University of Virginia Biosafety Manual
advertisement

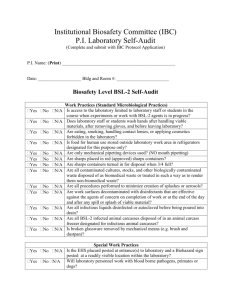
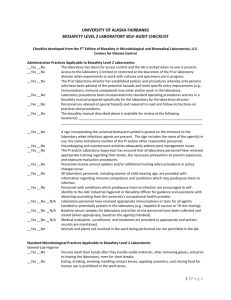
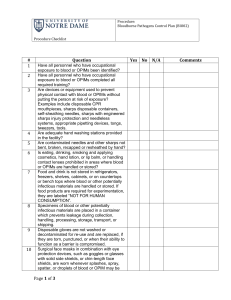
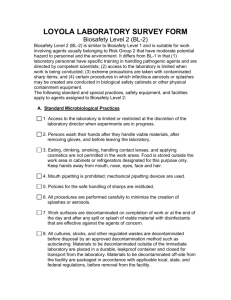
University of Virginia Biosafety Manual And Standard Operating Procedures For Biosafety Level 2 Agents Dr. J. Thomas Parsons University of Virginia Microbiology Department Rooms 223, 224, 2216B Jordan Hall Charlottesville, VA March 26, 2008 2 University of Virginia Biosafety Manual Principal Investigator Lab Building/Rooms Dr. J. Thomas Parsons Jordan Hall/ Rooms 223, 224, 2216B Agents used: BSL-2 Microorganisms Rooms 2216B & 223 Adenovirus Lentivirus Human-derived materials Room 224 A549 IGROV Asp-Pc1 Ishikawa BxPc3 L3.6pl CaOV-3 LNCap Colo357 LP-9 DU145 MCF-7 ES-2 MD-MBA-231 FG MD-MBA-468 H23 MeT5A H460 MPanc 96 H1650 OvCar-3 H1975 Panc1 HEC-1A PC3 HEC-50co PC12 HEK293 RL-95 HeLa SKOV-3 SK-UT Biotoxins/room None Principal Investigator’s Certification I hereby certify that I have reviewed the contents of this manual and that it reflects my current operating practices. Signature____________________ Date_________________ Annual Review: Signature____________________ Date_________________ Signature____________________ Date_________________ 3 Contact Information Office of Environmental Health and Safety 982-4911 Institutional Biosafety Committee (IBC) 982-1597 UVA-WorkMed (formerly Occupational Health Services) 243-0075 UVA Employee Health 924-2013 Student Health Center 924-5362 Principal Investigator’s Home Phone 540-248-1225 4 SIGNATURE and ACKNOWLEDGEMENT PAGE Authorization All members of the J.T. Parsons Lab who have signed the list below are approved for entry into Rooms 2-23, 2-24, and 2-2216B while work with BSL 2 agents is in progress. HOWEVER, only those persons who have attended the OSHA Bloodborne Pathogens lecture and are otherwise specifically trained (e.g., the University Biosafety Officer provides a short training program entitled, “Fundamentals of Biosafety”) may perform work with samples or cell cultures in Rooms 2-23, 2-24, 2-2216B. Anyone (including any workers not in the P.I.’s Lab) who uses Rooms 2-23, 2-24, and 2-216B must sign the disclaimer below. Disclaimer We, the undersigned, understand that adenovirus and lentivirus are in use in the Tissue Culture Room (2-23), Room 2-24, and Room 2216B on the second floor of Jordan Hall, and that these agents are infectious to humans. We agree to follow BL2 containment when using adenoviruses, lentiviruses, or virus-infected cells, and to follow appropriate precautions to prevent inadvertent exposures to these agents. Further, we have read and understood this manual and agree to attend required Bloodborne Pathogens lectures prior to handling samples in Rooms 2-23, 2-24, and 2216B, Jordan Hall. Name Todd Bauer Cheryl Borgman Catherine Cowan Pablo Grigera Christine Harrer Dan Hershey Linda Patchel Amy Koski Marcin Iwanicki Tom Parsons Jill Slack-Davis Jayme Stokes Rob Tilghman Signature Date HBV Yes/No/ Declined? 5 6 Authorization and Disclaimer for Weber Laboratory We, the undersigned, understand that adenovirus and lentivirus (low titers) are in use in the Tissue Culture Room (2-23), and Room 2-24, on the second floor of Jordan Hall. We have been informed that the Biosafety Manual for the JT Parsons laboratory is available for review and is located in room 225 A and on the JT Parsons lab web page (http://faculty.virginia.edu/tparsons/). We agree to follow BL2 containment when using adenoviruses, lentiviruses, or virus-infected cells and to follow appropriate precautions. Name Signature Date 7 8 Rooms 223 and 232 9 Rooms 224 & 225 10 Table of Contents Principal Investigator Certification and Agent Inventory 2 Signatures and Acknowledgement of Risk 4, 5 Biosafety Manual (must be completed by all Investigators working with BSL2 microorganisms and/or human-derived materials and/or toxins of biological) origin) 1. Purpose 2. Responsibilities 3. Background 4. Work Practices A. Standard Practices for BSL-2 agents B. Safety Equipment C. PPE D. Lab Standard Operating Procedures 5. Waste Disposal A. Liquids B. Sharps C. Solid Wastes D. Research Animal Carcasses 6. Spill Clean Up Procedures A. Spills Outside of a Containment Device B. Spills inside a Biosafety Cabinet C. Spills in a Centrifuge D .Biological/Radioactive Emergencies/Spills 7. Proper Use of a Biosafety Cabinet 8. Emergency Phone Numbers and Procedures A. Fire B. Injury C. Exposure to Biohazardous Materials D .Security Incidents 9. Shipping Infectious Substances 11 11 12 14 14 16 16 17 17 18 18 18 19 19 19 20 20 21 21 22 23 23 23 23 24 Appendix A. Exposure Control Plan (must be completed by investigators working with human-derived materials including human cell lines) 25 Appendix B. Toxin Safety Plan (must be completed by investigators working with toxins of biological origin) 37 11 1. Purpose This Biosafety Manual outlines procedures for using and disposing of Biosafety Level 2 (BSL-2) agents. All University laboratories using BSL-2 agents must comply with the procedures in this manual. Principal Investigators or laboratory supervisors must contact the Office of Environmental Health & Safety if they are uncertain how to categorize, handle, store, treat or discard any biohazardous material. 2. Responsibilities The Principal Investigator: 1. Ensures that laboratory and support personnel receive appropriate training for the potential hazards associated with the work involved, the necessary precautions to prevent exposures, and the exposure evaluation procedures. 2. Ensures biosafety procedures are incorporated into standard operating procedures for the laboratory. 3. Ensures personal protective equipment and necessary safety equipment is provided and used. 4. Ensures compliance by laboratory personnel with the relevant regulations, guidelines, and policies 5. Reviews and updates the Biosafety Manual annually. 6. Submits a written report to the Institutional Biosafety Committee concerning: Any accident that results in inoculation, ingestion, and inhalation of biohazardous materials or recombinant DNA Any incident causing exposure of personnel or danger of environmental contamination. Any problems pertaining to operation and implementation of biological and physical containment safety procedures or equipment or facility failure. Laboratory Personnel 1. Participates in appropriate training and instruction 2. Complies with biosafety procedures. 3. Reports all accidents, major spills, or exposure incidents to supervisor 4. Reviews the Biosafety Manual annually. Additional Responsibilities for this lab - 12 3. Background The focus of the laboratory of Dr. J. Thomas Parsons is to study adhesion signaling as it relates to cell growth, migration and metastasis. The potentially infectious biological materials used in this work include viral vectors (adenovirus and retrovirus), and human cells and tissues which will be handled at the BSL2 level. Also, BSL 1 level agents are used such as recombinant DNA, E.coli K12, and baculovirus. Specific details regarding the use of BSL2 level agents is described below. Avian retroviruses are commonly used to transfer new genetic constructs into cultured chick embryo fibroblast cells (CEF). The constructs used in the Parsons laboratory use a vector system, RCAS-A and RCAS-B, designed by Hughes, et al (J. Virol. 