Indicators
advertisement
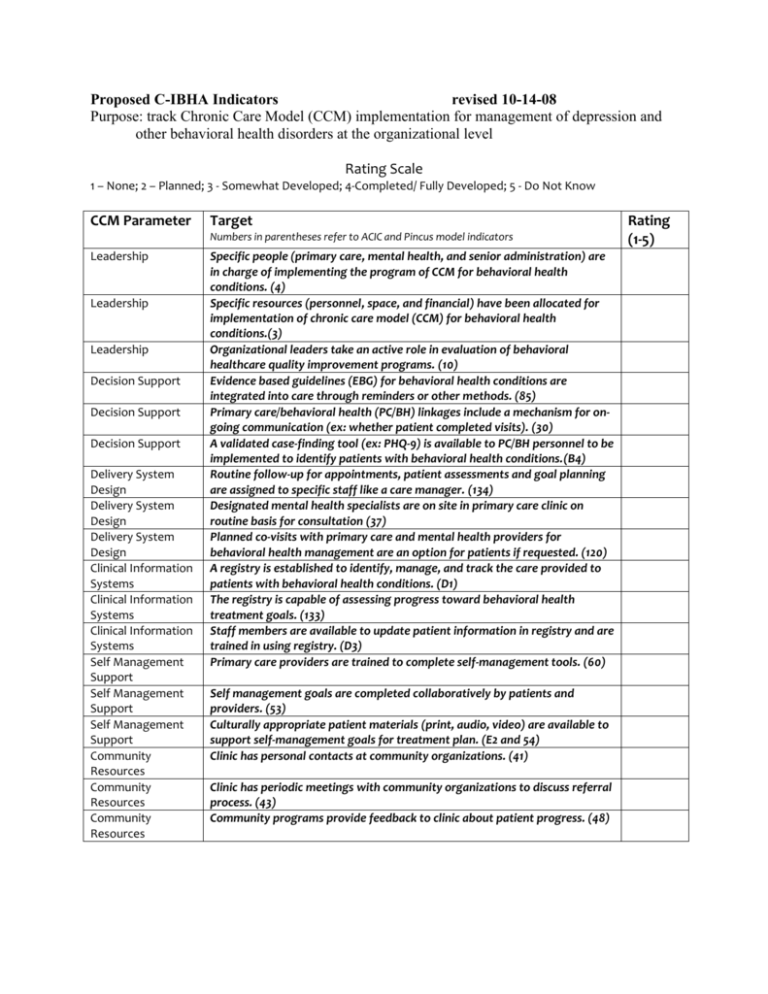
Proposed C-IBHA Indicators revised 10-14-08 Purpose: track Chronic Care Model (CCM) implementation for management of depression and other behavioral health disorders at the organizational level Rating Scale 1 – None; 2 – Planned; 3 - Somewhat Developed; 4-Completed/ Fully Developed; 5 - Do Not Know CCM Parameter Target Numbers in parentheses refer to ACIC and Pincus model indicators Leadership Leadership Leadership Decision Support Decision Support Decision Support Delivery System Design Delivery System Design Delivery System Design Clinical Information Systems Clinical Information Systems Clinical Information Systems Self Management Support Self Management Support Self Management Support Community Resources Community Resources Community Resources Specific people (primary care, mental health, and senior administration) are in charge of implementing the program of CCM for behavioral health conditions. (4) Specific resources (personnel, space, and financial) have been allocated for implementation of chronic care model (CCM) for behavioral health conditions.(3) Organizational leaders take an active role in evaluation of behavioral healthcare quality improvement programs. (10) Evidence based guidelines (EBG) for behavioral health conditions are integrated into care through reminders or other methods. (85) Primary care/behavioral health (PC/BH) linkages include a mechanism for ongoing communication (ex: whether patient completed visits). (30) A validated case-finding tool (ex: PHQ-9) is available to PC/BH personnel to be implemented to identify patients with behavioral health conditions.(B4) Routine follow-up for appointments, patient assessments and goal planning are assigned to specific staff like a care manager. (134) Designated mental health specialists are on site in primary care clinic on routine basis for consultation (37) Planned co-visits with primary care and mental health providers for behavioral health management are an option for patients if requested. (120) A registry is established to identify, manage, and track the care provided to patients with behavioral health conditions. (D1) The registry is capable of assessing progress toward behavioral health treatment goals. (133) Staff members are available to update patient information in registry and are trained in using registry. (D3) Primary care providers are trained to complete self-management tools. (60) Self management goals are completed collaboratively by patients and providers. (53) Culturally appropriate patient materials (print, audio, video) are available to support self-management goals for treatment plan. (E2 and 54) Clinic has personal contacts at community organizations. (41) Clinic has periodic meetings with community organizations to discuss referral process. (43) Community programs provide feedback to clinic about patient progress. (48) Rating (1-5) Chronic Care Model for depression A. Leadership Key Principle(s): There must be a leadership team composed of organizational partners with overall program accountability for implementation across partnering organizations. Please address the following items when describing your current status, planned changes, and projections for technical assistance needed: 1. Team consists of primary care, mental health, and senior administrative personnel; 2. Team has established personnel, space, and financial resources; 3. Team reviews guidelines for treatment and continuous quality improvement; and 4. Team sets target goals for key process measures and outcomes. B. Decision Support Key Principle(s): Evidence-based behavioral health treatment guidelines and care protocols are available to improve recognition and treatment of common behavioral health disorders. Please address the following items when describing your current status, planned changes, and projections for technical assistance needed: 1. Practices have a plan for implementing evidence based guidelines for depression and