Welsh Healthcare Associated Infection Programme (WHAIP) Pilot
advertisement
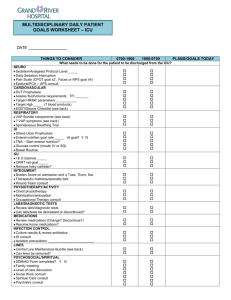
Welsh Healthcare Associated Infection Programme (WHAIP) Pilot evaluation of an alternative definition for Ventilator-Associated Pneumonia (VAP) Author: Richard Pugh, Tamas Szakmany, Wendy Harrison Date: March 2014 Version: 1.2 Publication/ Distribution: Members of WICSARG / WICS Critical care networks Critical care staff (all units in Wales) Purpose and Summary of Document: To provide information on the forthcoming second pilot study which will assess an alternative surveillance definition for VAP in critical care units in Wales. The pilot study is conducted in conjunction with the Welsh Intensive Care Society Audit and Research Group (WICSARG) and the Critical Care Networks. 1 Introduction Since the introduction of surveillance by the Welsh Healthcare Associated Infection Programme (WHAIP), rates of VAP in Wales have been strikingly low compared with other parts of the United Kingdom and Europe, with a mean incidence density of 2.5 episodes per 1000 ventilator days over the period 2008-13. 1 It is hoped that this in part reflects the high compliance of Welsh ICUs with ventilator bundles. However, a previous pilot surveillance study, conducted in November 2012 in 13 of 15 Welsh ICUs, suggested that the currently used surveillance system probably fails to capture a significant proportion of episodes of VAP.2 There are multiple reasons why this may have occurred; however, given that the currently used HELICS definition3 (see appendix, Table 1) for VAP incorporates subjective clinical features (e.g. dyspnoea or purulent sputum), and necessitates performance of chest radiography (which in itself is prone to inter-observer variability4), perhaps failure to capture some episodes is not surprising. Indeed in the previous pilot surveillance study, in a number of cases of apparent ICU-acquired respiratory tract infection, the HELICS VAP definition could not be met because chest radiography had not been performed. In the United States, the Center for Disease Control and Prevention (CDC) until recently operated a VAP surveillance programme using a definition very similar to that of HELICS. However, appreciating the limitations posed by a definition that includes subjective clinical criteria and radiographic features, the CDC recently developed and in 2013 implemented a new surveillance definition to identify complications associated with mechanically ventilated patients.5 This new CDC classification was intended to be objective, streamlined and potentially automatable and defines three tiers of Ventilator Associated Events6 (VAEs; see appendix, Figure 1): 1. Ventilator-Associated Condition (VAC) 2. Infection-related Ventilator-Associated Complication (IVAC), and 3. Possible or Probable Ventilator-Associated Pneumonia (Possible or Probable VAP – used mainly for surveillance purposes) 2 Of note, the primary criteria to be met are a sustained deterioration in oxygen or positive end-expiratory pressure requirements relative to a steady baseline, and this defines a VAC. An IVAC is said to have occurred if in addition to this deterioration, there is abnormal white cell count or temperature, and antibiotics are commenced and continued for a minimum of 4 days. Finally, Possible and Probable VAP are defined on the basis of quantitative measure of pus cells and/ or culture of pathogens from a respiratory specimen. In a retrospective study comparing outcomes according to these new VAEs and the CDC's previous surveillance definition of VAP, VAC was a stronger predictor of hospital mortality than VAP, though VAC and VAP development were both associated with duration of mechanical ventilation, ICU and hospital lengths of stay. 6 In a separate study, a low degree of agreement was found between a traditional VAP definition and VAC and IVAC; in nearly 80% cases of VAP, criteria for VAC were not met, and again VAC and IVAC were stronger predictors of hospital mortality than VAP. 7 Interestingly, higher concordance with VAP prevention guidelines was associated with reduced VAP and VAC (though not IVAC) rates in this study. It has been noted, that this definition allows automation of detection of VACs in an electronic patient information system environment, however data collection could be more difficult in critical care units utilising paper charts (Dr Szakmany, personal communication). To have confidence in the apparent success of VAP-prevention measures in Wales, we need to ensure we are using surveillance methodology most appropriate for our critically ill population, which are cared for in units of different size and specialisation, and with variations in processes of care and indeed data collection. Given the limitations identified with use of the HELICS definition in Wales, it therefore seems appropriate to attempt to evaluate the CDC's objective surveillance methodology as applied to Welsh critical care. Aims 1. To assess the incidence of CDC-defined VAE in Welsh ICUs over a 2 week period 2. To concurrently assess episodes of VAP according to HELICS and CPIS definitions 3. To investigate clinical outcomes according to development of VAE or VAP 3 4. To gauge ease of use of CDC surveillance methodology in a largely nonautomated Welsh critical care setting Methodology Study design To conduct a prospective, observational evaluation of current clinical practice. This study is considered a service evaluation, which does not need Ethical Approval, but will need to be registered with the R&D and/or audit offices of the Health Boards. Data collection Local investigators, identified through the Welsh Intensive Care Society Audit and Research Group (WICSARG) network, will complete a standardised data collection form for each patient receiving invasive (via endotracheal or tracheostomy tube) mechanical ventilation (including CPAP) at the start of or admitted to their critical care unit during the 2-week study period (24th March to and including 6th April 2014) Each form will require the hospital name and patient hospital id. In addition the serial number from the matching routine VAP surveillance form will need to be recorded (NB only if routine surveillance