and 5. Cultures were pending. The patient did receive Solu-Medrol 125 mg intravenously, continued oxygen at 6 liters supplemental with the BiPAP and Levaquin 500 intravenously. Admit orders were received per Dr. Feroz. The patient was admitted to the medical intensive care unit in guarded condition with a poor prognosis. Critical care time was approximately 50 minutes excluding procedure. Edward Salko Sample Date of Visit: 08/31/2003 CHIEF COMPLAINT/HISTORY OF PRESENT ILLNESS: This 79-year-old Caucasian female is seen in the emergency department with the chief complaint of lightheadedness. The patient stated that she had gotten up about 9 a.m. The patient got herself ready for church, had a small bowel of cereal and at about 10 to 10 took all of her medications and went on to church. At church, she became lightheaded. She felt very lightheaded to the point that she almost passed out. EMS was summoned. There was no headache, no diaphoresis, no chest pain. She denies any shortness of breath. The patient has had about three of four episodes similar to this with similar presenting circumstances. The patient was seen at Cape Coral Hospital emergency department on 07/12/03. At that time she was treated for possible exacerbation of Ménière's disease. The patient had no vertiginous symptoms. The patient was seen by her primary care physician as well as a nephrologist within the last week. She has been given a relatively clean bill of health regarding her chronic problems. She was to the hematologist for a hemoglobin and hematocrit due to her chronic Procrit therapy. Her hemoglobin and hematocrit have remained stable and she did not require repeat injection. The patient is on multiple blood pressure medications. Several of these medications are vasodilators. PAST MEDICAL HISTORY: Is well documented on her previous charts. To summarize it, the patient did have a previous gastrointestinal bleed within the last six months. She had been on chronic warfarin therapy for deep venous thrombosis. She has chronic renal insufficiency with a history of renal artery stenosis. She has chronic hypertension, history of coronary artery disease with previous myocardial infarction and coronary artery stenting. She has a history of renal artery bypass. She has a chronic anemia of multiple factors, including chronic disease and chronic renal insufficiency. MEDICATIONS: Acrinol, Norvasc, Atenolol, Cozaar, Imdur, hydrochlorothiazide, aspirin, Pepcid, Clonidine. ALLERGIES: MOTRIN, IODINE AND INTRAVENOUS PYELOGRAM CONTRAST. SOCIAL HISTORY: She is married. She is a non-smoker and non-drinker. FAMILY HISTORY: Noncontributory. REVIEW OF SYSTEMS: As in History of Present Illness. SKIN: Denies rashes, lesions or urticaria. HEENT/SINUS: No ear pain or drainage bilaterally. Denies sore throat or difficulty swallowing. No tongue or throat swelling, denies hoarseness or change in voice. No maxillary or frontal sinus pain bilaterally. Denies nasal congestion or drainage. No hearing loss or changes. Denies photophobia, blurred vision or changes in vision, no eye pain, pressure, itching or drainage. NECK: Denies neck pain, stiffness or swelling. RESPIRATORY: No cough, shortness of breath, wheezing, stridor or hemoptysis. Denies pain with deep inspiration. Denies sputum production, night sweats or pleuritic pain. CARDIAC: Denies chest pain, pressure or tightness. No nocturnal dyspnea or diaphoresis. Denies extremity swelling or edema. No palpitations, tachycardia, irregular rhythm or cyanosis. GASTROINTESTINAL: No abdominal pain or cramping. Denies nausea, vomiting, diarrhea or constipation. Appetite good and taking fluids well. Denies blood in stool or black tarry stool. No unexplained weight loss or gain. Denies abdominal distention, flatulence, jaundice or hematemesis. GENITOURINARY: Patient denies urinary symptoms. No urinary incontinence, hesitance or retention. Denies change in urinary pattern. No bilateral flank pain. MUSCULOSKELETAL: Denies joint pain, swelling or erythema. No muscle cramps or spasms. No numbness or tingling to extremities or digits. No limitation in range of motion to joints as compared to their normal. NEUROLOGICAL: Patient denies headache, vertigo, dizziness or facial weakness. No change in motor or sensory function. Denies paralysis, convulsions or change in coordination. No difficulty with speech, slurred speech or aphasia. HEMATOLOGIC: Denies any blood dyscrasia, easy bleeding or bruising. ENDOCRINE: Patient denies goiter, exophthalmus, intolerance to heat or cold, dryness of hair or skin. Denies polydipsia, polyphagia or polyuria. Her old charts were reviewed in detail. There has been essentially no change since her Cape Coral Hospital emergency department visit of 07/12/03 except for her presenting complaint. Review of her labs suggests that her BUN and creatinine have remained relatively stable. In addition, her hemoglobin and hematocrit have been stable. PHYSICAL EXAMINATION: GENERAL: The patient is awake, alert and oriented. VITAL SIGNS: Temperature 98.6, blood pressure is 139/56, heart rate 50, respirations 20, O2 saturation 100%, weight is 137 pounds. HEENT: Normocephalic. Ears, nose and throat are clear. NECK: Supple, no jugular venous distention or bruits, no thyromegaly. CHEST: Symmetrical, no bony tenderness. LUNGS: Clear. CARDIAC: Regular. ABDOMINAL: Soft, no masses and no organomegaly. EXTREMITIES: Free of edema, cyanosis , digital clubbing. Neuromuscular examination revealed no motor or sensory deficits. No nystagmus. No peripheral bruits. Reflexes are physiologic. Plantar response is downgoing. SKIN: No stigmata of internal disease. PERTINENT LABORATORY AND X-RAY FINDINGS; A 12-lead electrocardiogram demonstrates sinus bradycardia with a rate of 48 beats per minute. She did have a first degree AV block. She had ST/T wave changes that appeared non-specific. T-waves noted in III and aVF of questionable clinical significance. Her chest x-ray showed no active disease. CT of the brain showed chronic changes with no acute bleed. Electrolytes were normal. BUN and creatinine were 68 and 3.3. Magnesium was 2.0. Cardiac enzymes negative. TSH was 5.358. D-dimer was 1.19. Her aPTT was 21.6, her prothrombin time was 14.3. Hemoglobin and hematocrit were 14.2 and 43. White blood cell count 9,000. CLINICAL IMPRESSION: 1. Near-Syncope, rule out cardiac versus neurologic etiology. 2. Rule out untoward drug reaction. 3. Chronic hypertension. 4. history of chronic renal insufficiency. 5. History of cerebrovascular disease. 6. History of atherosclerotic heart disease. 7. History of coronary artery disease. 8. History of peripheral vascular disease. EMERGENCY DEPARTMENT TREATMENT AND DISPOSITION: As noted, the above workup was carried out. The patient did not have any orthostatic symptoms. The patient remained hemodynamically stable. She was monitored throughout her emergency department visit with no evidence of any malignant arrhythmia. The patient did tolerate a diet. The patient's case was discussed with Dr. Robert Bourgeois covering for Dr. Sebastian Draulans. Arrangements will be made for outpatient follow-up with Dr. Draulans. Verbal and written information regarding the patient's visit given to she and her husband. Richard Kinder Sample Date of Visit: 09/13/2003 CHIEF COMPLAINT: Head injury. HISTORY OF PRESENT ILLNESS: This is a 45-year-old male who presented to the emergency department after suffering a head injury. He was working at the resort that employs him when he attempted to open a door. As he put his hand on the door, the door flew open, striking him in the head. There was a brief period of loss of consciousness and the patient is complaining of nausea. He has had no vomiting. He denies neck pain or neck stiffness. He denies any motor or sensory loss. He denies vision change or hearing loss. REVIEW OF SYSTEMS: All systems are reviewed and are negative with the exception of those mentioned above. PAST MEDICAL HISTORY: Positive for hypertension. CURRENT MEDICATIONS: Lotrel. MEDICATION ALLERGIES: None. PAST SURGICAL HISTORY: Negative. SOCIAL HISTORY: The patient is a married male who lives and works locally. He smokes cigarettes. He denies the use of alcohol or recreational drugs. FAMILY HISTORY: Unremarkable. PHYSICAL EXAMINATION: GENERAL: The patient is well nourished middle-aged male. VITAL SIGNS: Blood pressure is 148/115, pulse 110 and regular, respirations 22 and unlabored, afebrile. O2 saturation is 98% on room air. NEUROLOGIC: The patient is awake and alert, oriented x 3. Motor strength is full and symmetric throughout. HEENT: Examination of the head reveals a 3 cm long vertical laceration just above the hairline in the midline. The wounds edges are separated and there has been moderate bleeding. The bleeding at this time is almost completely controlled. There is no palpable underlying bony deformity. Orbits, zygomas, mandible palpated intact. Occlusion is within normal limits. The pupils equal, round and reactive. Extraocular movements are full. The sclerae and conjunctivae are clear. Oropharynx is without swelling or exudate. The uvula is midline. Mucous membranes are moist. Dentition is intact. There is no intraoral bleeding. The nose is without swelling or deformity. The nasal septum is midline and there is no septal hematoma. There is bleeding or discharge at this time. NECK: The neck is supple and nontender to general range of motion. The trachea is midline. There is no swelling or deformity. There is no crepitus or subcutaneous air. CT scan of the head is interpreted by the emergency department physician [radiologist is not available to read this study], as without evidence of fracture, bleed, or mass affect. A small amount of extracranial soft tissue swelling is noted over the frontal region. PROCEDURE: After obtaining permission from the patient, the wound was cleaned and draped in the usual fashion. The wound was irrigated with dilute Betadine and inspected for retained foreign material. None was found. The wound was then closed with staples. ASSESSMENT: 1. Closed head injury. 