61:3004-3012) in which the gene of interest is cloned into a replication-competent plasmid and transfected into CEF cells. This results in the expression of the introduced gene in CEF cells and also the production of recombinant infectious virus, containing the viral recombinant RNA genome and the viral structural proteins. Virus generated by this procedure is used in further infections of CEF cells. These avian retroviruses are restricted to avian cell lines and are NOT capable of infecting cells of other species. Nevertheless, it is prudent that these viruses and infected cells be handled as a potential hazard if the gene introduced is biologically active (e.g. an oncogene). Examples of such oncogenes used in the laboratory include the tyrosine kinase Src and the small GTPases Ras and Cdc42. Thus, RCAS virus stocks, infected and transfected CEF cells will be handled at the BL2 level of containment, as described below. Human Adenovirus Type 5 (Ad5) will be employed to transfer genetic constructs into mammalian cancer cell lines and primary rodent cells. The Ad5 genome (100 map units, mu) containing a 4.3 kB insert which renders the virus defective in packaging will be co-transfected into human HEK293 cells with a shuttle plasmid containing the CMV promoter and the coding sequence of the gene of interest flanked by 0-1 mu and 9-16 mu of the Ad5 genome. Following recombination, the cassette will replace the 4.3 kB insert and the E1 region of the genome, making the virus capable of packaging but replication defective. The HEK293 cell line is Ad5 transformed and expresses the E1 region (1-11.3 mu) in trans which allows for replication of the recombinant adenovirus. Virus is collected from cells and purified by cesium-chloride gradient. Virus is then incubated with the cells of interest at 20-100 plaque forming units/cell. The Ad5 virus stocks, infected HEK293 packaging cells and target cells will be handled at the BSL2 level of containment, as described below. Retroviruses will be used to infect rodent and human cells lines to allow for over expression of defined proteins or expression of small interfering RNAs to selectively suppress the expression of targeted proteins. Appropriate virus stocks are generated using transfection of HEK293 cells with three separate plasmids, each containing a different component of the virus. The transducing vector is pLKO.1 puro (Sigma); it contains a hairpin insert corresponding to the gene to be targeted, an RRE rev response element, self-3' inactivation long 13 terminal repeat and RNA packaging signal. The packaging plasmid is CMVdeltaR8.2 (obtained from David Rekosh, UVa. It has HIV-1 structural proteins, NEF and Rev downstram of CMV promotor. The envelope vector, MDg (David Rekosh) encodes VSV-G under beta globin promotor. These plasmids are transfected into HEK293 T cells and supernatants are collected 48 hrs later. Transfection of HEK293 cells with the three plasmids generates replication defective virus particles that can be used to infect human or rodent cells to effect the knockdown of selected genes in the target cells. The tripartite vector system ensures that there is no infectious virus produced. Generation of the virus and subsequent infection of target cells is carried out using BSL2 containment. Human cell lines and archival human tumor samples will also be handled at the BSL 2 level because of the possibility that they contain unidentified etiologic agents. The Parsons laboratory does not use any biotoxins regulated by the Antiterrorism and Effective Death Penalty Act of 1996. 14 4. Work Practices Many laboratory procedures using BSL-2 agents can be safely done on the open laboratory bench utilizing good microbiological techniques and appropriate Personal Protective Equipment (PPE) provided the potential for producing splashes or aerosols is low. Work on the open laboratory bench is permitted, except when performing activities with BSL-2 agents that may produce aerosols or splashes. Procedures with a potential for creating infectious aerosols or splashes must be conducted in a certified Biosafety Cabinet (BSC). These may include centrifuging, grinding, blending, vigorous shaking or mixing, sonic disruption, opening containers of infectious materials whose internal pressures may be different from ambient pressures, inoculating animals intranasally, and harvesting infected tissues from animals or embryonate eggs. A. Standard Microbiological Practices for Biosafety Level 2 agents 1. Access to the laboratory is restricted when work with BSL-2 agents is in progress. Access may be restricted by locking doors, posting warning signs or using other suitable methods as determined by the Principal Investigator. 2. A biohazard sign must be posted on the entrance to the laboratory when BSL-2 agents are in use. Information to be posted includes the agent(s) in use, the Biosafety level, the investigator's name and telephone number, and any personal protective equipment that must be worn in the laboratory. 3. Persons wash their hands after they handle viable materials, after removing gloves, and before leaving the laboratory. 4. Eating, drinking, smoking, handling contact lenses, and applying cosmetics are not permitted in the laboratory. Food is stored outside the laboratory. 5. Mouth pipeting is prohibited; mechanical pipeting devices are used. 6. All procedures are performed carefully to minimize the creation of splashes or aerosols. 7. Work surfaces are decontaminated with disinfectants that are effective against the infectious agents present upon completion of work or at the end of the day and after any spill or splash of viable material 8. Chairs and other furniture are covered with a non-fabric material that can be easily decontaminated. Carpets and rugs in laboratories are inappropriate. 9. All cultures, stocks, contaminated wastes and other Regulated Medical Waste (RMW) are disposed of in accordance with University of Virginia Infectious Waste Disposal Procedures (see page 15). 15 10. A sharps management program is in place including: a. Needles and syringes or other sharp instruments should be restricted in the laboratory for use only when there is no alternative. b. Used disposable needles must not be bent, sheared, broken, recapped, removed from disposable syringes, or otherwise manipulated by hand before disposal; rather, they must be carefully placed in a conveniently located Sharps Container. Non-disposable sharps must be placed in a hard-walled container for transport to a processing area for decontamination, preferably by autoclaving. c. Syringes which re-sheathe the needle, needleless systems, and other safety devices are used when appropriate. d. Broken glassware must not be handled directly by hand, but must be removed by mechanical means such as a brush and dustpan, tongs, or forceps. 