is via paper forms) Baseline characteristic information will be collected for each patient retrospectively by contacting the nominated local study investigators 1 month following the end of the study On a daily basis (or until critical care discharge) data will be recorded regarding: - Whether the patient is invasively ventilated or not - Whether the patient has been invasively ventilated for 48 hours or more at date and time of assessment To determine if the patient meets a VAE and subsequently a VAC, IVAC, Possible VAP or Probable VAP, daily variables will need to be recorded, such as FiO 2, PEEP, temperature, white cell count, antibiotic therapy and clinical features (e.g. change in sputum). Figure 1 in the appendix provides a summary of the requirements When antibiotics therapy is commenced for a presumed new infection, the likely source of infection, according to the Infection Code (e.g. "RTI" for respiratory infection) should be recorded. If antibiotics are commenced when the source of infection is unclear, the Infection Code should be recorded as "UNK"; however, if a source of infection later becomes clear for this episode of infection, then the Infection Code should be recorded on this subsequent day 4 Microbiology relating to a RTI should also be collected. This includes completing the microbiology results from samples collected during the period beginning 48 hours before and ending 48 hours after a new course of antibiotics has commenced. Details will include the specimen type (e.g. BAL, PBS etc.), the organism grown and if the culture is significant (i.e. quantitative / semi-quantitative measure of the growth) To compare the CDC definition to the HELICS definition the following daily information will also be collected in addition to those already noted: chest radiography (with new diffuse or localised change), new bronchial breathing or crepitations, or new cough or dyspnoea Kindly keep a record of forms for each patient which has been included in the study, so that WHAIP can contact you with any queries. In particular, we wish to collect data approximately 1 month after study completion regarding number of advanced respiratory days, duration of critical care stay, and ICU and hospital mortality – all of which data should be available via your ICU’s Ward Watcher database. At the end of the 2-week study period, completed data collection forms should be sent to: John Twiddy, Welsh Healthcare Associated Infection Programme, Temple of Peace and Health, Cathays Park, Cardiff, CF10 3NW Data analysis Data will be analysed by staff at the WHAIP with respect to the following: 1. Episodes of VAC, IVAC and Possible and Probable VAP according to CDC definitions of a Ventilator-Associated Event 2. Episodes of respiratory tract infection (commencement of antibiotic therapy for suspected RTI) 3. Episodes of VAP according to HELICS criteria 4. Episodes of ICU-acquired pneumonia, as defined by modified Clinical Pulmonary Infection Score 8 5 5. Proportion of mechanically ventilated patients who required invasive ventilation for more than 48 hours 6. Baseline characteristics of patients who develop RTI, VAC, IVAC, Possible and Probable VAP, HELICS-defined VAP and VAP according to CPIS (score including microbiological criterion greater than 6) 7. Clinical outcome characteristics of patients who develop RTI, VAC, IVAC, Possible and Probable VAP, HELICS-defined VAP and VAP according to CPIS (score including microbiological criterion greater than 6) Dissemination - Results will be forwarded to all members of the WICSARG group (and may be presented at future WICS meetings), the Critical Care Networks and via the Critical Care Steering Group. - A report will be disseminated by WHAIP (once data is analysed in conjunction with WICSARG) to all critical care units in Wales. - It is anticipated that all Wales data may also be published in conjunction with the above groups. 6 References 1. Welsh Healthcare Associated Infection Programme. Critical Care Annual Report: central venous catheter and ventilator associated pneumonia, January- December 2012, Public Health Wales 2013. www2.nphs.wales.nhs.uk. Date last updated August 7th 2013. Date last accessed November 3rd 2013 2. Szakmany T, Harrison W, Roberts H, Scholey G, Pugh R. Surveillance for ventialtor-associated pneumonia (VAP) in Wales: is HELICS the best way? Crit Care Med 2013; 41 (12 Suppl): 46. 3. Hospital in Europe Link for Infection Control through Surveillance (HELICS). Surveillance of Nosocomial Infections in Intensive Care Units, Protocol Version 6.1, September 2004. 4. Wunderink R. Radiologic diagnosis of ventilator-associated pneumonia. Chest 2000; 117: 188S– 190S. 5. Klompas M, Khan Y, Kleinman K, et al.; CDC Prevention Epicenters Program. Multicenter evaluation of a novel surveillance paradigm for complications of mechanical ventilation. PLoS One. 2011; 6: e18062 6. Magill S, Klompas M, Balk R et al. Developing a new, national approach to surveillance for ventilator-associated events. Crit Care Med 2013; 41: 2467- 75. 7. Muscedere J, Sinuff T, Heyland D, et al.; for the Canadian Critical Care Trials Group. Chest 2013; 144(5): 1453-60. 8. Fartoukh M, Maitre B, Honore S, Cerf C, Zahar J-R, Brun-Buisson C. Diagnosing pneumonia during mechanical ventilation: the clinical pulmonary infection score revisited. Am J Resp Crit Care Med 2003; 168: 173-79 7 Appendix Table 1. HELICS case definition of ICU-acquired pneumonia (adapted from Surveillance of Nosocomial Infections in Intensive Care Units Protocol 3) Criteria Feature Radiological (2 or more serial radiographs in patients with underlying cardiac or pulmonary disease) Suggestive image of pneumonia Systemic (at least one of) 1. Fever (>38oC) Pulmonary criteria (in the absence of supportive microbiological data, at least two of) 2. Leukopoenia (<4 x109/L white blood cells) or leukocytosis (≥12 x109/L white blood cells) 1. New onset of purulent sputum, or change in character of sputum 2. Worsening gas exchange 3. Cough, or dyspnoea, or tachypnoea 4. Suggestive auscultation Patients must fulfil radiological, systemic and pulmonary criteria for VAP 8 Figure 1. Ventilator-associated events surveillance algorithm (adapted from Magill et al. 6 ) 9