2. Scalp laceration. Richard Kinder Sample Date of Visit: 08/23/2003 CHIEF COMPLAINT: Chest pain. HISTORY OF PRESENT ILLNESS: This 39-year-old male presents to the emergency department with complaints of chest pain. The pain is described as a pressure in the center of his chest that radiates to the left arm. He is also short of breath and nauseated. The patient states that he has had an myocardial infarction in the past and these symptoms are similar to what he experienced with that myocardial infarction. He was given nitroglycerin by EMS en route to the hospital and had some improvement. REVIEW OF SYSTEMS: All systems are reviewed and are negative with the exception of those mentioned above. PAST MEDICAL HISTORY: Positive for myocardial infarction in the past. CURRENT MEDICATIONS: Aspirin. MEDICATION ALLERGIES: None. PAST SURGICAL HISTORY: Negative. SOCIAL HISTORY: The patient is a single male who lives locally. He uses tobacco and alcohol. He denies the use of recreational drugs. FAMILY HISTORY: Positive for cardiac disease. PHYSICAL EXAMINATION: GENERAL: The patient is a well nourished young man. VITAL SIGNS: Blood pressure is 124/66, pulse 118 and regular, respirations 20 and unlabored, afebrile. O2 saturation is 96% on room air. NEUROLOGIC: The patient is awake and alert, oriented x 3. Cranial nerves II through XII are grossly intact. Motor strength is full and symmetric throughout. HEENT: The pupils are round and reactive. The sclerae and conjunctivae are clear. Oropharynx is without swelling or exudate. The uvula is midline. Mucous membranes are moist. NECK: The neck is supple and nontender to general range of motion. The trachea is midline. The thyroid is not enlarged. There is no regional lymphadenopathy. CARDIOVASCULAR: Heart demonstrates a regular rhythm at 110 beats per minute without a murmur. No rubs or gallops are heard. EXTREMITIES: Without clubbing, cyanosis, or edema. There is no jugular venous distention. PULMONARY: Lungs are clear with decreased expansion left and right. No rales, rhonchi, or wheezing are heard. GASTROINTESTINAL: The abdomen is soft, flat, nontender, with good bowel sounds. SKIN: The skin is clear, without rash. The patient is improved on arrival in the emergency department. He is placed on a cardiac monitor and given supplemental oxygen by nasal cannula. An intravenous is established. His care is turned over to Dr. Edward Salko at change of shift. Please see his follow-on dictation for laboratory and x-ray results, diagnosis, and disposition. William Burkey Sample Date of Visit: 07/03/2003 CHIEF COMPLAINT/HISTORY OF PRESENT ILLNESS: The patient is a 16-year-old female who developed a bad headache last night. She had seen a doctor yesterday who thought that she had a sinus infection and was started on a Z-Pack and aspirin. The aspirin seemed to help. The pain is better but it was quite severe last evening. She was kind of lying down with her head cocked when it occurred. PAST MEDICAL HISTORY: Otherwise unremarkable. PAST SURGICAL HISTORY: Negative. MEDICATIONS: Z-Pack and aspirin. SOCIAL HISTORY: She smokes. She does not drink or use recreational drugs. FAMILY HISTORY: Otherwise noncontributory. REVIEW OF SYSTEMS: ??CONSTITUTIONAL No fever, chills, rigors, weight loss. HEENT: The patient denies visual disturbances, denies ear pain, ear drainage or hearing changes. NOSE: The patient denies discharge, bleeding, congestion or pain. MOUTH: The patient denies mouth sores, pain, excessive saliva; denies dental discomfort. NECK: The patient denies pain or discomfort, no difficulty swallowing. CHEST: No pain. LUNGS: No difficulty breathing, no pain, no congestion, no shortness of breath. HEART: No palpitations. ABDOMEN: No pain, no distention. BACK: No back pain, no vertebral tenderness GI: Denies excess flatulence, diarrhea, constipation; denies nausea or vomiting. GU: The patient denies frequency, urgency, pain on urination, denies hematuria. EXTREMITIES: The patient denies arm pain, joint discomfort or weakness. SKIN: The patient denies lesions, sores, rashes; denies swelling. NEUROLOGICAL: No weakness, denies change in concentration, denies paresthesia, denies anesthesia. PHYSICAL EXAMINATION: VITAL SIGNS: Temperature 97.7, pulse 80, respirations 18, blood pressure 119/70. GENERAL: The patient appears healthy, alert oriented and in no distress. HEENT: HEAD: Normocephalic, no evidence of trauma. Eyes are reactive to light and accommodation, extraocular movements are intact. Ears are patent, not injected. Nose is clear. Throat is clear. Oropharynx is not injected, tongue and uvula are midline. NECK: Supple, without lymphadenopathy or thyromegaly, no jugular venous distension or bruits. CHEST WALL: Nontender, no scars. LUNGS: Clear to auscultation and percussion, no wheezes, rales or rhonchi. HEART: Regular, without murmur or gallop, no thrills. ABDOMEN: Soft, nontender, no localizing signs, no rebound or guarding, no hepatosplenomegaly, normoactive bowel sounds. BACK: No localizing signs, no CVA pain, no vertebrae tenderness. MUSCULOSKELETAL: Essentially normal, able to ambulate without difficulty. There is no crepitation or deformity. Grips are equal, tone is symmetrical. NEUROLOGICAL EXAM: Grossly unremarkable with no focal findings. Cranial nerves II/XII are intact, reflexes are equal. SKIN: No edema, ulcers, lesions, cyanosis, clubbing or edema. PSYCHIATRIC: Grossly normal, no mental status changes, no delusions, no suicidal or homicidal ideation. CT of the head is unremarkable for any acute pathology. Radiology reading is pending. The patient has remained clinically stable. The patient was given a Darvocet N100. The pain symptoms were gone. DIAGNOSIS: Headache. PLAN: Darvocet N100, 1 p.o. q6h p.r.n. Continue her other medications. She should return here if worse, at which point might consider an MRI or even a lumbar puncture. The patient is clinically stable at the time of this dictation. William Burkey Sample Date of Visit: 08/31/2003 CHIEF COMPLAINT: Nosebleed. HISTORY OF PRESENT ILLNESS: This is a 68-year-old male who returns here after a recurrent nosebleed. Apparently he was treated with Neo-Synephrine drops but has continued to have symptoms. The patient is otherwise relatively stable, not acutely ill or distressed. PAST MEDICAL HISTORY: remarkable for ulcers and anemia. PAST SURGICAL HISTORY: He has had surgery for stomach ulcers. ALLERGIES: None. MEDICATIONS: Iron pills, water pills. SOCIAL HISTORY: He smokes, does not drink or use recreational drugs. FAMILY HISTORY: Otherwise noncontributory. REVIEW OF SYSTEMS: CONSTITUTIONAL No fever, chills, rigors, weight loss. HEENT: The patient denies headache, denies visual disturbances, denies ear pain, ear drainage or hearing changes. NOSE: Nosebleed as noted in History of Present Illness. The patient denies congestion or pain. MOUTH: The patient denies mouth sores, pain, excessive saliva; denies dental discomfort. NECK: The patient denies pain or discomfort, no difficulty swallowing. CHEST: No pain. LUNGS: No difficulty breathing, no pain, no congestion, no shortness of breath. HEART: No palpitations. ABDOMEN: No pain, no distention. BACK: No back pain, no vertebral tenderness GI: Denies excess flatulence, diarrhea, constipation; denies nausea or vomiting. GU: The patient denies frequency, urgency, pain on urination, denies hematuria. EXTREMITIES: The patient denies arm pain, joint discomfort or weakness. SKIN: The patient denies lesions, sores, rashes; denies swelling. NEUROLOGICAL: No weakness, denies change in concentration, denies paresthesia, denies anesthesia. PHYSICAL EXAMINATION: VITAL SIGNS: Temperature 95.3, pulse 78, respirations 18, blood pressure 160/90. GENERAL: The patient looks relatively stable. HEENT: HEAD: Normocephalic, no evidence of trauma. Eyes are reactive to light and accommodation, extraocular movements are intact. Ears are patent, not injected. Nose: There are areas of previous bleeding from the left naris. Otherwise stable. There is no gross active bleeding at this time. Throat is clear. Oropharynx is not injected, tongue and uvula are midline. NECK: Supple, without lymphadenopathy or thyromegaly, no jugular venous distension or bruits. CHEST WALL: Nontender, no scars. LUNGS: Clear to auscultation and percussion, no