Mental Health Nursing I
advertisement

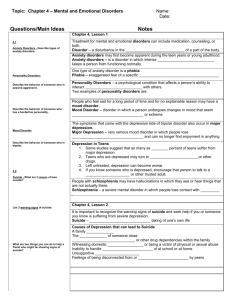
Mental Health Nursing I NURS1300 Lecture Notes Unit V: Mental Health Alterations Objective 1: Describe the mood disorders. A mood disorder is a condition in which the prevailing emotional mood is distorted or inappropriate to the circumstances (Wikipedia, 2007). People with mood disorders experience significantly elevated or depressed moods. Some people experience cycles of elevated mood and depressed mood. Major depression is an episode of depressed mood. A manic episode is an episode of elevated mood. Alternation between significantly depressed mood and significantly elevated mood over time is called bipolar disorder. Psychotic features may be present. Objective 2: Describe the nursing interventions and medical treatment for clients with a mood disorder. Refer to Objective 11 for medications for mood disorder. Electroconvulsive therapy (ECT) – May be indicated for clients with severe depression that does not respond to other treatment Acts more quickly than medications, and may produce fewer side effects in older patients Nursing Diagnoses – Risk for self-directed violence R/T suicidal feelings Risk for violence directed at others R/T homicidal ideation Low self-esteem R/T depression Imbalanced nutrition, less than body requirements R/T lack of interest in food Disturbed sleep pattern R/T depression Objective 3: Describe characteristics of an individual with suicide potential. HealthForums, 2007 – Females attempt suicide 2-3 times as often as males Males are 4 times more likely to complete a suicide Suicide by firearm is the most common method of suicide for both men and women Risk of suicide is higher for people with psychiatric conditions o mood disorder o substance abuse o schizophrenia o anxiety disorder o personality disorder o PTSD Married people with children have the lowest rate of suicide High-risk populations – Previous suicide attempt Family history of suicide Suicide of a friend, co-worker, colleague, or role model Anyone threatening suicide must be taken seriously. Objective 4: State common age groups for suicide. HealthForums, 2007 – Suicide is the 3rd leading cause of death among teenagers and young adults age 15-24, and the leading cause of death for adolescents age 13-18 o often considered a solution to an environmental or psychological problem o often experience hostility toward self o desire to seek revenge on others by hurting self White males over age 70 have the highest rates of suicide o fewer attempts but more completed suicides attempts generally more lethal than those of younger adults decreased ability to recover from or survive a suicide attempt o often occur through covert measures self-inflicted falls refusing to eat refusing to take medication o usually planned instead of impulsive bereavement real or perceived losses physical illness Objective 5: Define personality disorders. A personality disorder is a pattern of perceiving, reacting, and relating to other people and events that is relatively inflexible and that impairs a person’s ability to function socially (Merck, 2007). This disorder involves personality traits which become rigid and dysfunctional. Personality disorders are chronic and maladaptive, impacting all aspects of one’s life. Objective 6: Describe the types of personality disorders. Personality disorders are grouped into three clusters according to traits to help describe them. Personality disorders that fall within Cluster A are characterized by behaviors that are considered odd or eccentric. Cluster B personality traits consist of dramatic, emotional, and erratic behaviors. Clients with Cluster C personality traits exhibit behaviors that are anxious or fearful (Wikipedia, 2007). Cluster A disorders Paranoid personality disorder Schizoid personality disorder Schizotypal personality disorder Cluster B disorders Antisocial personality disorder Borderline personality disorder Histrionic personality disorder Narcissistic personality disorder Cluster C disorders Avoidant personality disorder Dependent personality disorder Obsessive-compulsive personality disorder Objective 7: Identify the nursing interventions and medical treatment for personality disorders. Merck, 2007 – Psychotherapy is the cornerstone of most treatments for clients with a personality disorder. Self-help groups, family support, group therapy, behavior modification, and medication are used as an adjunct to psychotherapy to treat personality disorders. Many clients with a personality disorder experience cocurrent conditions such as anxiety, depression, and substance abuse, and much of their pharmacotherapy is focused on these issues. Nursing diagnoses – Ineffective coping R/T personality disorder AEB reliance on maladaptive defense mechanisms