11. Cultures, tissues, specimens of body fluids, or potentially infectious wastes are placed in a container with a cover that prevents leakage during handling, processing and storage. 12. Transport of BSL-2 agents to sites within the grounds of UVA, must be placed in a secondary leak proof carrier that can contain the contents if the primary container were to leak or break. Carriers must have the biohazard label affixed to the outer surface of the transport container 13. Contaminated equipment must be decontaminated before it is sent for repair or maintenance or before removal from the laboratory. 14. Spills and accidents that result in overt exposures to infectious materials are immediately reported to the Principal Investigator and UVAWorkMed. 15. Animals not involved in the work being performed are not permitted in the lab. 16. Additional Special Practices for this Laboratory Spills and accidents which result in overt exposure to virus containing oncogenic recombinant DNA molecules will be immediately reported to J.T. Parsons. Medical evaluation, surveillance and treatment will be provided as outlined in the CDC-NIH Biosafety Manual for personnel at risk. Infectious agents will not be mixed with radiochemicals. 16 B. Safety Equipment 1. Properly maintained and annually certified biological safety cabinets, preferably Class II, or other appropriate personal protective equipment or physical containment devices are used whenever procedures with a potential for creating infectious aerosols or splashes are conducted. These may include centrifuging, grinding, blending, vigorous shaking or mixing, sonic disruption, opening containers of infectious materials whose internal pressures may be different from ambient pressures, inoculating animals intranasally and harvesting infected tissues from animals or embryonate eggs. 2. Centrifugation presents a physical hazard in the event of mechanical disruption. Aerosols and droplets may also be generated. High concentrations or large volumes of infectious agents may be centrifuged in the open laboratory if sealed rotor heads or centrifuge safety cups are used, and if these rotors or safety cups are opened only in a biological safety cabinet. C. Personal Protective Equipment (PPE) 1. Laboratory coats or gowns are worn while work is performed in the laboratory. Lab coats are removed before leaving for non-laboratory areas (e.g., cafeteria, library, administrative offices). All protective clothing is either disposed of in the laboratory or laundered by an approved outside vendor. Lab coats are never taken home by personnel. Prior to sending out for laundering, contaminated coats must first be decontaminated by autoclaving or soaking in a freshly prepared 10% bleach solution for 10 minutes. 2. Gloves are worn when hands may contact potentially infectious materials, contaminated surfaces or equipment. Gloves are disposed of when overtly contaminated, and removed when work with infectious materials is completed or when the integrity of the glove is compromised. Disposable gloves are not washed, reused, or used for touching "clean" surfaces (keyboards, telephones, etc.), and they should not be worn outside the lab. Hands are washed following removal of gloves. 3. Face protection (goggles, mask, face shield or other splatter guard) is used for anticipated splashes or sprays of infectious or other hazardous materials to the face when the BSL-2 agents must be manipulated outside the BSC 4. Respirators are generally not required when working with BSL-2 agents. Respirators should only be used after consultation with the Office of Environmental Health and Safety. Fit testing, respirator training and annual medical surveillance are required. 17 D. Laboratory Standard Operating Procedures Describe the laboratory procedures using BSL2 agents that will be performed in a BSC and the PPE used: Cell cultures will be Work with BSL 2 agents in open containers will only be done in the designated hood in Room 223 Jordan. Gloves and laboratory coats will be worn when working with live virus or virus-producing cells. No razor blades, scalpels, or hypodermic needles are permitted while working with live virus. Describe the laboratory procedures using BSL2 agents that will be performed on the open bench and the PPE used: Living BSL 2 agents will not be handled on open lab benches, but only in a certified biosafety cabinet. List the disinfectant used for routine decontamination : Work surfaces will be decontaminated after each use with 70% ethanol. In addition, the surface of all equipment used in manipulations will be decontaminated with 70% ethanol. Materials that come into direct contact with the virus will be decontaminated with bleach (0.3% NaOCl) and allowed to stand for 15 minutes before autoclaving in a biohazard bag. Decontamination of vessels containing liquid will be achieved by adding bleach to a final concentration of at least 0.3%. After 15 minutes, bleached liquid will be disposed into the drain. 5. Infectious Waste Disposal Infectious Waste or “Regulated Medical Waste” (RMW) is defined as any waste materials that are capable of producing a disease by an organism likely to be pathogenic to humans, such as the following: 1. Discarded cultures and stocks of microorganisms, specimens, vaccines and associated items containing organisms likely to be pathogenic to healthy humans. 2. Human blood and certain body fluids as defined by OSHA. 3. Items saturated or caked with human blood or body fluids that would release blood/body fluid in a liquid or semi liquid state if compressed or would flake if handled. 4. Human tissue, human cell lines or anatomical wastes 5. Sharps (needles, syringes with attached needles, and scalpel blades, etc). 18 6. Animal carcasses, body parts, bedding and related wastes when intentionally infected with organisms pathogenic to healthy humans. 7. Any residue that results from the clean up of a spill of infectious waste. 8. Any waste contaminated by or mixed with infectious waste. The disposal of RMW is both highly regulated and very costly. University of Virginia faculty, staff and students must use the utmost care to segregate all waste materials properly A. Liquids: Durable, leak proof containers will be used to receive liquid waste. Liquids are decontaminated by adding bleach to a final concentration of 10% or other appropriate disinfectant to a final concentration recommended by the manufacturer. Mix well and allow to stand for fifteen minutes or recommended time, whichever is greater. Pour decontaminated liquid into the sink and rinse with copious amounts of cold water. Liquid waste that is not compatible with disinfectant must be autoclaved for at least 30 minutes, using slow exhaust before disposal. B. Sharps: (needles, syringes with attached needles, and scalpel blades, scissors lancets, guidewires, contaminated glass pasture pipettes, etc). Disposable sharps must be placed in a plastic sharps container as soon after use as possible. Approved sharps containers are available from the UVA Hospital Storeroom. Sharps containers must be located as close as possible to the area where sharps are used. When the sharps