wheezes, rales or rhonchi. HEART: Regular, without murmur or gallop, no thrills. ABDOMEN: Soft, nontender, no localizing signs, no rebound or guarding, no hepatosplenomegaly, normoactive bowel sounds. BACK: No localizing signs, no CVA pain, no vertebrae tenderness. MUSCULOSKELETAL: Essentially normal, able to ambulate without difficulty. There is no crepitation or deformity. Grips are equal, tone is symmetrical. NEUROLOGICAL EXAM: Grossly unremarkable with no focal findings. Cranial nerves II/XII are intact, reflexes are equal. SKIN: No edema, ulcers, lesions, cyanosis, clubbing or edema. PSYCHIATRIC: Grossly normal, no mental status changes, no delusions, no suicidal or homicidal ideation. A nasal tampon was applied and the patient was to leave in for 24 hours and to follow-up with the VA Clinic on Tuesday. He can return here if problems. Jason Wilson Sample Date of Visit: 09/02/2003 CHIEF COMPLAINT: Difficulty breathing. HISTORY OF PRESENT ILLNESS: The patient is a 33-year-old female with history of asthma who has had cough and congestion for two days with increased difficulty breathing, not relieved by her albuterol inhaler. She called the ambulance to bring her in to the hospital. The patient denies any chest pain, no loss of consciousness. She has no history of deep venous thrombosis, pulmonary embolism or coronary artery disease. She has had episodes like this before but feels worse today. She complains also of a lot of “sinus drainage”. REVIEW OF SYSTEMS: All systems reviewed and negative, other than as mentioned above in the History of Present Illness. PAST MEDICAL HISTORY: Asthma. SURGERIES: Surgery for scoliosis with Harrington rod placement. MEDICATIONS: Albuterol inhaler. ALLERGIES: None. SOCIAL HISTORY: Smokes tobacco and marijuana, denies alcohol use. PHYSICAL EXAMINATION: VITAL SIGNS: She is afebrile. Temperature 96, pulse 99, respirations 20, blood pressure 124/82, O2 saturation 99% on room air, which was normal. GENERAL: The patient is a well developed, well nourished female with nasal congestion and a dry cough. She is in no respiratory distress. HEENT: Head is normocephalic, atraumatic. Conjunctivae are pink. Mucous membranes moist, oropharynx clear. NECK: Supple with no jugular venous distention or meningismus. LUNGS: Show mild scattered expiratory wheeze with adequate aeration, no accessory muscle use. ABDOMEN: Nontender to palpation. SKIN: Warm and dry. EXTREMITIES: Without edema, cyanosis or tenderness. NEUROLOGIC: Conversant, no apparent deficit. MEDICAL DECISION-MAKING: The differential diagnosis includes upper respiratory infection, viral syndrome, asthma exacerbation, doubt pneumonia or pulmonary embolism. EMERGENCY DEPARTMENT COURSE: She was given prednisone 50 mg p.o. and a combination albuterol and Atrovent updrafts. On re-examination she reports she felt much better. Her lungs were clear. She is appropriate for discharge home. DISPOSITION: I wrote a prescription for prednisone and Guaifenex to take as directed. Follow-up with her doctor at the Family Health Center by calling tomorrow. Return is worse or concerned. FINAL DIAGNOSES: 1. Acute asthma exacerbation. 2. Upper respiratory infection. Jason Wilson Sample Date of Visit: 09/02/2003 CHIEF COMPLAINT: Abdominal pain. HISTORY OF PRESENT ILLNESS: The patient is a 79-year-old male who comes in with intermittent abdominal pain since about 4 p.m. this afternoon. He has had waves of generalized abdominal pain and cramping sensation, which will come and go. Currently the pain is described only as very mild. He does complaint of feeling bloated. He has been using stool softeners intermittently for the past few months for constipation. He reports that his constipation started after having what sounds like a barium enema a few months ago at the VA Clinic. He was told the results were normal. He has had no nausea or vomiting, no fever, no back pain, no dysuria. He has a history of an abdominal aneurysm repair, also a history of kidney stones, but he has no flank pain or hematuria. His primary is Dr. Del Sol. REVIEW OF SYSTEMS: All systems reviewed and negative, other than as mentioned above in the History of Present Illness. PAST MEDICAL HISTORY: Diabetes and hypertension. SURGERIES: Abdominal aortic aneurysm repair. MEDICATIONS: Glyburide, Atenolol and Lisinopril. ALLERGIES: None SOCIAL HISTORY: Denies tobacco, alcohol or drug use. PHYSICAL EXAMINATION: VITAL SIGNS: He is afebrile. Pulse 76, respirations 16, blood pressure 150/80. GENERAL: The patient is a well developed, well nourished male who appears to be in no acute distress. HEENT: Head is normocephalic, atraumatic. Conjunctivae are pink. Mucous membranes are slightly dry. NECK: Supple. LUNGS: Clear. ABDOMEN: Soft, slightly distended and tympanitic with a mild generalized tenderness to palpation, no focal tenderness, no peritoneal signs or guarding and no pulsatile mass. SKIN: Warm and dry. EXTREMITIES: show no edema or deformity and symmetrical pulses. NEUROLOGIC: He is conversant, he has no apparent focal deficit. MEDICAL DECISION-MAKING: The differential diagnosis includes constipation, obstruction, urinary tract infection, doubt intraabdominal infection or aneurysm rupture. EMERGENCY DEPARTMENT COURSE: He had an intravenous placed and was given MS 2 mg intravenously and Phenergan 12.5 mg intravenously for complaints of nausea and pain. He was given 500 cc saline bolus for hydration. Studies done in the emergency department that I reviewed included an acute abdominal series, which did show increased amount of fecal matter with a non-specific bowel gas pattern, no free air and no obstruction. These were reviewed with radiology, who is in agreement. Laboratory studies included a normal chemistry panel except for glucose of 185, liver function studies and lipase were normal. Troponin was negative at less than 0.3. Urinalysis with no signs of blood or infection, normal specific gravity. CBC shows a normal white blood cell count of 9.8 and normal hemoglobin. Electrocardiogram showed sinus rhythm at 73 with non-specific flattening of the T-waves and inverted T-wave inferiorly. There was no ST elevation nor depression, and no ectopy. Upon re-examination, the patient was sitting up. He appeared comfortable. He was drinking a cup of ice water. His abdominal examination is benign. He stated that he was essentially asymptomatic at this time and wanted to be discharged home. He does tell me that he has been having trouble with constipation since his procedure at the VA Clinic, also his diet has been off recently since he has been visiting his wife at Lee Convalescent. The patient appeared appropriate for discharge home at this time. DISPOSITION: He is to call Dr. Del Sol, his primary physician, first thing in the morning. He was a given a bottle of magnesium citrate to drink one-half bottle with 4 ounces of water and repeat in one hour if no bowel movement. He was instructed to return here immediately if worse or concerned, which would include increasing pain, fever, or vomiting. FINAL DIAGNOSES: 1. Abdominal pain. 2. Constipation. ADDENDUM/3381026/G55 The patient received a dose of MS 2 mg and Phenergan 12.5 mg now about 3 hours ago during his initial evaluation. He will be discharged home, although the patient did drive himself here. He is completely awake and alert; he is ambulatory without difficulty. He states that he feels fine and has no effect of the medication at all and is safe to drive home. In my opinion, the patient is appropriate to drive home at this time as he is showing no ill effects from the small dose of medicine. He is neurologically intact, converses appropriately and shows no signs of incoordination. James Gostigian Sample Date of Visit: 08/31/2003 CHIEF COMPLAINT: Cough, wheezing. HISTORY OF PRESENT ILLNESS: The patient is a 2 and ½-year-old child who is being brought to the emergency department by parents for evaluation and treatment of the above named symptoms. The child has been ill since approximately 7 a.m. the day of arrival in the emergency department. The parents noted that the child was wheezing. There has not been any vomiting, no diarrhea, no irritability. There has been a cough. The child is still taking fluids well. REVIEW OF SYSTEMS: All systems reviewed and are negative except for the items as mentioned above. PAST MEDICAL HISTORY: Similar episodes of wheezing and cough in the past. SOCIAL HISTORY: Lives with the parents. FAMILY HISTORY: Positive for asthma as a child in the mother. ALLERGIES: None. MEDICATIONS: Tylenol. PHYSICAL EXAMINATION: VITAL SIGNS: Reviewed. GENERAL: The child is awake, alert, responsive and not in any acute distress. HEENT: Ears: Both tympanic membranes are clear. External canals are normal. Lips and mucous membranes are moist. Throat: No injection, exudates or tonsillar hypertrophy. NECK: Supple, no lymphadenopathy, no rigidity. CHEST: The patient initially did have use of accessory muscles. HEART: S1, S2 regular. LUNGS: Good bilateral breath sounds with expiratory wheezes heard. ABDOMEN: Soft, nontender. SKIN: Warm and dry, no rash. TESTS INTERPRETED BY THE EMERGENCY DEPARTMENT PHYSICIAN: Pulse oximetry on room air initially was 95%, improved to 98% prior to discharge, which was normal oxygenation, and is also on room air. Chest x-ray was normal. INTERVENTION: Medications - Proventil and Atrovent updraft x 2 was administered. This was repeated x 1 as was a regular Proventil updraft. The patient was given Prelone syrup 15 mg p.o. after which condition was improved. Re-examination showed lungs mostly clear with only minimal scattered wheezing heard. The case was discussed with the patient's parents in the emergency department prior to discharge. DIAGNOSES: 1. Wheezing. 