Hyponatraemia - WordPress.com
advertisement
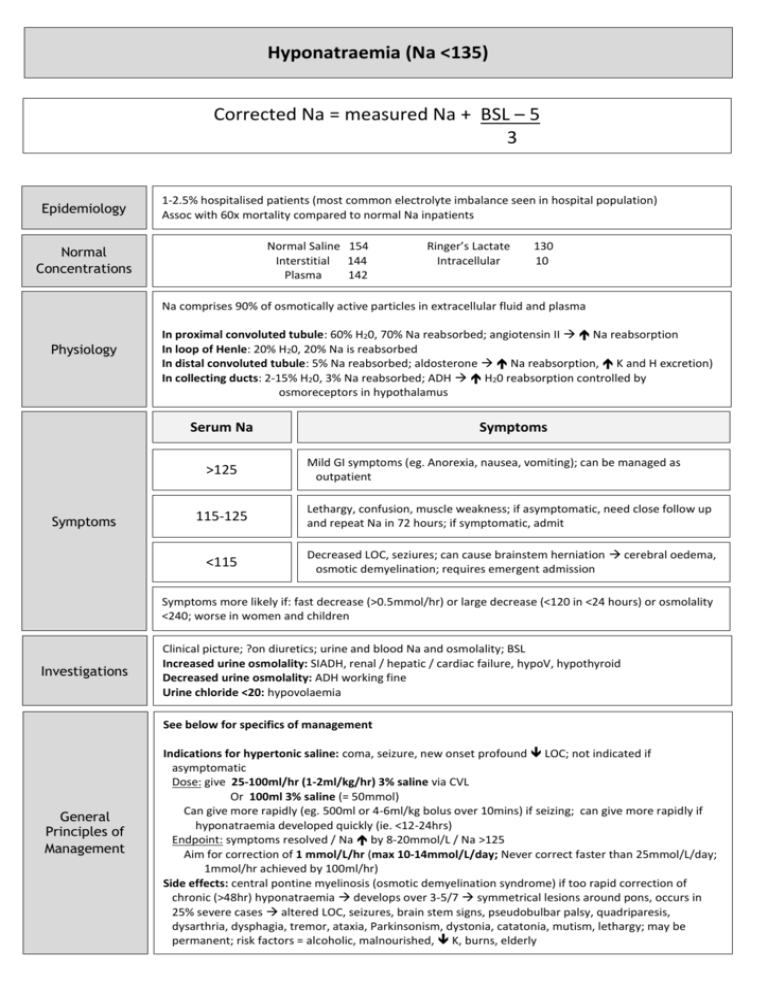
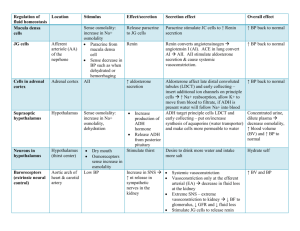
Hyponatraemia (Na <135) Corrected Na = measured Na + BSL – 5 3 Epidemiology 1-2.5% hospitalised patients (most common electrolyte imbalance seen in hospital population) Assoc with 60x mortality compared to normal Na inpatients Normal Saline 154 Interstitial 144 Plasma 142 Normal Concentrations Ringer’s Lactate Intracellular 130 10 Na comprises 90% of osmotically active particles in extracellular fluid and plasma Physiology In proximal convoluted tubule: 60% H20, 70% Na reabsorbed; angiotensin II Na reabsorption In loop of Henle: 20% H20, 20% Na is reabsorbed In distal convoluted tubule: 5% Na reabsorbed; aldosterone Na reabsorption, K and H excretion) In collecting ducts: 2-15% H20, 3% Na reabsorbed; ADH H20 reabsorption controlled by osmoreceptors in hypothalamus Serum Na >125 Symptoms Symptoms Mild GI symptoms (eg. Anorexia, nausea, vomiting); can be managed as outpatient 115-125 Lethargy, confusion, muscle weakness; if asymptomatic, need close follow up and repeat Na in 72 hours; if symptomatic, admit <115 Decreased LOC, seziures; can cause brainstem herniation cerebral oedema, osmotic demyelination; requires emergent admission Symptoms more likely if: fast decrease (>0.5mmol/hr) or large decrease (<120 in <24 hours) or osmolality <240; worse in women and children Investigations Clinical picture; ?on diuretics; urine and blood Na and osmolality; BSL Increased urine osmolality: SIADH, renal / hepatic / cardiac failure, hypoV, hypothyroid Decreased urine osmolality: ADH working fine Urine chloride <20: hypovolaemia See below for specifics of management General Principles of Management Indications for hypertonic saline: coma, seizure, new onset profound LOC; not indicated if asymptomatic Dose: give 25-100ml/hr (1-2ml/kg/hr) 3% saline via CVL Or 100ml 3% saline (= 50mmol) Can give more rapidly (eg. 500ml or 4-6ml/kg bolus over 10mins) if seizing; can give more rapidly if hyponatraemia developed quickly (ie. <12-24hrs) Endpoint: symptoms resolved / Na by 8-20mmol/L / Na >125 Aim for correction of 1 mmol/L/hr (max 10-14mmol/L/day; Never correct faster than 25mmol/L/day; 1mmol/hr achieved by 100ml/hr) Side effects: central pontine myelinosis (osmotic demyelination syndrome) if too rapid correction of chronic (>48hr) hyponatraemia develops over 3-5/7 symmetrical lesions around pons, occurs in 25% severe cases altered LOC, seizures, brain stem signs, pseudobulbar