container is a ¾ full, close it and place it a UVA “Contaminated Materials Container” (CMC) for final disposal. C. Solid Wastes: Solid infectious waste material (other than sharps) may be autoclaved in the lab in clear autoclave bags and then disposed of as regular trash. The outside of the receptacles containing the autoclave bag should be marked with the biohazard symbol until processing has been completed. Alternatively, solid infectious waste may be disposed of directly into a UVA “Contaminated Materials Container” (CMC) CMCs are available from the UVA Hospital Storeroom. These containers must be lined with red bags. Once a CMC is full, the top must be taped closed and properly labeled with the generator’s name, building, room number, phone extension and date. CMCs are either removed and managed by UVA Environmental Services Department or brought to the appropriate storage area for your building (contact the Office of Environmental Health & Safety, OEHS 2-4911 for information on this location) where it will be removed and managed by OEHS. If the outside of the CMC becomes contaminated, the waste must be repackaged by placing it into a secondary container that meets all the requirements of CMCs. CMCs are sterilized at the Hospital Waste Sterilizer. 19 D. Animal Carcasses: Research Animal carcasses that have been intentionally infected with organisms likely to be pathogenic to healthy humans, inoculated with human-derived materials, or are otherwise considered ABSL-2 must be put in red plastic bags and disposed of in the vivarium cold room or designated freezer. Contact the Center for Comparative Medicine for additional information and guidance. 6. Biohazard Spill Clean up Procedures All major spills must be reported to the Principal Investigator A major spill is one in which: the spill splashes over an area larger than one foot in diameter, the extent of the spill is undetermined, or the spill involves an aerosol. All spills must be described in your Biosafety Manual. The description must include: 1) the type of spill, 2) the time and date it happened, 3) the time and date it was cleaned up, and 4) the time and date you autoclaved the waste from the spill. A. Spills outside of a containment device: 1. Close off spill area to traffic, and notify coworkers. 2. If the spill may involve an aerosol, leave the room for 30 minutes to allow aerosols to settle. 3. Remove contaminated clothing and wash exposed skin. 4. Put on gloves and lab coat. 5. Contain the spill with paper towels. 6. Flood the spill area with a freshly prepared 1:10 dilution of chlorine bleach. If dilution is not possible, undiluted household bleach can be used taking care not to splash the bleach onto oneself. Leave on for 10 minutes. 7. Push the towels at the edge of the spill into the spill's center. Add more paper towels as needed. 8. Discard the paper towels into a regulated medical waste container (CMC). If glass is present, do not use bare hands! Use forceps or a dustpan to remove large pieces. Leave small pieces for clean up by Environmental Services, cover with paper towels and block off area. 9. If contact with bleach occurs with skin, mucous membranes or eyes, flush area with copious amounts of water. 10. Discard gloves into regulated medical waste container. Wash hands thoroughly. 11. Report incident to supervisor and Principal Investigator. 20 B. Spills inside of a Biological Safety Cabinet Prepare a fresh dilution of 1:10 bleach, or use another appropriate nonrinse disinfectant. Allow sufficient contact time (10 minutes for bleach). If using another disinfectant, manufactures directions must be followed. 1. Put on gloves and lab coat. 2. Disinfect the contaminated absorbent paper toweling if present then discard it into the biohazard bag or CMC. 3. Wipe down the cabinet interior and any items inside the BSC with a towel dampened with disinfectant 4. The spilled fluid and disinfectant solution on the work surface must be absorbed with paper towels and discarded into a CMC. 5. Spills large enough to result in liquids flowing through the front or rear grilles require more extensive decontamination; consult OEHS for guidance. C. Spills in a centrifuge 1. Wait at least 30 minutes after centrifuge has stopped before opening (or reopening if breakage is discovered after the machine has stopped). 2. Before attempting to deal with the leak, prepare a pan of non-rinse sanitizer disinfectant solution large enough to immerse the entire bucket for at least 20 minutes (bleach can cause corrosion). 3. Don any protective gear needed to clean up spills. If the rotor is sealed, and removable, place it in the biosafety cabinet before opening and carefully remove the lid from the rotor. If the rotor is not removable, remove the buckets and place them in the BSC. 4. Retrieve unbroken tubes, wipe outside with disinfectant, and leave them in the cabinet, out of the way. The broken tube must be removed with a forceps or other instrument if possible and immersed in a beaker of disinfectant solution for a minimum of fifteen minutes. Do not use bare hands. 5. All instruments and rotor pieces involved in the incident must be chemically decontaminated before re-use. After proper decontamination, instruments and rotor pieces may be washed with a mild detergent according to the manufacturer’s instructions. 6. The inside of the centrifuge chamber must be wiped out with disinfectant. 21 D. Biological/Radioactive emergencies/spills The Radiation Safety Office (982-4911) must be notified and will assist in the clean up of a biological/radioactive spill. Determine if anyone has been contaminated; remove contaminated clothing and wash contaminated skin with soap and water. Proceed with clean up as instructed by the Radiation Safety Office. The infectious agent will be neutralized first, taking care in choosing a disinfecting agent to avoid chemical incompatibility. Chlorine compounds such as bleach must NOT be used to disinfect anything containing 125I because the chlorine will cause the volatilization of radioactive iodine. 7. Proper use of the Biological Safety Cabinet (BSC) Biosafety Cabinets must be certified annually. BSCs are certified by an outside contactor at no cost to the Investigator. Contact OEHS for details. 1. BSC fans must run for 10-15 minutes prior to working in the cabinet and after completion of work. 2. Minimize other activities in the room (e.g., rapid movement, open/closing room doors, etc.) to avoid disrupting the cabinet air barrier. 3. Laboratory coats should be worn buttoned over street clothing; gloves are worn to provide hand protection. 4. Before beginning work, the investigator must adjust the stool height so that his/her face is above the front opening. 5. Plastic-backed absorbent toweling can be placed on the work surface (but not on the front or rear grille openings). This toweling facilitates routine cleanup and reduces splatter and aerosol formation during an overt spill. 6. Closure of the drain valve under the work surface must be done prior to beginning work so that all contaminated materials are contained within the cabinet should a large spill occur. 