memory loss, speech problems, fatigue, urinary
advertisement
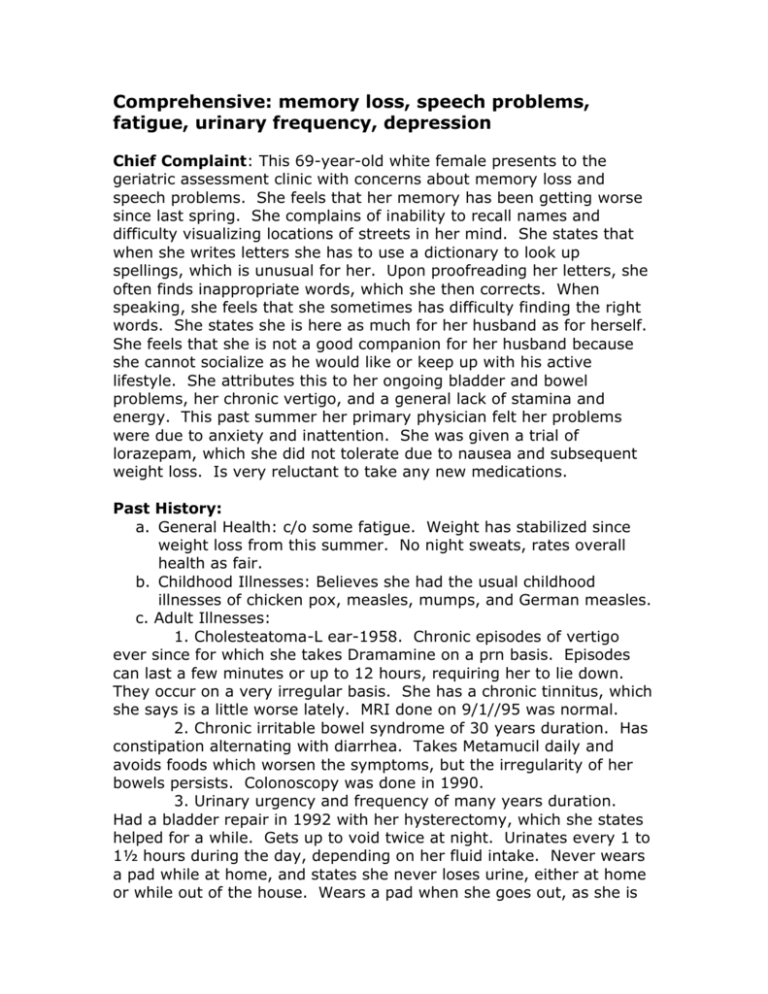
Comprehensive: memory loss, speech problems, fatigue, urinary frequency, depression Chief Complaint: This 69-year-old white female presents to the geriatric assessment clinic with concerns about memory loss and speech problems. She feels that her memory has been getting worse since last spring. She complains of inability to recall names and difficulty visualizing locations of streets in her mind. She states that when she writes letters she has to use a dictionary to look up spellings, which is unusual for her. Upon proofreading her letters, she often finds inappropriate words, which she then corrects. When speaking, she feels that she sometimes has difficulty finding the right words. She states she is here as much for her husband as for herself. She feels that she is not a good companion for her husband because she cannot socialize as he would like or keep up with his active lifestyle. She attributes this to her ongoing bladder and bowel problems, her chronic vertigo, and a general lack of stamina and energy. This past summer her primary physician felt her problems were due to anxiety and inattention. She was given a trial of lorazepam, which she did not tolerate due to nausea and subsequent weight loss. Is very reluctant to take any new medications. Past History: a. General Health: c/o some fatigue. Weight has stabilized since weight loss from this summer. No night sweats, rates overall health as fair. b. Childhood Illnesses: Believes she had the usual childhood illnesses of chicken pox, measles, mumps, and German measles. c. Adult Illnesses: 1. Cholesteatoma-L ear-1958. Chronic episodes of vertigo ever since for which she takes Dramamine on a prn basis. Episodes can last a few minutes or up to 12 hours, requiring her to lie down. They occur on a very irregular basis. She has a chronic tinnitus, which she says is a little worse lately. MRI done on 9/1//95 was normal. 2. Chronic irritable bowel syndrome of 30 years duration. Has constipation alternating with diarrhea. Takes Metamucil daily and avoids foods which worsen the symptoms, but the irregularity of her bowels persists. Colonoscopy was done in 1990. 3. Urinary urgency and frequency of many years duration. Had a bladder repair in 1992 with her hysterectomy, which she states helped for a while. Gets up to void twice at night. Urinates every 1 to 1½ hours during the day, depending on her fluid intake. Never wears a pad while at home, and states she never loses urine, either at home or while out of the house. Wears a pad when she goes out, as she is constantly worried that she will not be able to find a restroom when she needs it. 4. Osteoporis-kyphosis. Has used estrogen patch for a number of years. d. Psychiatric Illnesses: 1. Anxiety? Was hospitalized in 1993 for pain in her chest and right arm. Cardiac work-up was negative. Client attributes symptoms to stress and anxiety. 2. States she dropped out of college when she was young due to stress and depression. e. Operations 1. Hysterectomy and bladder repair, 1992. 2. Cholesteatoma- 1958. Current Health Status: a. Allergies: None. b. Immunizations: Has had flu shot for this year and Pneumovac. Does not recall date of last tetanus shot. c. Environmental hazards: None. d. Use of safety measures: Always wears a seat belt in the car. Lives in a multilevel town home. Has railings on stairs and safety rails in the bathroom. e. Exercise and leisure activities: Does not do much for leisure activities any more. States she participates in church activities when her husband can drive her, and she goes to the beauty parlor each week. Does not exercise regularly. f. Screening tests: Visits dentist regularly. Recently had eye exam. States has hearing loss in L ear from cholesteatoma. Mammogram within past year. Pap smear done 9/29. g. Sleep patterns: Feels she sleeps fairly well – about 7 hours per night. h. Diet: Avoids foods such as fresh fruits, beans, and cabbage, which irritate her bowel. i. Tobacco: Does not smoke. j. Alcohol: Very occasionally. k. Current medications: 1. Metamucil 1 Tbsp. daily 2. Estraderm 0.05 patch 3. Stress tabs vitamins I daily 4. Baby ASA daily 5. Ecotrin I prn for headache 6. Dramamine 50 mg. prn vertigo Family History: Mother died