2. Bronchiolitis. DISPOSITION: Discharged home. PRESCRIBED MEDICATIONS: Prelone syrup and Zithromax suspension. The parents were instructed to increase fluid intake and to follow-up with her own doctor in two days, or to return to the emergency department if worse. James Gostigian Sample Date of Visit: 08/31/2003 CHIEF COMPLAINT: Rash. HISTORY OF PRESENT ILLNESS: The patient is a 59-year-old male presenting to the emergency department with a rash. He states that he has had an itching rash on his forearms and hands since approximately Tuesday. He states that the rash appeared after he came in contact with a pepper plant. The patient did go to a clinic and received an intramuscular injection of Cortisone. He has been taking Clarinex pills. He does not report any relief. There is no difficulty breathing, throat closing sensation, abdominal pain or nausea. No fever, sweats or chills. REVIEW OF SYSTEMS: All systems reviewed and are negative except for the items as mentioned above. PAST MEDICAL HISTORY: Cerebrovascular accident, depression, hypercholesterolemia, left knee surgery. SOCIAL HISTORY: He does not smoke or drink alcohol. ALLERGIES: MULTIPLE, and as noted per chart. MEDICATIONS: PHYSICAL EXAMINATION: VITAL SIGNS: Reviewed. GENERAL: The patient is awake, alert, responsive and not in any acute distress. HEENT: Head is normocephalic. Eyes pupils equal, round, reactive to light and accommodation. Lips and mucous membranes moist. NECK: Tender. CHEST: Normal chest excursions. HEART: S1, S2 regular. LUNGS: Clear. ABDOMEN: Soft, nontender. SKIN: The patient has a macular/papular scaly type rash present on the forearms, wrists and hands. INTERVENTION: Medications - prednisone 40 mg p.o. was given, after which his condition was unchanged. DIAGNOSIS: Contact dermatitis. DISPOSITION: Discharged home. PRESCRIBED MEDICATIONS: Medrol Dosepak. Anthony Dalley Sample Date of Visit: 09/02/2003 CHIEF COMPLAINT: Numbness. HISTORY OF PRESENT ILLNESS: The patient is a 45-year-old gentleman who states for the past couple of days he has had numbness of the left side of his face. He has also had some numbness in the fingers of both hands and the supervisor at the Rescue Mission brought him to the emergency department for evaluation. He denied having any headache or any visual symptoms. He denies any near-syncope, no neck pain, no chest pain or shortness of breath, no abdominal pain, no vomiting, no hematemesis, no rectal bleeding, no urinary symptoms, no incontinence, no back pain and no other complaints. REVIEW OF SYSTEMS: As noted above. All other systems are reviewed and are negative. PAST MEDICAL HISTORY: No history of hypertension or diabetes. SOCIAL AND FAMILY HISTORY: The patient is a truck driver. He is staying at the Rescue Mission. He does not smoke or drink alcohol. PHYSICAL EXAMINATION: GENERAL: The patient is alert and oriented. VITAL SIGNS: He is afebrile. Blood pressure initially was 144/104. SKIN: Warm and dry. HEENT: Normal. Eyes are normal. Throat is clear. NECK: Supple, no neck stiffness or tenderness. LUNGS: Clear bilaterally. HEART: Normal sinus rhythm. ABDOMEN: Soft, nontender. There is no rebound and no guarding. NEUROLOGIC: Examination of the cranial nerves revealed decreased sensation to the maxillary division of the 5th cranial nerve. There is no facial paralysis noted. Motor is intact. Reflexes symmetrical. Electrocardiogram showed a normal sinus rhythm with a rate of 67 per minute, PR interval is normal, axis is normal, no acute ST/T changes. A CT scan of the head is done and showed evidence of cerebellar tonsillar herniation. The radiologist reviewed the films and called this adult Chiari malformation. The patient was presented to neurologist on call, Dr. Eileen Schwartz. She indicated she would see the patient in the office for follow-up and she also advised consultation with neurosurgery. The patient was presented to the neurosurgeon on call, Dr. Tipton, and he advised that the patient be discharged home to follow-up in the office. Dr. Tipton will see the patient and obtain MRI and other tests as needed. DIAGNOSES: 1. Numbness. 2. Adult Chiari malformation. DISPOSITION: The patient agrees to follow-up as directed. He will contact Dr. Tipton first thing in the morning for further instructions and follow-up, return if worse. Anthony Dalley Sample Date of Visit: 09/02/2003 CHIEF COMPLAINT: Vomiting and diarrhea. HISTORY OF PRESENT ILLNESS: The patient is a 91-year-old female who presents with vomiting and diarrhea, which began early this evening. She lives alone and the manager of the mobile park went to visit her and found the patient appeared to be quite weak and called EMS and had her transported to the emergency department. On arrival she complained of diffuse abdominal pain. There is no report of any hematemesis or any rectal bleeding. She denied any fever or chills, no headache and neck pain, no chest pain, no shortness of breath, cough or hemoptysis and no other complaints. REVIEW OF SYSTEMS: As noted above. All other systems are reviewed and are negative. PAST MEDICAL HISTORY: The patient has a history of hypertension. PAST SURGICAL HISTORY: She has had appendectomy and hysterectomy. She has also had bilateral corneal transplants. SOCIAL AND FAMILY HISTORY: The patient is twice widowed; no children. She lives alone in the mobile park. She does not smoke or drink alcohol. PHYSICAL EXAMINATION: GENERAL: The patient is alert and oriented. VITAL SIGNS: She is afebrile. Blood pressure 192/91. SKIN: Warm and dry, no petechiae or ecchymosis. HEENT: Normal. Mucous membranes are pink and sclerae anicteric. NECK: Supple and nontender, no jugular venous distention or thyromegaly or adenopathy. LUNGS: Clear bilaterally; no rales or rhonchi. HEART: Normal sinus rhythm. ABDOMEN: Soft with mild diffuse tenderness, no rebound and no guarding. Bowel sounds are present. There is some tympany on percussion. EXTREMITIES: There is no calf swelling or tenderness, no evidence of deep venous thrombosis. NEUROLOGIC: Grossly intact. X-RAYS: Abdominal series showed non-specific gas pattern with large air/fluid level in the upper abdomen. Radiology report is pending. Electrocardiogram showed a normal sinus rhythm with a rate of 79 per minute. There is left axis deviation. PR interval is normal, no acute ST/T changes are identified. LABORATORY: CBC showed mild leukocytosis. Hemoglobin is 14.8, hematocrit 45.0 and white blood cell count 13.1. Electrolytes are all normal. BUN is 20, creatinine is 0.8 and glucose 144. Liver function test are normal. CPK is 43 and troponin negative at less than 0.3. EMERGENCY DEPARTMENT COURSE: The patient was given intravenous fluids, normal saline at 75 cc/hr and she also received intravenous Phenergan. DIAGNOSIS: Abdominal pain, abdominal tenderness and gastroenteritis. DISPOSITION: The patient presented to Dr. Lalla, who kindly agreed to admit the patient for further evaluation and management. Glen Fortier Sample Date of Visit: 08/30/2003 CHIEF COMPLAINT: Dizziness. HISTORY OF PRESENT ILLNESS: The patient is a 39-year-old female who comes in complaining of dizziness. Dr. Klingerman, her PMD, came in to see the patient and he asked if we could take a look at some labs and make sure she was not anemic since she has been having blood in her urine. Apparently she had stood up and felt dizzy, so she came in. The laboratories sent were a CBC, which was entirely normal, and she had a chemistry profile, which was entirely normal. Her prothrombin time and her PTT were normal. She does have some continued problems with back pain. She does have a transitional cell carcinoma of her kidney, which is causing bleeding. Dr. Klingerman felt she was probably having renal colic secondary to a clot. We will give her Dilaudid 3 mg and Vistaril 50 mg IM and discharge her. DIAGNOSES: 1. Dizziness. 2. Renal colic. 