7. Place necessary materials in the BSC before beginning work. This serves to minimize the number of arm-movement disruptions across the air barrier of the cabinet. All materials must be placed as far back in the cabinet as practical, toward the rear edge of the work surface and away from the front grille of the cabinet 8. The front grille must not be blocked with research notes, discarded plastic wrappers, pipeting devices, etc. 9. Aspirator suction flasks must contain an appropriate disinfectant, and an in-line filter. This combination will provide protection to the central building vacuum system or vacuum pump, as well as to the personnel who service this equipment. Inactivation of aspirated materials can be accomplished by placing sufficient chemical decontamination solution such as bleach, into the flask to kill the microorganisms as they are collected. Once inactivation occurs, liquid materials can be disposed of as noninfectious waste. 22 10. Horizontal pipette discard trays containing an autoclave bag or an appropriate chemical disinfectant should be used within the cabinet. Upright pipette collection containers placed on the floor outside the cabinet or autoclavable biohazard collection bags taped to the outside of the cabinet should not be used. The frequent inward/outward movement needed to place objects in these containers is disruptive to the integrity of the cabinet air barrier and can compromise both personnel and product protection. 11. All operations should be performed on the work surface at least four (4) inches from the inside edge of the front grille. 12. Active work should flow from the clean to contaminated area across the work surface. Bulky items such as biohazard bags, discard pipette trays and suction collection flasks must be placed to one side of the interior of the cabinet. 13. Open flames are rarely necessary in the near microbe-free environment of a biological safety cabinet. An open flame creates turbulence that disrupts the pattern of HEPA-filtered air supplied to the work surface. When deemed absolutely necessary, touch-plate microburners equipped with a pilot light to provide a flame on demand may be used. Internal cabinet air disturbance and heat buildup will be minimized. The burner must be turned off when work is completed. 14. Clean Up: Upon completion of work, the final surface decontamination of the cabinet must include a wipe-down of the interior surfaces. Investigators must remove their gloves and gowns in a manner to prevent contamination of unprotected skin and aerosol generation and wash their hands as the final step in safe microbiological practice. Investigators must determine the appropriate method of decontaminating materials that will be removed from the BSC at the conclusion of the work. 8. EMERGENCY PHONE NUMBERS AND PROCEDURES Emergency Phone Numbers Fire and Medical Emergencies within the Medical Center ….. 924-2012 Fire and Medical Emergencies.................................................9+911 Police……………………………………………………………… 9+911 Principal Investigator’s Home Phone…………………............. 540-248-1225 UVA-WorkMed (formerly Occupational Health Services) ……243-0075 UVA Employee Health……………………………………………924-2013 Hospital Emergency Room……………………………………… 924-2231 Office of Environmental Health and Safety……………………. 982-4911 Evacuation Meeting Place for Laboratory Personnel – Jefferson Park Avenue entrance of Jordan Hall. 23 A. Fire In case of fire, activate the fire alarm pull station and evacuate immediately. Judgment should be exercised in deciding whether to store or contain any hazardous materials prior to evacuation. Remove contaminated protective garments and gloves before leaving laboratory if possible. B. Injury If an injury is life threatening call 9-911. For less serious injuries treatment should be sought at UVA-WorkMed (formerly Occupational Health Services) or UVA Employee Health during weekday, daytime hours. During night and weekend hours, treatment should be sought at the UVA Hospital Emergency Room. Any injury to a laboratory worker shall be reported as soon as possible to the Principal Investigator. C. Exposure to Biohazardous material An exposure is defined as: BSL-2 agent contact with broken skin, eyes, nose, mouth, other mucous membranes, a percutaneous injury with a contaminated sharp, or contact with an infectious agent over a large area of apparently intact skin. In the event of exposure: 1. Wash the area with soap and water or flush eyes, nose or mouth with large amounts of water for 15 minutes. 2. Staff must report immediately to UVA-WorkMed or UVA Employee Health, or after hours to the Hospital Emergency Room. Students must report to the Student Health Center 8am-5pm Monday-Friday or to the Emergency Room after hours. 3. All exposures must be reported to the immediate supervisor and Principal Investigator. 4. Principal Investigators are responsible for reporting exposure incidents to the Institutional Biosafety Committee. D. Security incidents Security incidents such as suspicious visitors, missing chemicals, or missing infectious agents must be promptly reported to the Principal Investigator. University Security or Police should be notified. Principal Investigators are responsible for reporting incidents to the Institutional Biosafety Committee.. 24 9. Shipping Biological and Infectious Substances The transportation of biohazardous substances is regulated by the U.S. Public Health Service, the Department of Transportation and the International Air Transport Association (IATA). University personnel who ship infectious substances including diagnostic specimens, microorganisms, human-derived materials, etc. must complete a training program. The Office of Environmental Health and Safety offers a regularly scheduled course and also has a proprietary training module available on compact disc. Individuals who complete training must retain documentation confirming that they passed the final exam. Training is valid for two years. This Lab does not ship Infectious substances, Diagnostic Specimens or Biological Agents (includes Human-derived materials and Human cell lines). X This Lab ships Infectious substances, Diagnostic Specimens or Biological Agents (includes Human-derived materials and human cell lines). List Personnel trained, date of training and attach the training certificate. Shipping Infectious Substances and Diagnostic Specimens Training Training Certificate on following page. Name Linda Patchel Date April 19, 2007 25 Appendix A Exposure Control Plan (must be completed by investigators working with human-derived materials including human cell lines) Table of Contents I. II. III. IV. V. Vl. VIl. Vlll lX. X. Introduction Exposure Determination Methods of Compliance A. Universal Precautions B. Engineering and Work Practice Controls Communication of Hazards to Employees Hepatitis B Vaccination Policy Procedures for Exposure Incidents Employee Training Recordkeeping Procedures Hepatitis B Vaccine Safe Medical Devices Available 25 25 26 26 26 29 30 30 31 31 33 34 26 I. Introduction This Exposure Control Plan was prepared by the