Risk for self-harm R/T unresolved fear of abandonment AEB attention-seeking behaviors and threats against self Depression R/T self-directed anger AEB social withdrawal and isolation Objective 8: Describe behaviors of the schizophrenic and identify causes of schizophrenia. Schizophrenia refers to a group of very serious, usually chronic, thought disorders in which the affected person’s ability to interpret the world accurately is impaired by psychotic symptoms. Typical schizophrenic behaviors include substance abuse, nicotine dependence, disordered thinking, apathetic personality, and changing behaviors (i.e. normal versus abnormal). Sudden onset of severe psychotic symptoms may occur, as well as unusual thinking, speech, and behavior. Social isolation and withdrawal are common. Most behaviors are expressed in relation to symptoms such as distorted perceptions of reality, delusions, and hallucinations (MentalHealthatAbout.com, 2007). The cause of schizophrenia is unknown, but researchers believe people with the disorder were genetically vulnerable to it. Besides biological predisposition and family history, there may be other influencing factors, such as environmental exposure which interrupts brain development (i.e. pregnancy or early childhood), making the individual more susceptible to developing schizophrenia (Schizophrenia.com, 2007). Objective 9: Differentiate the types of schizophrenia. 1. Catatonic type = prominent psychomotor disturbances, stupor, and waxy flexibility 2. Disorganized type = thought disorder and flat affect are present together 3. Paranoid type = delusions and hallucinations are present but thought disorder, disorganized behavior, and affective flattening are absent 4. Residual type = positive symptoms are present at low intensity 5. Undifferentiated type = may include symptoms of more than one subtype of schizophrenia (MedlinePlus, 2007) Objective 10: Discuss the medical treatment and nursing interventions for the schizophrenic client. Medical treatment for the client with schizophrenia involves therapy modalities and antipsychotic medication. Therapies include individual psychotherapy, family education, and community support groups. Hospitalization is often required to treat severe delusions, hallucinations, or self-care deficits (NIMH – National Institute of Mental Health, 2007). Nursing interventions – nonconfrontational speech and mannerisms o do not confirm or refute the delusion, hallucination, or illusion o focus on reality encourage communication and expression of feelings and fears decrease stimuli and offer quiet activities seek clarification of conversations provide recognition for constructive self-care activities make adjustments in food preparation or service for patients with paranoia Objective 11: Identify classifications, uses, actions, and side effects for selected classifications of psychoactive medications as they relate to the above mental health alterations. See Psychoactive Medications handout Neuroleptics are prescribed for the treatment of schizophrenia. Typical neuroleptics were the original antipsychotics, and were useful in treating positive symptoms of schizophrenia. Atypical neuroleptics help with both positive and negative symptoms, and cause fewer side effects. The most common side effect associated with neuroleptics is orthostatic hypotension, which creates a fall risk. o Extrapyramidal symptoms (EPS) may also occur with neuroleptic use due to effects on central nervous system control of involuntary muscle movement. A neuroleptic side effect that requires immediate medical attention is neuroleptic malignant syndrome. This may result in permanent impairment or death. The syndrome involves muscle rigidity, akinesia (emotional unresponsiveness and blunted affect), and respiratory distress. Hyperthermia (body temperature of 101 – 103 degrees or higher) is the cardinal sign of this syndrome. Agranulocytosis, which is an extreme decrease in white blood cells, may occur with use of clozapine. The symptoms of this condition include sore throat and fever. Frequent white blood cell count is required for patients taking clozapine to monitor for a significant drop in WBC levels. If this occurs, or the patient presents with a sore throat, fever, and/or flu symptoms, the nurse must hold the medication and call the physician immediately due to risk for severe infection. MAOIs (monoamine oxidase inhibitors) – not first choice of drugs 2-week period should elapse between ending most antidepressants and beginning an MAOI 4-week “washout” period should occur between stopping MAOI and staring most other antidepressants must be given in divided doses hypertensive crisis o requires immediate medical attention o can result from consuming tyramine during or within 3 weeks after stopping MAOI