of lung cancer. Father died at 89 of pneumonia. Two sisters – one is 79 with diabetes, other is 75 with osteoporosis and temporal arteritis. Has two daughters in good health. Psychosocial: Married. Retired teacher. States she is fairly content to stay home most of the time, but she realizes she has withdrawn from many of her activities. Husband is very active and would like her to go out more. States she feels tethered to the bathroom because of her bladder and bowel problems, and she also worries about having an attack of vertigo. Neither daughter lives in town. One daughter lives in Italy. Her husband is learning Italian and would like her to take a trip to Italy, but she feels she is not able. Does go to church regularly – religion is Lutheran. Review of Systems: a. Skin: Denies rashes, pruritis, suspicious lesions. b. Head: Normal scalp and skull. Hair - normal texture. c. Eyes: Denies diploplia, blurred vision, pain, redness, or drainage. d. Ears: Hearing loss in L ear. Tinnitus of long-standing duration. No ear pain or drainage. e. Nose and Sinuses: Denies epistaxis, discharge, sinus pain, nasal obstruction. f. Mouth and Throat: Denies sores, hoarseness, bleeding gums, toothache. g. Neck: No stiffness, lumps, swollen glands, pain. h. Breasts: No nipple discharge, lumps, pain, rashes. Does SBE. h. Respiratory: No chest pain, wheezing, shortness of breath, dyspnea on exertion. i. Cardiac: Denies chest pain, palpitations, orthopnea, PND. j. Gastrointestinal: Appetite is decreased. Especially has no desire to eat meat. Denies heartburn. Bowels are irregular and unpredictable, with constipation alternating with diarrhea. k. GU: Has frequency and some urgency. Denies dysuria, hematuria, or flank pain. No vaginal bleeding, no discharge, or itching. l. Musculoskeletal: Denies significant joint pain or stiffness, no swelling, no muscle pain or weakness. m. Peripheral vascular: No pain, numbness, tingling, ulcers, cyanosis, or edema in extremities. Has some varicosities. n. Neurologic: No seizures, tremors, dizziness, loss of consciousness, difficulty swallowing, weakness. o. Hematologic: No bleeding, unusual bruising. Denies blood transfusions. p. Endocrine: No unusual hunger, thirst, increased urination. Denies intolerance to heat and cold. q. Psychiatric: Admits to some anxiety and depression. Physical Exam: Wt. 122# (stable). BP 130/80. General: Pleasant, cooperative female who is oriented x3 and a fairly good historian. Skin: Warm and dry, turgor good, no rashes, no suspicious lesions. Nail beds, pink, good capillary refill. Head: Hair of normal texture. Scalp normal. Eyes: Visual fields full by confrontation. EOMs intact, no nystagmus. Conjunctiva pink, no discharge. PERRLA. Unable to visualize optic disk, but vessels and background appear normal. Ears: No discharge or tenderness to palpation. Minimal cerumen in canals. Tympanic membranes pearly gray. Acuity to whispered voice normal on R, diminished on left. Nose: Mucosa pink. Septum midline. No sinus tenderness. Mouth: Mucosa pink. No lesions or bleeding. Teeth in good repair. Pharynx pink. Tongue symmetric, protrudes midline. Uvula rises midline on phonation. Neck: Neck supple with full ROM. No lymphadenopathy. Trachea midline. Thyroid nonpalpable. No JVD, no carotid bruits. Thorax and Lungs: Expansion symmetric. Lung fields resonant. Vesicular breath sounds throughout. No CVA tenderness. Kyphosis of back. Breasts: Symmetric, no nipple discharge, no masses, no lymphadenopathy. Heart: Regular rate of 72, regular rhythm. S1 S2 normal, no S3 or S4 murmur. Abdomen: Symmetric, soft, nontender, no masses. Bowel sounds present in all quadrants. No hepatosplenomegaly. GU: Pelvic, pap smear, and rectal exam deferred – were done within the past month by primary physician. Extremities: Warm to touch. No calf tenderness. Superficial varicosities on lower extremities. Peripheral pulses strong and equal. Musculoskeletal: Full ROM. No weakness of muscles. Neurologic: Alert and oriented to person, place, and time. Speech appropriate. No difficulty finding or using words. Occasional stuttering or difficulty pronouncing words. Cranial nerves II-XII intact. Cerebellar, finger-to-nose smoothly intact. Sensation intact. Reflexes normal. Negative Babinski. Folstein Mini-Mental – 28/30. Geriatric Depression Scale 13/30.