3. Renal cancer. PLAN: Follow-up as scheduled with Dr. Klingerman. Glen Fortier Sample Date of Visit: 09/18/2003 CHIEF COMPLAINT: The patient is a 1-month-old female with the chief complaint of drainage from the right eye. HISTORY OF PRESENT ILLNESS: This 1-month-old female has had drainage from her right eye since birth. They had seen their PMD for a two-week follow-up and advised lacrimal massage. Unfortunately, the mother whenever she tries to do this, the baby cries, so she does not do it. Today there is greenish drainage, which has matted the eye shut. There have been no fevers, no other infections. PAST MEDICAL HISTORY: No significant perinatal problems. REVIEW OF SYSTEMS: As noted in the History of Present Illness; all other systems are reviewed and negative. PHYSICAL EXAMINATION: GENERAL: Examination reveals an alert 1-month-old Hispanic female in no distress. VITAL SIGNS: Temperature 98.1, pulse 206 and the patient is crying when I examine her. HEENT: Head: Fontanelle flat. Eyes: There is greenish discharge, right eye. There is no conjunctival injection noted. The pupils equal, round and reactive to light.. Ears, nose, throat: No nasal discharge and no pharyngeal injection noted. Tympanic membranes are not injected. NECK: Supple. EMERGENCY DEPARTMENT COURSE: We showed the mother how to use cotton balls again, warm water, to clean the discharge off. We showed her how to do lacrimal massage and advised she needs to keep doing it even if the baby is crying and we put gentamicin drops, 2 in the right eye. DIAGNOSIS: Dacryocystitis. PLAN: We advised the mother to do as we have done above every three hours and follow-up with her PMD. Richard Macchiaroli Sample Date of Visit: 07/11/2003 CHIEF COMPLAINT: Cough. HISTORY OF PRESENT ILLNESS: The patient is a pleasant 37-year-old female who reports that she has had approximately three weeks of cough, which is non-productive in quality, moderate in severity, worse at night. She denies any shortness of breath, but she says the cough wakes her up at night. She has had no hemoptysis. She has had no night sweats; she has no fevers or chills. She also reports that she had some low back pain two days ago in the left low lumbar area, but that dissipated within a couple of hours two days ago. She reports that she does have a mild amount of post-tussive emesis. She does have some nausea and she has had some dysuria recently. She has no chest pain. She has no headache, numbness or weakness. Her last menstrual period was 06/17. PAST MEDICAL HISTORY: She denies. PAST SURGICAL HISTORY: Ectopic pregnancy. SOCIAL HISTORY: She does smokes. She drinks occasional alcohol and she does not use recreational drugs. MEDICATIONS: Robitussin. FAMILY HISTORY: There is no asthma in the family. REVIEW OF SYSTEMS: All systems were reviewed and negative except as in the history of present illness. PHYSICAL EXAMINATION: GENERAL: She is well developed, well nourished in no acute distress. VITAL SIGNS: Temperature 98.8, pulse of 87, respirations of 20, blood pressure of 115/77, pulse oximetry 99% on room air. SKIN: Warm and dry distally with less than 2 second capillary refill. HEENT: Eyes: Pupils equal, round and reactive to light. Extraocular movements intact. Head is normocephalic, atraumatic. Oropharynx clear and moist. NECK: Supple. LUNGS: Clear to auscultation bilaterally with wheezes, rhonchi or rales, however, there is a mild prolonged expiratory phase. CARDIOVASCULAR: Regular rate and rhythm with no murmurs, gallops or rubs. ABDOMEN: Soft, nontender, non-distended with normoactive bowel sounds and no guarding, rebound or rigidity. MUSCULOSKELETAL EXAM: Normal gait, full range of motion of all extremities. NEUROLOGIC: The patient is alert and oriented x 3 and has distal strength and sensation intact in all four extremities. PSYCHIATRIC: She has normal mood and affect. HEMATOLOGIC: The patient has no ecchymosis or petechiae. MEDICAL DECISION-MAKING: The differential diagnosis includes bronchitis, pneumonia, pneumothorax, asthma, bronchospasm, urinary tract infection. EMERGENCY DEPARTMENT COURSE: The patient was stable throughout her emergency department course. She had an albuterol treatment, which made her feel substantially better and got rid of her coughing. She had a chest x-ray and urinalysis with results as below. She was discharged to home in stable condition. Her diagnostic studies in the emergency department included a pulse oximetry of 99% on room air, which is normal per emergency department physician interpretation; chest x-ray with no acute changes per emergency department physician interpretation; urinalysis, which was normal. Re-evaluation of the patient revealed her to be much more comfortable. I did treat her for the possibility of a mycoplasma pneumonia with the non-productive cough that she had had for approximately three weeks as well as for the possibility of some nighttime bronchospasm. DISPOSITION: To home in stable in stable condition. DIAGNOSES: 1. Acute cough. 2. Possible bronchospasm. INSTRUCTIONS: Take Zithromax for possible infection, albuterol inhaler two puffs q 4h as needed for cough, Hycodan syrup for cough and follow-up with Dr. Haines next week for a recheck. Richard Macchiaroli Sample Date of Visit: 09/12/2003 CHIEF COMPLAINT: Motor vehicle crash. HISTORY OF PRESENT ILLNESS: The patient is a pleasant 22-year-old female who reports she was the restrained driver in a motor vehicle crash that occurred one hour ago in duration. She complains of neck pain and high thoracic back pain, which is moderate in severity, gradually increasing. The patient reports she has a mild posterior occipital headache which started after the accident. She has no numbness or weakness to me. She denies any abdominal pain or chest pain. She denies any loss of consciousness. She denies fevers, chills, nausea, vomiting or diarrhea. She denies visual changes. Her symptoms are mild in severity, constant in timing. PAST MEDICAL HISTORY: Negative. PAST SURGICAL HISTORY: Negative. SOCIAL HISTORY: She does not smoke, drink alcohol or use recreational drugs. MEDICATIONS: None. ALLERGIES: None. REVIEW OF SYSTEMS: All systems were reviewed and negative except as in the history of present illness. PHYSICAL EXAMINATION: GENERAL: The patient is well developed, well nourished in no acute distress. VITAL SIGNS: Stable. Pulse oximetry 97% on room air. SKIN: Warm and dry distally with less than 2 second capillary refill. HEENT: Eyes: Pupils equal, round and reactive to light. Extraocular movements intact. Head is normocephalic, atraumatic. Oropharynx clear and moist. NECK: Supple. LUNGS: Clear to auscultation bilaterally, no wheezes, rhonchi or rales. CARDIOVASCULAR: Regular rate and rhythm with no murmurs, gallops or rubs. ABDOMEN: Soft, nontender, non-distended with normoactive bowel sounds and no guarding, rebound or rigidity. MUSCULOSKELETAL EXAM: Normal gait, full range of motion of all extremities. She does have some mild lateral neck pain. She has no midline cervical, thoracic or lumbar tenderness. NEUROLOGIC: The patient is alert and oriented x 3 and has distal strength and sensation intact in all four extremities. PSYCHIATRIC: She has normal mood and affect. HEMATOLOGIC: The patient has no ecchymosis, petechiae or lymphadenopathy. MEDICAL DECISION-MAKING: The differential diagnosis includes cervical strain, cervical fracture, thoracic strain, thoracic fracture, epidural hematoma, subdural hematoma. EMERGENCY DEPARTMENT COURSE: The patient was stable throughout the emergency department course and had no major abnormalities on examination. She had a CT of the head and C-spine, which were normal per emergency department physician interpretation. She was discharged home in stable condition. Her diagnostic studies in the emergency department - C-spine, which was normal per emergency department physician interpretation, CT of the head, which was normal per emergency department physician interpretation. DIAGNOSES: 1. 2. Cervical strain. Closed head injury. DISPOSITION: To home in stable condition. INSTRUCTIONS: Follow head injury instructions as given; follow-up with primary doctor; take Motrin and Flexeril for pain. Roy Wood Sample Date of Visit: 07/13/2003 PHYSICIAN TIME: 0615 CHIEF COMPLAINT: This is a 26-year-old female with the chief complaint of nausea, vomiting, diarrhea and abdominal pain. HISTORY OF PRESENT ILLNESS: The patient states that for about 24 hours the patient has been having some significant amount of abdominal pain with nausea and vomiting. She denies any fever, but she has had some chills. She has had no dysuria, frequency, urgency, and she denied any vaginal discharge. REVIEW OF SYSTEMS: All other systems reviewed and negative. PAST MEDICAL HISTORY: Anemia. PAST SURGICAL HISTORY: None. MEDICATIONS: None. ALLERGIES: None. SOCIAL HISTORY: She is a half pack to a pack a day cigarette smoker, and occasional alcohol drinker and she denies recreational drugs. PHYSICAL EXAMINATION: GENERAL: This is a well developed female in obvious distress secondary to her complaint. VITAL SIGNS: Temperature Afebrile, pulse 116 and regular, respirations 24 and unlabored and blood pressure was 161/100, saturation 100% on room air. HEENT: Eyes are pupils equal, round and reactive to light. Oral: Clear. Posterior pharynx is normal. NECK: Supple LUNGS: Clear. HEART: Regular rate and rhythm without murmur, rub or gallop. ABDOMEN: Soft. Increased bowel sounds in four quadrants with no organomegaly, mass and no bruit. She has some suprapubic tenderness without rebound or guarding. There is no organomegaly, no mass and no bruit. EXTREMITIES: No cyanosis or clubbing, no obvious edema. 