other common mental health disorders; 2. Practices can systemically identify patients at elevated risk for depression and other common mental health disorders; 3. A validating case-finding tool is available to be implemented to identify patients with depression or other common mental health disorders; 4. Protocol available to stratify treatment intensity by severity; 5. Mental health specialists are available to primary care providers for decision support and patient referral; and 6. Primary care and behavioral health providers and staff understand the decision support tools. C. Delivery System Design Key Principle: A delivery system is available to implement all aspects of decision support. Please address the following items when describing your current status, planned changes, and projections for technical assistance needed: 1. Care managers (CMs) are available and are trained to implement coordinated care in conjunction with primary care providers and mental health specialists (MHSs); 2. A systematized approach has been established for routine follow-up at intervals specific to a patient’s phase of mental health treatment (acute, continuation, or maintenance); and 3. A system is in place to monitor adherence to guideline-based treatment(s) for depression and other common mental health disorders. D. Clinical Information Systems Key Principle: The Clinical Information System (CIS) consists of tools to facilitate the roles of the primary care providers and behavioral health specialists. Please address the following items when describing your current status, planned changes, and projections for technical assistance needed: 1. A registry has been established to identify, manage, AND track the care provided to patients with depression or other common mental health illness patients; 2. The registry (either alone or in conjunction with another information system) can track key process and program measures (e.g., % patients who received a structured assessment for depression and other common mental health disorders, % continuing pharmacotherapy after three months, % patients who achieved a 50% decrease in symptoms) ; and 3. Staff members are available to update patient information in registry AND are trained in using registry. E. Self Management Support Key Principle: Materials, tools, and processes are available to promote patient activation and self-care for behavioral health conditions. Please address the following items when describing your current status, planned changes, and projections for technical assistance needed: 1. Protocols allow for shared decision making between patient and provider(s) that take into account patient preferences for treatment and family involvement; 2. Culturally appropriate patient information on care for depression and other common mental health disorders is available in a variety of formats (e.g., print, audio, and videotape) and language/literacy levels specific to the populations you serve; and 3. Care manager follows up with patients regarding their use of self-management materials. F. Community Resources Key Principle: Patient information and education about behavioral health conditions are available from organizations that are independent of providers and health plans. Please address the following items when describing your current status, planned changes, and projections for technical assistance needed: 1. Decision support materials include protocols for informing patients and families of information and other resources outside the plan or practice that may assist in their understanding of depression and other common mental health disorders and the various treatments available (e.g., clergy, support groups, and local/national organizations); 2. Care managers are updated on available community resources; and 3. Community resources identified are appropriate for addressing the needs of the specific patient populations that are significantly represented in your target population (e.g., African-Americans, immigrants, etc.).