30 Mar 2010 - Personality Disorders
advertisement
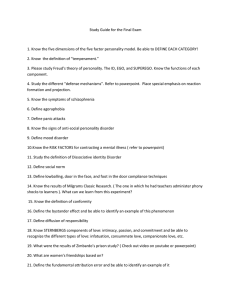
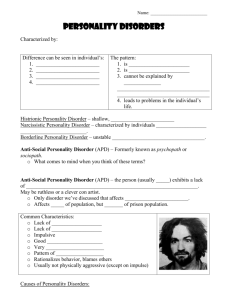
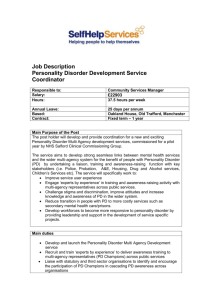
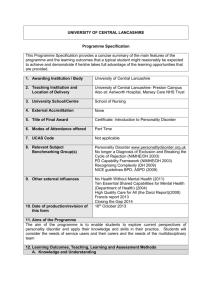
Personality Disorders A Case Presentation Kate Hooks Aims To discuss a complex case and review psychiatric history taking. Look at Personality Disorder. Review the Mental health act and the changes made in 2008 Patient K Pc- Jan 2010 Admitted via the crisis team with depression and suicidal ideation involving her daughter. HPCMiserable from the age of 11. Failed exam for Skipton Girls Eating disorder 1995 first referrall to CAMHS for eating 1999 Grandmother died- admitted after taking an overdose Around this time- mother diagnosed with breast ca Abuse from chef where she worked Abuse from taxi driver- lifts to school Older sister went to university. Around this time started drinking at school (age14) 2000 university 2001 father diagnosed with stomach ca. 2002 Raped by acquaintance ......pregnant. 2003 baby c born Moves back with parents and suffers Postnatal Depression. 2004 Nurse training in Bradford- vulnerable to men. 2005 lives in own cottage drinking 2-3 bottles of wine per day. 2007 Father dies. 2008 2 admissions with suicidal ideas Medical HX IBS Alcoholic polyneuropathy 2009. Medication Pregabalin Thiamine and Vit B Buspirone Quetiapine Ranitidine Lamotrigine Citalopram Previously..... Paroxetine Venlafaxine Fluoxetine Started antidepressants at age 14 Family Hx 56 Teacher 27 29 Teacher 33 solicitor 6 baby Childhood Normal development Happy up to the age 11 Parents ‘loving’ Dad could loose his temper Education Settle Middle school Settle High Edge Hill- Bradford Qualified nurse 2006 Employment Started work 2006 Break for detox later that year Periods of sick leave Gave up in Jan 2009 Relationships Finds sexual relationships difficult 2 brief heterosexual relationships Forensic Put in a police van when trying to jump on railway. Substances Took ecstasy once Previously smoked cannabis Alcohol- 1-4 bottles of wine per day Premorbid personality Describes self as ‘happy’ to age 11. Then only ever brief moments of happiness. Mental state varies on a daily basis and within the consultation. ? Personality Disorder • Cognition • Affect • Behaviour Epidemiology 2-18% in the community Aetiology Genetics Childhood development Neurophysiology Cognitive-behavioural Management Medication- Antipsychotics Anticonvulsants and lithium Antidepressants Therapeutic community Cognitive behavioural therapy ICD10 Types Paranoid Schizoid Dissocial Emotionally unstable- impulsive type Emotionally unstable- Borderline type Histrionic Anxious (avoidant) Anankastic (OC) Dependent The Mental Health Act 1983 Section 2 Admission for assessment Up to 28 days Must be a danger to themselves or to others Application made by an AMHP or nearest relative and supported by 2 doctors One section 12 app. Other usually GP. Section 3 Diagnosis already known Admission for compulsory treatment Up to 6 months Can be extended to 12 months Section 4 Emergency admission If no second medical recommendation For a patient who is not admitted NR or AMHP and 1 registered medical practitioner. 72 hrs 5(2) Inpatient Responsible clinician or nominated deputy 72hrs • 5(4)- nurse holding power 6hrs • 17- Leave • 136- Police officer can detain to safety New- Community Treatment Order Patients detained on section 3 Must- have mental disorder - be appropriate treatment available May need to- Reside at specific address -Available for treatment - avoid specified activities Re called if they become a danger to themselves or others.