2+ radials and 2+ dorsalis pedis. NEUROLOGIC: She is alert to person, place, time and following commands, answering questions appropriately and not slurring her speech and does not appear to be intoxicated. ASSESSMENT AND PLAN: Acute abdominal pain with nausea and vomiting and diarrhea. PLAN: Abdominal pain workup including normal saline, 250 cc an hour, Demerol 25 mg intravenously and Phenergan 25 mg intravenously. She got good relief from her pain. Her amylase and lipase came back in the normal range. AST and ALT came back in the normal range as well as her coagulation studies were normal; her BMP was normal. Her white blood cell count was elevated at 20 and her hemoglobin and hematocrit were decreased from normal at 10 and 34. Her urine showed a trace of white blood cells and moderate leukocyte esterase but no nitrite and this was a clean-catch. It shows 11-15 white blood cells and 3-5 red blood cells and moderate leukocyte esterase. In light of her continued pain, she was sent over for a CT scan of her abdomen and pelvis, which was read by the radiologist as normal. She received Pepcid 20 mg intravenously, a GI cocktail and Demerol 25 mg intravenously, and Phenergan 12.5 mg intravenously. She got good relief from her pain and she was discharged with: FINAL DIAGNOSES: 1. Acute abdominal pain. 2. Nausea. 3. Vomiting. DISCHARGE INSTRUCTIONS: Phenergan 25 mg suppositories, one per rectum q6h nausea and vomiting, #12, Bentyl 25 mg p.o. q6h abdominal pain, #20, Zantac 150 b.i.d., #60 with no refills. Follow-up with private MD; return if worse. Roy Wood Sample Date of Visit: 07/28/2003 PHYSICIAN TIME: 1845 CHIEF COMPLAINT: This is a 39-year-old female with chief complaint of acute alcohol intoxication according to her friends. HISTORY OF PRESENT ILLNESS: The patient with altered mental status today with known alcohol binge. She has apparently been in Indiana with alcohol rehabilitation and has not been drinking, but apparently she drank today. She has been uncooperative in triage, but continues to refuse to answer questions and is significantly intoxicated. REVIEW OF SYSTEMS: All other systems reviewed with the patient's friends and are negative. The patient is unable to review systems secondary to her acute alcohol intoxication. PAST MEDICAL HISTORY: Hypertension, alcohol abuse. PAST SURGICAL HISTORY: Tubal pregnancy. MEDICATIONS: Prozac, Inderal. ALLERGIES: No known drug allergies. SOCIAL HISTORY: The patient smokes a half pack of cigarettes a day. PHYSICAL EXAMINATION: GENERAL: The patient is a well developed female in obvious distress secondary to her complaint. VITAL SIGNS: Temperature afebrile 98.1, pulse 111 and regular, respirations 20 unlabored, blood pressure 121/83. Saturation 98% on room air. HEENT: Normocephalic with obvious head trauma. Pupils equal, round, reactive to light and accommodation. Oral is clear. Posterior pharynx is normal. NECK: Supple. No jugular venous distension, carotid bruits, mass, or lymphadenopathy. LUNGS: Clear to auscultation bilaterally. HEART: Regular rate and rhythm without murmur, rub or gallop. ABDOMEN: Soft without pulsatile mass or bruit. No organomegaly. The abdomen is distension, with normal bowel sounds in four quadrants. EXTREMITIES: No cyanosis or clubbing. No obvious edema, 2+ radials and 2+ dorsalis pedis. NEUROLOGIC: Alert, oriented to person, place and time. The patient is unable to answer questions due to her acute alcohol intoxication. The patient is slurring her speech, acute alcohol intoxication. PLAN: PT/PTT, amylase and lipase, ETOH, CMP, CBC. ETOH was 513. PT/PTT normal. BMP normal sugar. Bicarb was slightly decreased at 20. White count normal. Hemoglobin, hematocrit, platelet count normal. The patient received normal saline one liter bolus. Her alcohol came back at 513, therefore requiring admission. I discussed the case with Dr. Ganatra who was next medical backup and he gave orders for admission. FINAL DIAGNOSIS: Acute alcohol intoxication. Peter Patton Sample Date of Visit: 07/25/2003 CHIEF COMPLAINT: Chest pain. HISTORY OF PRESENT ILLNESS: The patient presents for evaluation of an episode of chest pain, which she had at work approximately an hour prior to arrival. The patient also states two episodes yesterday. The pain is described as a pressure. She has no other associated symptoms. The patient is currently pain-free. She works in Convenient Care. An electrocardiogram was done while she was pain-free, which she presents with. The patient otherwise has no other complaints or symptoms. She denies current headache, fever, chills, sweats, neck pain, chest pain, shortness of breath, abdominal pain, nausea, vomiting, diarrhea, constipation, urological disorder or neurological complaint. PAST MEDICAL HISTORY: As noted on chart. SOCIAL HISTORY: The patient smokes, occasionally drinks. She denies drug use. FAMILY HISTORY: Benign. ALLERGIES: As noted on chart. MEDICATIONS: As noted on medication list. REVIEW OF SYSTEMS: Otherwise negative except for the positive findings as stated above. PHYSICAL EXAMINATION: PATIENT STATUS: She is awake, alert and cooperative, in no distress and well hydrated. VITAL SIGNS: Are noted. The patient is noted to be obese. The patient is slightly hypertensive and has a history of hypertension. HEENT: Normal. NECK: Supple without tenderness, decreased range of motion, meningeal signs, jugular venous distention, lymphadenopathy or bruits. CHEST: Without tenderness to palpation, retraction, or accessory muscle use. LUNGS: Breath sounds are equal bilaterally without rales, rhonchi or wheezes. HEART: Rate normal, rhythm regular, without ectopy or murmurs. ABDOMEN: Soft, without tenderness, guarding or rebound. Bowel sounds are normal. No organomegaly or masses. NEUROLOGICAL: Cranial nerves II-XII are intact. Motor, sensory, cerebellar and reflexes are normal. SKIN: No rashes or lesions. EMERGENCY DEPARTMENT COURSE: The patient with a stable emergency department course. The patient underwent the noted workup in the emergency department. All data was subsequently reviewed and interpreted by myself. Electrocardiogram from Convenient Care shows a normal sinus mechanism at 87, without ectopy or ischemia. CBC reveals a 14.5 white blood cell count, otherwise normal hemoglobin, hematocrit and platelets. BMP, cardiac enzymes, troponin, PT, PTT, chest x-ray were normal. The pulse oximetry was 98% on room air. Rhythm strip demonstrates normal sinus mechanism at 80, without ectopy. The patient was medicated with an aspirin. She remained pain-free. Dr. Gomeringer, on call for her primary care physician, who is out of town, was subsequently consulted. She will return on Monday. An outpatient stress test will be scheduled for the beginning of the week. The patient will be given a prescription for sublingual nitroglycerin. She was instructed to take one pill every 5 minutes up to a total of 3 for chest pain. She was also instructed to return to the emergency department for any additional chest pain between now and her stress test. The patient is reliable, and will be discharged to outpatient follow-up. DIAGNOSIS: Chest pain. PLAN: The patient was discharged in stable and improved condition to herself. She was instructed on the diagnosis, care, reasons for emergent return and follow-up. Peter Patton Sample Date of Visit: 09/05/2003 CHIEF COMPLAINT: Fell from bed. HISTORY OF PRESENT ILLNESS: The patient presents for evaluation approximately one hour after falling off a bed, hitting a solid floor. The patient has a right forehead swelling. There was no loss of consciousness and the patient apparently has been acting normally. The mother felt it was prudent for emergency room evaluation. The mother otherwise has no other complaints or symptoms and denies chills, sweats, neck pain, chest pain, shortness of breath, abdominal pain, nausea, vomiting, diarrhea or constipation, urological disorder or neurological complaint. PAST MEDICAL HISTORY: As noted on chart. SOCIAL HISTORY: Benign. FAMILY HISTORY: Benign. ALLERGIES: No known drug allergies. CURRENT MEDICATIONS: Noted on medication list. REVIEW OF SYSTEMS: Negative, except the positive findings stated above. PHYSICAL EXAMINATION: PATIENT STATUS: She is awake, alert, cooperative, in no distress, and well-hydrated. VITAL SIGNS: As noted. HEENT: The patient has a small 2-cm in diameter contusion on the right aspect of the forehead. NECK: Supple, without tenderness, decreased range of motion, meningeal signs, jugular venous distention, lymphadenopathy or bruits. CHEST: Without tenderness to palpation, retraction or accessory muscle use. LUNGS: Breath sounds equal bilaterally, without rales, rhonchi or wheezes. HEART: Rate normal, rhythm regular, without ectopy or murmur. ABDOMEN: Soft, without tenderness, guarding or rebound, bowel sounds are normal, there are no palpable masses. NEUROLOGICAL: Cranial nerves II/XII are intact, motor, sensory, cerebellar and reflexes are normal. SKIN: Normal, without rashes or lesions. EXTREMITIES: The patient has normal range of motion of all extremities, distal extremities are neurovascularly intact. EMERGENCY DEPARTMENT COURSE: The patient was stable in the emergency room course. The patient underwent the noted physical examination. CT scan of the head was ordered. The mother subsequently states she does not feel the child needs a CT scan at this time and will be discharged to outpatient follow up. She states the patient is acting normally. The mother subsequently signs out against medical advice after informed consent. FINAL DIAGNOSES: 1. Forehead contusion. 