palsy, quadriparesis, dysarthria, dysphagia, tremor, ataxia, Parkinsonism, dystonia, catatonia, mutism, lethargy; may be permanent; risk factors = alcoholic, malnourished, K, burns, elderly Aetiology Investigations Renal Osmotic diuresis: glucose, urea, mannitol Diuretics Mineralocorticoid: hypoaldosteronism Na losing nephropathy: renal tubular acidosis, chronic renal failure, interstitial nephritis, cerebal salt wasting syndrome) ExtraRenal Gastrointesinal loss: diarrhoea, vomiting, NG tube Third space loss: burns, pancreatitis, peritonitis Sweating, blood loss Hypovolaemic Loss of Na > H20 Urinary Na >20 Urinary Na >20 urinary osmolality Kidneys reabsorb Na to make up for their losses Na deficit (mmol/L) = (0.6 x kg) x (desired Na – actual Na) Management: give normal saline correct at <0.5mmol/hr or <12mmol/day; aim to get Na >125 Aetiology Hypotonic = serum osmolality <275 Renal Euvolaemic ExtraRenal Investigations SIADH: ADH holds on to H20 concentrated urine; accounts for 50% of all hyponatraemia; multiple causes as below: CNS: cancer, trauma, infection, CVA, Guillian-Barre syndrome, delirium tremens, multiple sclerosis, SLE, SAH, AIDS RS: cancer (oat cell, bronchogenic), Infection, COPD, cystic fibrosis, abscess, TB Drugs: SSRI, TCA, MAOI, ecstasy, oxytocin, carbamazepine, haloperidol, barbiturates, NSAID’s, tramadol, omeprazole Endocrine: hypothyroidism, hypocortisolism Iatrogenic H20 overdose: bladder irrigation, IV fluids Polydipsia Endocrine: hypothyroidism, hypocortisolism Minimal increase in body water Urinary Na >20 urinary osmolality Urinary Cl >40 Urinary Na <20 Large amounts H20 in urine No change in body Na Management: fluid restrict to 500-1500ml/day; consider ADH antagonist if SIADH Hypervolaemic Aetiology Investigations Renal Acute renal failure: can’t excrete water Urinary Na >20 ExtraRenal Cardiac failure, cirrhosis, nephrotic syndrome H20 but functionally underfilled aldosterone Na retention Urinary Na <20 Management: fluid and salt restrict; loop diuretics; dialysis Isotonic = serum osmolality 275-295 Hypertonic = serum osmolality >295 No change to total body water or Na (ie. Pseudohyponatraemia) Factitious: protein, lipids artifically low Na Therefore requires no treatment Management: fluid restrict to 500-1500ml/day; consider ADH antagonist if SIADH No change to total body water or Na Extracellular solute load water moves into extracellular fluid, diluting Na (eg. Hyperglycaemia, mannitol, glycerol) Management: treat cause (this may cause osmotic diuresis genuine Na) IV fluids may help as often hypovolaemic