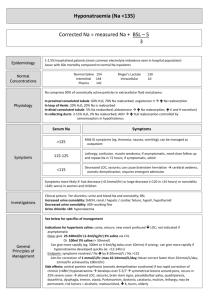
Hyponatraemia
advertisement

Hyponatraemia 29/9/10 My FANZCA notes PY Mindmaps Duggal, A.K et al (2006) “Clinical Approach to Altered Serum Sodium Levels” JIACM 7(2):91103 UptoDate - common problem in ICU (30% of patients have a Na < 134mmol/L) - independent predictor of mortality in ICU - goals = to determine: (1) (2) (3) (4) severity type treat cause prevent complications SEVERITY Na+ < 135mmol/L Mild 125-134 Moderate 120-124 Severe <120 TYPES and CAUSE Hypoosmolar/Hypotonic -> hypovolaemic, euvolaemic and hypervolaemic Isoosmolar Hypertonic Hypotonic/Hypoosmolar - causes = solute depletion or solute dilution Hypovolaemic - loss of H2O and Na from the ECF -> increased ADH secretion -> decreased free H2O excretion and H2O retention -> hyponatraemia - renal or extra-renal causes RENAL LOSS - diuretics osmotic diuresis (glucose, mannitol) bicarbonaturia (RTA) salt wasting nephropathy mineralocorticoids deficiencies ketones Jeremy Fernando (2011) NON-RENAL LOSS - upper GI: vomiting middle GI: pancreatitis, bowel obstruction lower GI: diarrhoea, bowel preparation other losses: sweat, bleeding - the way to sort out whether it is a renal or extra-renal source = to do a urinary Na+ - if urinary Na+ < 10mmoL/L -> extra-renal (as kidney appropriately attempting to hold onto Na+) - if urinary Na+ > 20mmol/L -> renal (as if clinically hypovolaemic then this is an inappropriate response) Euvolaemic - causes = SIADH (most common), psychogenic polydipsia, hypotonic IVF therapy, adrenal insufficiency, hypothyroidism - any disease state causing hypoosmolality can present with a normal state of hydration - clinical examination of volume status is not sensitive - more sensitive = a normal or low urea and an elevated urinary Na+ See SIADH document for further information Causes of SIADH (PAM tHe COD) Pulmonary ADH secretion (ectopic) Malignancy Hormone deficiency CNS disease Others Drugs Hypervolaemic - increase in total body Na+ and H2O -> however, total body H2O is out of proportion to Na+ - clinically evident oedema or ascites - causes: CHF, cirrhosis, nephrotic syndrome, hypothyroidism, pregnancy, TURP/hysteroscopy syndrome Isotonic - known as “pseudohyponatraemia” - plasma osmolality can be measured directly in the laboratory using a osmometer or by the formula: calculated osmolarity = (2xNa+) + glucose + urea - serum is made up of 93% H2O and 7% non-aqueous factors including lipids and proteins - normally the nonaqueous components do not effect the tonicity but in states of marked hyperproteinaemia or hyperlipidaemia (elevated chylomicrons or triglycerides) -> this ratio is changed artifactually decreasing the apparent concentration of Na+ in serum. Jeremy Fernando (2011) Hypertonic - translocational hyponatraemia - osmotically active particles in the plasma induces movement of H2O from ICF -> ECF -> decreasing serum Na+ even though the serum osmolality remains elevated. - agents that cause this: glucose, mannitol, sorbitol, radiocontrast - for each 1mmol/L rise in blood glucose the serum sodium will decrease by 0.3mmol/L *** Advanced renal disease = an important cause of a normal or high serum osmolality - hyponatraemia from the inability to excrete H2O -> lowers osmolality but because of high urea this acts to normalise osmolality or can make it high. - however, urea is an ineffective osmole (as it freely crosses cell membranes) -> therefore does not cause H2O to moved out of cells. - you need to correct serum osmolality for the effect of urea: Corrected serum osmolality = measure osmolality – [urea] HISTORY - speed of onset more important than level most patients won’t be symptomatic until Na+ < 125mmol/L fluid intake/output nausea vomiting neuropsychiatric symptoms muscular weakness headache lethargy psychosis raised ICP seizures coma - medications! - ROS to find precipitant and organ dysfunction - co-morbidities: adrenal disease, liver disease EXAMINATION - cause! - volume status - neurological complications (increased ICP, lateralizing signs) INVESTIGATIONS - diagnostic U+E (Na+, glucose, renal function) plasma osmolality plasma proteins and lipids urinary Na+ sodium deficit = 0.6 x weight in kg x [Na desired - Na measured] Jeremy Fernando (2011) MANAGEMENT - treat cause ideally correct slowly to avoid central pontine myelinolysis quantify duration, severity and type treatment is dependent on cause (1) (2) (3) (4) (5) fluid restriction (< 800mL/day) diuretics isotonic saline (in true volume depletion) oral Na+ tablets hypertonic saline (3%): -> rapid reversal – 100mL (raises Na+ by 2-3mmol/L) Q 10 min until seizures stops -> less rapid – 1mL/kg/hr of LBW - can use desmopressin or dextrose if inadvertent rapid correction takes place Acute (<48hrs) and symptomatic - seizing and coma raise by 1-5mmol/L/hr until symptoms resolve or Na+ 125-130mmol/L hypertonic saline (3%) 1-2ml/kg/hr frusemide 20mg IV Chronic symptomatic (>48 hrs or unknown duration) - calculate Na+ deficit correct Na+ by 10mmol/L/day frusemide 20mg IV N/S fluid restrict repeat Na+ every 2 hours high risk patients = young premenopausal woman Asymptomatic from SIADH - fluid restrict frusemide 20-40mg/day NaCl tablets 3-18g/day urea 30g/day demclocycline 600-1200mg/day current trials underway looking @ AVP V2 receptor antagonists NORMAL RANGES Serum osmolality: 272-295mOsm/kg water (panic values = 240 and 320!) Jeremy Fernando (2011) Urine osmolality: from 50-1400mOsm/kg water (average 500-800) – after an overnight fast urine osmolality should be 3 times the plasma osmolality Urinary Na+ - 15 to 250 mmol/L Jeremy Fernando (2011)