2. Closed head injury. 3. Status post fall. PLAN: The patient was discharged in stable condition to his mother and grandmother. All were instructed on the diagnosis, care and reasons for emergent return and follow up. Karen Calkins Sample Date of Visit: 07/31/2003 CHIEF COMPLAINT: Nosebleed. HISTORY OF PRESENT ILLNESS: The patient is a 71-year-old white male with history only of high cholesterol. About a week ago he went to see his regular physician for routine physical and he was started on an aspirin a day. He picked up the adult strength aspirin and he has been taking one a day and then on Tuesday of this week started with nosebleeds. They have been intermittent since then and this morning it was more prolonged, although did seem to slow down with some pressure, otherwise he has never had problems with nosebleeds in the past. No other spontaneous bleeding, no fevers. PAST MEDICAL HISTORY: Significant for hypercholesterolemia. PAST SURGICAL HISTORY: Significant for tonsillectomy. MEDICATIONS: Aspirin x 1 week, Pravachol. ALLERGIES: He has no known drug allergies. SOCIAL HISTORY: He stopped smoking about a week ago. He drinks socially. He denies any drugs. He is retired and lives at home with his wife. REVIEW OF SYSTEMS: CONSTITUTIONAL: There is no fever, chills or weight loss. EYES, EARS, NOSE AND THROAT: He is complaining of this intermittent nosebleed from the right naris since Tuesday. Unable to get it stopped fully today. CARDIOVASCULAR: No chest pain or palpitations. RESPIRATORY: There is no shortness of breath or cough. GASTROINTESTINAL: There is no abdominal pain, nausea, vomiting or diarrhea. GENITOURINARY: There is no dysuria, hematuria or frequency, no discharge. MUSCULOSKELETAL: There is no swelling, deformity or pain. SKIN: There is no rash, abrasions or ecchymoses. NEUROLOGICAL: There is no loss of consciousness, headache, focal weakness or paresthesia. PSYCHIATRIC: There are no suicidal or homicidal ideations, no known ingestions. PHYSICAL EXAMINATION: GENERAL APPEARANCE: The patient is sitting up, awake, and alert. He has a tissue in the right naris, but he is in no distress. VITAL SIGNS: Temperature 97.9, pulse 86 and regular, respiratory rate 18, blood pressure initially at triage was 192/103; repeated was 176/80, room air saturation is 96%, he weights 163 pounds. EYES, EARS, NOSE AND THROAT: Examination of the left naris reveals that it is clear and there is no bleeding; the right reveals some oozing from the posterior aspect. Pupils are equal and reactive to light, extraocular muscles are intact. Ears reveal no erythema or discharge. Throat reveals no erythema, edema or exudate. NECK: The neck is supple, trachea is midline. There is no jugular venous distension or lymphadenopathy. CARDIOVASCULAR: S1, S2, regular rate and rhythm, no murmurs, rubs or gallops. RESPIRATORY: Clear breath sounds bilaterally, no wheezing, rales or rhonchi. Chest wall is nontender. GASTROINTESTINAL: Positive bowel sounds, soft, nontender, nondistended. There is no rebound or guarding, no palpable masses or organomegaly. GENITOURINARY: Normal external genitalia, no hernias, no discharge. NEUROLOGICAL: The patient is alert and oriented X3, cranial nerves II-XII are intact, 5/5 strength throughout, intact sensation, symmetrical reflexes. SKIN: Warm and dry, no lesions, rash, lacerations or ecchymosis. In the emergency department, the area was anesthetized with a mixture of lidocaine and Neo-Synephrine with cotton; after this there was still a little bit of oozing from posterior. Merocel packing was applied. In the emergency department, he had labs with a white blood cell count of 8.7, hemoglobin of 16.2, platelets 245. He had normal PT/PTT and no active bleeding through the packing here. PLAN: Discharge. Keflex while the packing is in place. Normal saline nasal spray. Have the packing removed in two days. Hold the aspirin until Monday and then restart the 81 mg a day aspirin. He is to follow-up with Dr. Stevens Monday, who is on for ENT and return for any problems. FINAL DIAGNOSES: Epistaxis. Karen Calkins Sample Date of Visit: 09/05/2003 CHIEF COMPLAINT: Light-headed. HISTORY OF PRESENT ILLNESS: The patient is a 26-year-old white male with history of reactive airway disease and what sounds like ulcer disease in the past. He comes in saying that he felt light-headed. He said he works outside doing heavy work and worked all day in the heat yesterday. He felt a little bit light-headed last night and got up this morning and actually went to work. He was again working outside, strenuously and he said he felt very light-headed, as if he might pass out. He says dizzy, although it does not sound vertiginous at all. He said he is a little bit nauseous with this. He says this has happened to him before in the past when he gets dehydrated from working out in the sun. There is no headache, no vision problems, no neck pain and no chest pain, no focal weakness or numbness. There is no difficulty with gait or speech and no recent illnesses at all. REVIEW OF SYSTEMS: CONSTITUTIONAL: There is no fever, chills or weight loss. EYES, EARS, NOSE AND THROAT: There is no blurred or double vision, no nasal discharge, no difficulty with swallowing. CARDIOVASCULAR: There is no chest pain or palpitations. RESPIRATORY: There is no shortness of breath or cough. GASTROINTESTINAL: There is no abdominal pain, nausea, vomiting or diarrhea. GENITOURINARY: There is no dysuria, hematuria or frequency, no discharge. MUSCULOSKELETAL: There is no swelling, deformity or pain. SKIN: There is no rash, abrasions or ecchymoses. NEUROLOGICAL: He is complaining of feeling a little bit light-headed with trying to work this morning. There is no headache, no blurred vision and no neck pain, no focal weakness or numbness. PSYCHIATRIC: There are no suicidal or homicidal ideations, no known ingestions. PAST MEDICAL HISTORY: Asthma and ulcer disease. PAST SURGICAL HISTORY: Negative. ALLERGIES: Aspirin and iodine. CURRENT MEDICATIONS: No medications at all. SOCIAL HISTORY: He smokes a pack a day and drinks socially. He denies any drugs. PHYSICAL EXAMINATION: GENERAL APPEARANCE: Sitting up awake, alert and in no distress. VITAL SIGNS: Temperature 98.1, pulse 75 and regular, respiration rate 16, blood pressure 130/75, room air SAT is 98% and his weight is 206 pounds. EYES, EARS, NOSE AND THROAT: Pupils are equal and reactive to light, extraocular muscles are intact. Ears reveal no erythema or discharge. Throat reveals no erythema, edema or exudate. NECK: The neck is supple, trachea is midline. There is no jugular venous distension or lymphadenopathy. CARDIOVASCULAR: S1, S2, regular rate and rhythm, no murmurs, rubs or gallops. RESPIRATORY: Clear breath sounds bilaterally, no wheezing, rales or rhonchi. Chest wall is nontender. GASTROINTESTINAL: Positive bowel sounds, soft, nontender, nondistended. There is no rebound or guarding, no palpable masses or organomegaly. GENITOURINARY: Normal external genitalia, no hernias, and no discharge. NEUROLOGICAL: The patient is alert and oriented X3, cranial nerves II-XII are intact, 5/5 strength throughout, intact sensation, symmetrical reflexes. SKIN: Warm and dry, no lesions, rash, lacerations or ecchymosis. ADDENDUM/3385464/G63 EMERGENCY DEPARTMENT COURSE: He had labs with a white count of 6.4, hemoglobin 14.3 and platelets 197. Chem 7 was normal. He received a total of a liter of normal saline and he says he feels 100% better. He got up and ambulated with no problems at all and remained neurologically intact. PLAN: Discharge, rest, plenty of fluids and follow up with next medical backup. He can return for any problems. FINAL DIAGNOSES: 1. Light-headedness. 2. Mild dehydration. Jennifer Springer Sample Date of Visit: 08/13/2003 HISTORY OF PRESENT ILLNESS: The patient is an 85-year-old female who presents to the Emergency Department at 4:40 p.m. complaining of left hand tingling and her mouth and tongue being numb while she was eating today, approximately an hour prior to arrival. She states that over that hour the symptoms resolved and she does not have any residual symptomatology at this point. She does have a history of bilateral carpal tunnel syndrome, but states that this was not the same and the numb feeling came all the down from the entire arm. She denies any weakness at that time; denies chest pain, shortness of breath, headache, visual changes, rash, swelling, syncope or any other complaints. REVIEW OF SYSTEMS: All other review of systems were reviewed and were negative. She has had no stroke history or workup for the same. ALLERGIES: None known. SOCIAL HISTORY: She denies smoking or recreational drug use. She does admit to rare alcohol use. PHYSICAL EXAMINATION: VITAL SIGNS: Temperature 98.5, pulse 104, respiratory rate 16, blood pressure 186/83, room air saturation 99%. GENERAL: The patient is awake and alert and in no acute distress. HEENT: Normocephalic, atraumatic. Sclerae are atraumatic. Conjunctivae pink. Mucous membranes are moist. Pharynx is clear. NECK: Supple, no jugular venous distention, bruits