University of Virginia to reduce employee exposure to bloodborne pathogens in accordance with OSHA standard 29 CFR 1910.1030 and Virginia state law. This plan must be reviewed by the Principal Investigator annually and in the event of interim changes. A copy of this plan is available for review by any employee during their work shift. Principal Investigators have 15 days to provide a written copy of this plan to any employee who requests it. II. Exposure Determination This plan covers all employees who may reasonably be anticipated to be at risk for exposure to human blood, or other potentially infectious materials (“OPIM”, see list below). Employees determined to be at risk for exposure must be offered the Hepatitis B vaccine at no charge to the employee and must receive annual Bloodborne Pathogens training. Principal Investigators must determine whether an employee has the potential for exposure without considering the use of personal protective equipment (PPE). Other Potentially Infectious Materials (“OPIM”) Human tissue or organs (unfixed) Human tissue cultures Human blood components Blood, organs or tissue from research animals inoculated with human cell lines, human tissue Blood, organs or tissue from research animals infected with HIV, HBV, HCV or other human pathogens Semen and vaginal secretions Cerebrospinal fluid Pleural and pericardial fluid Peritoneal fluid All body fluids visibly contaminated with blood Check the job classifications in the lab with potential for exposure to human blood/OPIM: X Laboratory and Research Aide X Laboratory and Research Specialist X Laboratory and Research Manager X Post-Doctoral Fellow 27 X X X Professor Research Associate Student (specify) Independent study students, work-study students Other (specify) Check the tasks and procedures performed by the employees listed above in which occupational exposure occurs X Handling and manipulating human blood or OPIM Other (specify) III. Methods Of Compliance Principal Investigators and all staff will comply with the OSHA Bloodborne Pathogens Standard 29 CFR 1910.1030 using the following methods: A. Universal Precautions All human blood and OPIM are considered contaminated with bloodborne and other pathogens. Employees must avoid direct contact with human blood, and OPIM to avoid exposure to bloodborne and other human pathogens. B. Engineering and Work Practice Controls Engineering controls and safe work practices will be used to minimize exposure to human blood, and OPIM. Sharps and other medical devices that incorporate built-in safety features and that have been evaluated and approved by the University of Virginia Health Sciences Center Safety Committee are available from the UVA Hospital Storeroom. Safe work practices are reviewed by the Office of Environmental Health and Safety (OEHS) and the Institutional Biosafety Committee (IBC). 1. Personal protective equipment. If the potential for exposure remains in spite of work practice and engineering controls, personal protective equipment (PPE) must be used. Employers must provide, clean and dispose of PPE at no cost to the employee. PPE must be worn during procedures in which human blood or OPIM exposure to skin, eyes, nose or mouth is reasonably anticipated. PPE must be selected based on the type of exposure anticipated. PPE must cover all body parts and street clothes that may be exposed and must prevent soak through. Gloves, fluid-resistant gowns, face shields, masks, and other types of PPE are available from the UVA Hospital Storeroom. Non-latex gloves are available for employees with latex sensitivity or allergy. PPE and personal clothing must be removed if they become contaminated. Disposable PPE that is contaminated must be discarded in a UVA Regulated Medical Waste Container (CMC). Reusable PPE such as goggles and lab coats that have become contaminated must be placed in a specified container for decontamination and reprocessing. 28 a. Lab coats and gowns. Lab coats or gowns must be worn when working with human blood or OPIM when the potential for exposure exists. All PPE should be removed before leaving the laboratory for non-laboratory areas (office, library cafeteria etc.).Home laundering of lab coats and other PPE is not permitted. Contaminated Laundry must be handled as little as possible and gloves must be worn. Contaminated lab coats or other PPE sent off site for laundering must first be decontaminated by soaking in a 1:10 diluted fresh chlorine bleach solution for 10 minutes or by steam sterilization. b. Gloves. Gloves must be worn when hands may come in contact with human blood, or OPIM, contaminated items or surfaces. Gloves must be worn when handling animals that have been inoculated with human cell lines, human tissue, or infected with HIV, HBV, HCV, or other human pathogens. Gloves must be replaced as soon as feasible if they are torn or contaminated. Disposable (single use) gloves must not be washed or decontaminated for reuse Utility gloves may be decontaminated for reuse, but must be discarded if they are cracking, peeling or show other signs of deterioration. c. Protection for eyes, nose and mouth. Work must be performed in a certified Biological Safety Cabinet or masks and eye protection (goggles or face shields) must be worn whenever splash or spray of human blood, or OPIM to the face is anticipated. 2. Handwashing. Hands must be washed with soap and water after contact with specimens, as soon as possible after removing PPE and whenever they become contaminated with human blood, or OPIM. Antiseptic hand cleaner may be used if soap and water are not available, but hands must be washed with soap and water as soon as feasible. 3. Personal hygiene. Eating, drinking, smoking, applying cosmetics or lip balm, or handling contact lenses in the lab is not permitted. 4. Food. Food and drink must not be stored in labs where human blood or OPIM are present. 5. Pipeting. Mouth pipeting is not permitted. 6. Minimization of aerosols. Splash, spray, spatter, or generation of droplets must be minimized during any procedure that involves human blood, or OPIM. If spattering or the generation of aerosols is reasonably anticipated, work should be performed in a certified Biological Safety Cabinet or eye protection 29 plus a mask or face shield must be worn to prevent an exposure to the mucus membranes of the eyes, nose and mouth. 