or adenopathy. NEUROLOGIC: Cranial nerves II-XII are intact. LUNGS: Clear. HEART: Regular rate, no gallops, murmurs or rubs are heard. ABDOMEN: Soft, non-tender, non-distended. Positive bowel sounds, no masses are palpated. SKIN: Warm and dry without rash. No clubbing, cyanosis or edema. EXTREMITIES: Calves are non-tender without cords. EMERGENCY DEPARTMENT COURSE: A stroke profile was ordered. Electrocardiogram returned while I was still in care of the patient with a sinus rhythm at 80 with a left bundle branch block. There is no old record to compare an old electrocardiogram with this at this time. At this point all labs and CT of the head are pending and the case is signed out to Dr. Burkey at 6 p.m. pending these laboratory results and disposition. DIAGNOSIS: Transient ischemic attack. Jennifer Springer Sample Date of Visit: 08/13/2003 HISTORY OF PRESENT ILLNESS: The patient is a 6-week-old female, normal vaginal delivery at full term. She was born here; discharged from here, told to follow-up with Lehigh Acres Family Health Center but mom states she lost the phone number and has not had this follow-up. She brings the child in to the Emergency Department for a checkup and because she says the baby will not stop crying. They are also concerned because the baby's soft spot is pulsatile at times and the baby's stool has little white seeds in it. The mom states that she is breast feeding and interchanging with Carnation Good Start formula and she states that the baby normally sleeps a lot and eats a lot, has several wet diapers a day and bowel movements. She denies any blood or black in the baby's stools. She denies her having any vomiting or even spit up; no rash, no fevers and mom has been measuring her temperatures rectally. Apparently on arrival to the Emergency Department and evaluation out in triage, the child was irritable and crying, by nursing report. REVIEW OF SYSTEMS: All other review of systems were reviewed and were negative. PAST MEDICAL HISTORY: Significant for recent full term delivery. ALLERGIES: None. PHYSICAL EXAMINATION: VITAL SIGNS: Temperature is 98.8 rectally, pulse was 199 while crying, and 140 at rest. Respiratory rate 62, room air saturation was 99%. GENERAL: The child is awake and alert, in no acute distress. She follows with eye contact, moves all extremities equally. HEENT: She is normocephalic and atraumatic. Anterior fontanelle is soft and flat. Sclerae are anicteric. Conjunctivae are pink. Mucous membranes are moist. Pharynx is clear. Tm are clear. Nares are patent without any discharge. Sinuses are non-tender without any swelling or erythema. NECK: Non-tender, with full range of motion. There is no anterior cervical adenopathy. LUNGS: Clear bilaterally without retractions. HEART: Regular rate, no gallops, murmurs or rubs are heard. ABDOMEN: Soft, non-tender, non-distended, positive bowel sounds are present. No masses are palpable. GU: Normal external female genitalia without any discharge or rash. The diaper has a brownish-green stool in it with the normal breast feeding seedy appearance, that the parents were worried about. SKIN: Warm and dry without rash. MUSCULOSKELETAL: All joints are non-tender will full range of motion. There is no hair tourniquet seen. The child is actually cooing and smiles at times. She does have periods of crying but is easily consoled by mom rocking her and is easily consoled by Carnation Good Start formula that we gave the mom for the baby to drink. The child is drinking formula with ease without any problems, no vomiting in the Emergency Department. When the child does have crying spells, the abdomen appears without any masses at that time. The symptoms resolve with consolation and without lethargy. The stool was tested for blood and was negative. After further discussion with the parents, mom stated there was one point where she thought she heard a rattle in the back of the child's chest, so a chest x-ray was obtained, which showed no acute disease. Inpatient record for the child was attempted to be retained but was unable to per the Emergency Department unit secretary. I spent much time with both parents educating them on how to care for a child; on the findings of normal seedy stools, as well as the soft spot area. I have also given them the Lehigh Acres Family Health Center number again for them to follow-up with them. I have reiterated how important this is; the child is to have six week immunization that she is due for as we speak. The parents were given strict instructions to follow-up with them by phone today or tomorrow and make an appointment as soon as they can. They were also told to return for any worsening or concerns, especially fever, vomiting, or blood in the stool. DIAGNOSIS: Well child, and colic. Adam Brenner Sample Date of Visit: 07/27/2003 AKA: “Unknown V” CHIEF COMPLAINT: Trauma alert. HISTORY OF PRESENT ILLNESS: This is a roughly 35-year-old male who was drinking, hit a telephone pole when he was driving. The car rolled over. He sustained prolonged extrication and had lots of facial trauma, right-sided. He denies any other complaints except on the scene, some abdominal pain. He does not complain of that here. He denies any neck pain. It is unclear if there was any loss of consciousness. He denies any extremity pains. He is a poor historian; not very cooperative. He reports he can see with his right eye. PAST MEDICAL HISTORY: Denies. PAST SURGICAL HISTORY: Denies. MEDICATIONS: None. MEDICAL ALLERGIES: None. SOCIAL HISTORY: No toxic habits. FAMILY HISTORY: Negative. REVIEW OF SYSTEMS: All systems reviewed and were negative except as detailed above in the History of Present Illness. PHYSICAL EXAMINATION: VITAL SIGNS: Are noted. The patient had a GCS of 15 and there was marked facial tenderness, right periorbital area, maxillary area. He had marked chemosis of the right bulbar conjunctiva, and subconjunctival hematomas of the bulbar conjunctiva. HEENT: Pupils are round, reactive to light at 4 mm bilaterally. He was able to see through his right eye. He was not cooperative with the exam; I could not test his extraocular movements. He had no septal hematoma. The face was otherwise stable. No loose dentition. He did have a tongue ring. He had no hemotympanum. NECK: Nontender to palpation. Trachea was midline. ENDOCRINE: No thyromegaly. LUNGS: Clear to auscultation bilaterally. CHEST WALL: Nontender to palpation. ABDOMEN: Soft, nontender, no organomegaly. GENITOURINARY: No costovertebral angle tenderness. BACK: Nontender to palpation. Per trauma surgeon, pelvis was stable. EXTREMITIES: The bilateral upper and lower extremities had full range of motion throughout. RECTAL EXAM: Per trauma surgeon. GENITALIA: Unremarkable. NEUROLOGIC: Cranial nerves II through XII intact and strength and sensation intact. The patient was sent for a CT of the brain, abdomen and pelvis, facial bones, only with multiple facial bone fractures, right-sided; this was the official radiology report. Plain film of the pelvis, C-spine and chest were unremarkable. LABORATORY RESULTS: Show unremarkable coagulation studies. Chemistry: Essentially unremarkable. Alcohol level 139 and CBC unremarkable. The remainder of disposition and management either per trauma service or oral surgery, if they are consulted. DIAGNOSES: 1. Alcohol intoxication. 2. Concussion. 3. Multiple right facial fractures. 4. Subconjunctival hemorrhage, right-sided. Adam Brenner Sample Date of Visit: 09/18/2003 AKA: “UNKNOWN YL” - TRAUMA ALERT HISTORY OF PRESENT ILLNESS: This is roughly a 30-year-old male who was stabbed to the abdomen. He reported had a low GCS on scene and was brought in awake and alert, complaining of abdominal pain, slashed with a blade, unknown how long. The history is limited due to the urgency of the situation. No shortness of breath, no chest pain otherwise. PAST MEDICAL/SURGICAL HISTORY: Negative as far as I was able to ascertain, but limited due to the urgency of the situation. MEDICATIONS: None known. MEDICAL ALLERGIES: None known. SOCIAL HISTORY: No toxic habits. FAMILY HISTORY: Unable to obtain. REVIEW OF SYSTEMS: All systems unable to be obtained due to the urgency of the situation. PHYSICAL EXAMINATION: VITAL SIGNS: Are noted. GENERAL: The patient was alert and oriented x 3. GCS of 15. NECK: Small superficial laceration to anterior neck, non-penetrating, through the platysma, very superficial. HEENT: Pupils equal, round, reactive to light and accommodation. Oropharynx clear. LUNGS: Clear to auscultation bilaterally. ENDOCRINE: No thyromegaly. CARDIOVASCULAR: Without murmur. ABDOMEN: Tender - left upper quadrant, penetrating wound to the abdomen. It is unclear how deep it is but it is several cm. Wide. There is also an exploratory laparotomy scar previously present; unknown due to what. GENITOURINARY: No significant findings. PSYCHIATRIC: Normal mood, normal affect. NEUROLOGIC: Unremarkable. The patient will be taken emergently to the operating theatre for exploratory laparotomy, as it most likely seems to penetrate, per the trauma surgeon. ADMITTING DIAGNOSIS: Penetrating wound to abdomen. Admitted for exploratory laparotomy. Admitted as per admitting physician.