7. Sharps handling. Bending, recapping or removing needles is prohibited, except under specific infrequent circumstances. If recapping, bending or removing needles or other sharps is required by a specific procedure, and no alternative is feasible then a one handed scoop technique, mechanical device or forceps must be used. Written justification supported by reliable evidence must be included as an addendum to this Exposure Control Plan. This justification must state the basis for the Principal Investigator’s determination that no alternative is feasible and must describe the specific procedure that requires the recapping, bending, or breaking of needles or other sharps. Disposable sharps must be placed in a plastic sharps container as soon after use as possible. Approved sharps containers are available from the UVA Hospital Storeroom. Sharps containers must be easily accessible, with the opening visible, as close as possible to the area where sharps are used and maintained upright during use. Sharps containers must be promptly closed, removed, and replaced when they are ¾ full and placed in a UVA Regulated Medical Waste Container (CMC) prior to transport for disposal. Broken glass must not be picked up with bare hands. Reusable sharps, such as surgical instruments and large bore reusable needles pose the same exposure hazard as disposable sharps and must be handled in a manner similar to disposable sharps until they are reprocessed. The container used for temporary storage of contaminated reusable sharps must be puncture resistant, and labeled as Biohazard. 8. Safe Medical Devices. Safe medical devices are used to prevent percutaneous injuries (examples may include needleless devices, shielded needle devices or plastic capillary tubes). See Appendix B for list of devices available in the UVA Hospital Storeroom. The Principal Investigator is responsible for involving employees in the selection of effective engineering controls and implementing the use of items that would eliminate or minimize exposures. 9. Specimen Transport on Grounds. For transport to sites within the grounds of UVA, specimens of human blood and OPIM must be placed in a secondary leak proof carrier that can contain the contents if the primary container were to leak or break. Carriers must have the biohazard label affixed to the outer surface of the transport container. 10. Servicing contaminated equipment. Before servicing or shipping, contaminated equipment must be decontaminated if possible. If it is not possible to decontaminate equipment, it must be marked with a biohazard label describing what parts remain contaminated. 30 11. Central reprocessing of contaminated reusable equipment. Supplies and equipment returned to a central facility (e.g. department washroom or autoclave room) for decontamination and reprocessing must be put in a plastic bag or closeable container and marked with a biohazard label. 12. Housekeeping. The workplace must be maintained in a clean and sanitary condition. Human blood, or OPIM spills must be cleaned up immediately with a freshly made 1:10 bleach solution or other approved disinfectant using appropriate established spill clean up procedures. Environmental Services is responsible for general cleaning in the majority of areas at the University and maintains written procedures in their office. 13. Equipment and Working Surfaces. Contaminated work surfaces must be disinfected with 1:10 freshly made dilution of bleach or an alternative approved disinfectant. The decontamination of work surfaces must be done as soon as possible when contaminated with human blood, or OPIM, after completing procedures or at the end of the work shift if the surface may have become contaminated since the last cleaning. Temporary coverings (plastic backed paper, chux, plastic wrap, foil, etc.) over bench tops, equipment and other surfaces must be removed and replaced as soon as possible when contaminated or at the end of the work shift if the surface may have become contaminated since the last cleaning. All reusable bins, pails, cans, and similar receptacles which may become contaminated must be regularly inspected and decontaminated as soon as possible if they become contaminated. 14. Regulated Medical Waste. Regulated Medical Waste is disposed of by UVA in accordance with the Virginia Department of Waste Management Regulations. See the section 5 of the Biosafety Manual for guidance. IV. Communication of Hazards to Employees 1. Labels. Biohazard warning labels must be affixed to refrigerators, freezers, incubators and other vessels used for storing human blood, or OPIM. Containers used for transporting human specimens beyond the immediate work area must have the biohazard label affixed to the outer surface of the transport container. Biohazard labels are required on areas and equipment reasonably anticipated to be contaminated with human blood, or OPIM 31 Biohazard labels are not required on individual specimens that are transported inside a carrier within the University or on Regulated Medical Waste that has been decontaminated by steam sterilization. V. Hepatitis B Vaccination Policy Employees identified as having potential for exposure to human blood or OPIM (see II. Exposure Determination), must be offered the Hepatitis B vaccine at no charge to the employee. The vaccination is a series of three injections given at approximately 0, 1 and 6 months. A routine booster dose is not recommended, but will be given at no charge if the U. S. Public Health Service recommends it in the future. The vaccine must be offered within 10 working days of initial assignment to a job category where exposure may occur. Employees who decline the Hepatitis B vaccine must sign a statement of declination (page 10). Principal Investigators must keep a copy of the declination statement on file. Vl. Procedures for Exposure Incidents. An exposure is defined as: blood or OPIM contact with broken skin, eyes, nose, mouth, other mucous membranes, a percutaneous injury with a contaminated sharp, or contact with blood or OPIM over a large area of apparently intact skin In the event of exposure: 1. Wash the area with soap and water or flush eyes, nose or mouth with large amounts of water for 15 minutes 2. Staff must report immediately to UVA-WorkMed (formerly Occupational Health) or Employee Health 8am-4:30pm Monday-Friday, or to the Emergency Room after hours. Students must report to the Student Health Center 8am-5pm Monday-Friday or to the Emergency Room after hours. 3. All exposures must be reported to the immediate supervisor and Principal Investigator. 4. Principal Investigators are responsible for reporting exposure incidents to the Institutional Biosafety Committee. 32 A. Evaluation and Treatment of Exposures The evaluation and treatment of an exposure is confidential and will be given by or under the supervision of a licensed physician and will follow an established protocol in compliance with OSHA standard 29 CFR 1910.1030, U.S. Public Health Service, CDC guidelines, and Virginia state law. Evaluation and treatment of exposures are managed by UVAWorkMed, UVA Employee Health or Student Health Services. If the infectivity status of the source individual is unknown and blood is available, it will be tested for HIV, hepatitis B and C in accordance with state law. The exposed employee will be told what the test results are and what they mean. If the employee consents, his or her blood will be tested as soon as possible after exposure to provide baseline hepatitis B, C and HIV status. If the employee does not consent to HIV testing, the sample will be stored for 90 days and tested if the employee consents in that time period. Post-exposure prophylaxis will be offered to exposed employees when medically indicated and as recommended by the US Public Health Service. Counseling and medical evaluation will be offered for any reported illnesses the employee develops as a result of the exposure. B. Documentation of Circumstances Documentation of the circumstances surrounding the exposure incident is required and allows for the identification and correction of occupational hazards. Exposure incidents will be investigated by the Office of Environmental Health and Safety in cooperation with UVAWorkMed. VIl. Employee Training All employees who may have the potential for occupational exposure to human blood, or OPIM must attend a Bloodborne Pathogens training session at the time of their initial assignment to tasks where occupational exposure may take place and annually thereafter. Annual retraining is completed via the UVA OEHS web based training system, or by other OEHS sponsored training programs. Additional training must be provided whenever there are changes in tasks or procedures which affect employees' potential for exposure. 33 VIlI. Recordkeeping Procedures A. Medical Recordkeeping UVA-WorkMed will establish a medical record for employees who have exposures. The record will be maintained for the duration of employment plus 30 years. The record is confidential and will not be disclosed to anybody within or outside the workplace without the employee’s written consent, except as required by law or regulation. The record will include: employee name and social security number; dates of hepatitis B vaccinations and medical records relative to the employee's ability to receive vaccination; examination results, medical testing, and follow-up procedures; the healthcare professional's written opinion; information provided to the healthcare professional who evaluated the employee for suitability to receive hepatitis B vaccination. B. Training Records The Office of Environmental Health and Safety’s web based training system will track all employees who complete Bloodborne pathogen training. Employees can access their records through the web based training system. Records will be maintained for at least 3 years. Employees, employee representatives, the Commissioner of the Virginia Department of Labor and Industry and other appropriate agencies may also request copies of these records. 34 IX. Hepatitis B Vaccination Employees identified as having potential for exposure to human blood or other Human-derived materials (see ECP II. Exposure Determination) must be offered the Hepatitis B vaccine at no charge to the employee. Employees who decline the Hepatitis B vaccine must sign a statement of declination. Principal Investigators must keep a copy of the declination statement on file See scanned document, page 4. Name Signature Date HepB vaccine Yes or Decline* *Hepatitis B Vaccine Declination I understand that due to my occupational exposure to blood or other potentially infectious materials I may be at risk of acquiring hepatitis B virus (HBV) infection. I have been given the opportunity to be vaccinated with hepatitis B vaccine, at no charge to myself. However, I decline hepatitis B vaccination at this time. I understand that by declining this vaccine I continue to be at risk of acquiring hepatitis B, a serious disease. If in the future I continue to have occupational exposure to blood or other potentially infectious materials and I want to be vaccinated with hepatitis B vaccine, I can receive the vaccination series at no charge to me. 35 X. Medical Center Storeroom Safety Products (2004) (This list is updated several times per year as a result of changes in safety items that are available in the UVA store room. Contact Materials Management if you would like a current list) Description of item Bin # Catheters Catheter IV Safety 14G 1 ¼ IN Catheter IV Safety 16G 1 ¼ IN Catheter IV Safety 18G 1 ¼ IN Catheter IV Safety 20G 1 IN Catheter IV Safety 20G 1 ¼ IN Catheter IV Safety 22G 1 IN Catheter IV Safety 24G ¾ IN 97045 97046 97047 97048 97049 97050 91827 Safety needles Needle Safety Hypo 19GX1.5IN Needle Safety Hypo 20GX1.5 IN Needle Safety Hypo 20GX1IN Needle Safety Hypo 21GX1.5IN Needle Safety Hypo 23GX1IN Needle Safety Hypo 25GX5/8IN 91966 91967 91968 91969 91970 91971 Winged Needles Needle Wing Safety 19Gx7/8 12 Needle Wing Safety 21Gx3/4 3.5 Needle Wing Safety 21Gx3/4 12 Needle Wing Safety 23Gx3/4 12 Needle Wing Safety 23Gx3/4 3.5 Needle Wing Safety 25Gx3/4 3.5 Needle Wing Safety 27Gx3/8 12 92877 92878 92873 92876 92870 92871 92872 Blood Glucose Lancet Safe-T-Stix Lancets 94002 Safety Syringes Syringe 10CC 20G Syringe 3CC 21G 1.5 IN Syringe 3CC 22G 1 IN Syringe 3CC 23G 1 IN Syringe 3CC 25G 5/8 IN Syringe Safety 3CC w/o needle Syringe TB 25G 5/8IN Syringe 3CC w/ vial access cannula Syringe 10CC w/vial access cannula 90725 90727 90729 90731 90733 97057 90735 92150 92151 36 IV tubing/extension sets/adapters Adapter Luer Slip 96332 Catheter IV Extension set 96340 Catheter Ext Set Y type 1 valve 96342 Filter Straw 96326 Needle Lock Device 18G 97063 Needleless Injection Cap 97051 Sampling site coupler 96933 Syringe Saline Prefilled 3 cc 96338 Syringe Saline Prefilled 10cc 96345 Tubing IV end cap 91441 Tubing IVAC Pump Primary 93271 Tubing IVAC Pump Blood Set 93274 Tubing IVAC Pump Burette 93271 Tubing IVAC Pump Low Sorbing 99415 Tubing IVAC Pump w/Filter 99416 Tubing Injection Cap 92507 adapt a valve to use with a sharp when appropriate Tubing Extension Set hi pressure 92875 Tubing IV 2 site 15 drops/ml 93841 Tubing IV 1 site 15 drops/ml 93843 Tubing IV Ext 43IN w/2 Y Inj sites 93844 Tubing IV 3 sites 60 drops/ml 93848 Tubing IV 3 sites 15 drops/ml 93999 Tubing IV Adaptor Vent for unvent bot 99224 Vacutainer Blood Collection Devices: Plastic Tubes: 3ML Li Heparin PST Green 4ML NaFl K Oxylate Gray 3.5ML SST Gold Tiger 3ML Lavender 7ML Pink Blood Bank 93456 92496 92495 92500 98803 Holder: Needle Holder Safety 92504 Safety Winged Sets: Set Safe Lok Blood Collection 21G Set Safe Lok Blood Collection 23G Set Safe Lok Blood Collection 25G 92477 92478 92479 Transfer Devices Vacutainer syringe blood transfer device 90020 Blood Culture Transfer set 96360 Vacutainer IV Tube Holder 94299 Kits Contact supply room for most current safety kits available. 37 Appendix B Toxin Safety Plan l. Biotoxin Safety Plan All Investigators working with toxins of biological origin must complete a laboratory specific Toxin Safety Plan that includes: toxins used ,know hazards, safety equipment and protocols, personal protective equipment and training requirements, toxin inactivation and disposal, inventory control and security measures and emergency procedures (spills, exposure management) Guidelines for working with toxins of biological origin can be found in Appendix I of the CDC/NIH Publication Biosafety in Microbiological and Biomedical Laboratories and the Toxin Inactivation document that follows. 1. Toxins Used, Total Quantity (maximum amount possessed by Principal investigator at UVA.) No toxins used in J.T. Parsons laboratory. 2. Known Hazards (attach MSDS if available) N/A 3. Safety Equipment, Procedures, PPE and Training requirements: N/A 4 Toxin inactivation and Disposal Procedure N/A 5. Inventory Control and Security Procedures: N/A 6. Spill Clean-up and Exposure Management N/A