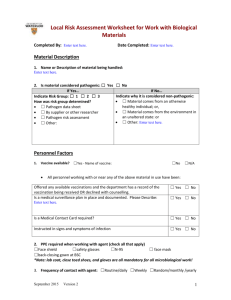
Generally applicable precautions
advertisement
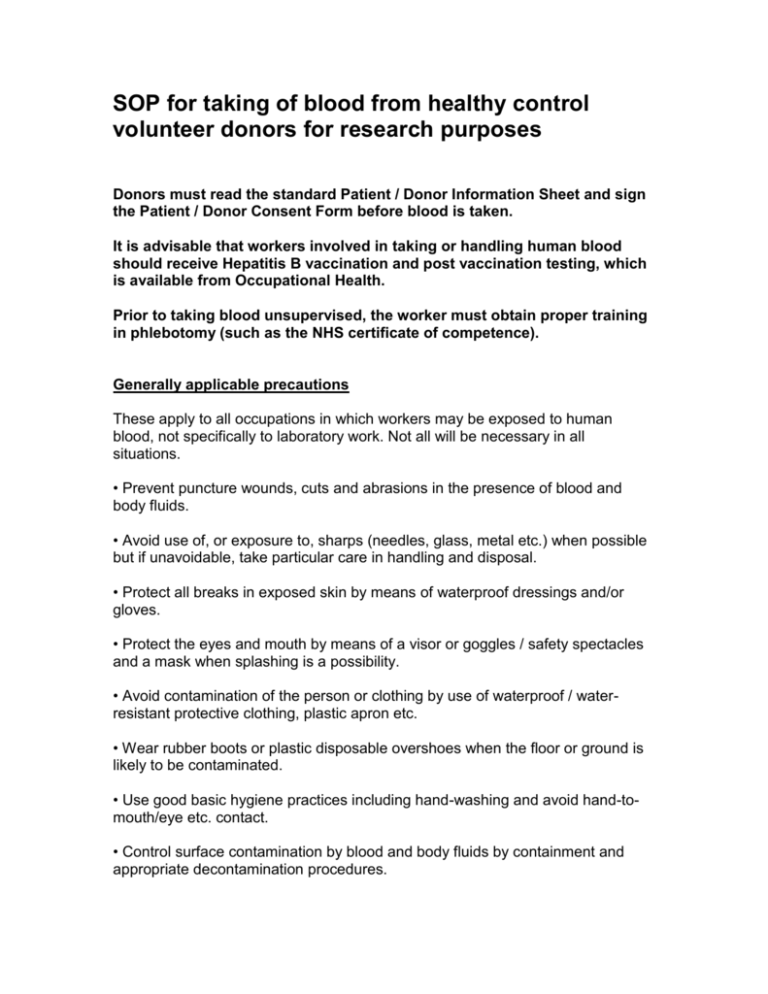
SOP for taking of blood from healthy control volunteer donors for research purposes Donors must read the standard Patient / Donor Information Sheet and sign the Patient / Donor Consent Form before blood is taken. It is advisable that workers involved in taking or handling human blood should receive Hepatitis B vaccination and post vaccination testing, which is available from Occupational Health. Prior to taking blood unsupervised, the worker must obtain proper training in phlebotomy (such as the NHS certificate of competence). Generally applicable precautions These apply to all occupations in which workers may be exposed to human blood, not specifically to laboratory work. Not all will be necessary in all situations. • Prevent puncture wounds, cuts and abrasions in the presence of blood and body fluids. • Avoid use of, or exposure to, sharps (needles, glass, metal etc.) when possible but if unavoidable, take particular care in handling and disposal. • Protect all breaks in exposed skin by means of waterproof dressings and/or gloves. • Protect the eyes and mouth by means of a visor or goggles / safety spectacles and a mask when splashing is a possibility. • Avoid contamination of the person or clothing by use of waterproof / waterresistant protective clothing, plastic apron etc. • Wear rubber boots or plastic disposable overshoes when the floor or ground is likely to be contaminated. • Use good basic hygiene practices including hand-washing and avoid hand-tomouth/eye etc. contact. • Control surface contamination by blood and body fluids by containment and appropriate decontamination procedures. Control surface contamination by blood and body fluids by containment and appropriate decontamination procedures. • Dispose of all contaminated waste safely: Contaminated sharps (eg needle used to take blood, if used): Approved bin for disposal of contaminated sharps, for disposal by incineration Blood, associated waste, and cells derived from blood: Large Yellow Clinical Waste bin, for disposal by incineration Taking specimens of human blood a. Hand washing facilities should be available. The area should be easy to decontaminate after any spillage. b. Venous blood must only be taken by people properly trained in phlebotomy, and authorised. A clean laboratory coat should be worn. Gloves must be used when taking blood. c. Blood must not be taken from persons suspected of having Hazard Group 3 infections or people from groups with a high risk of hepatitis B virus or HIV infection unless under medical supervision. The Safety Services Office must be informed of any work likely to involve blood from such individuals. d. Before taking blood, disinfect the patient’s skin, e.g. with a Medi-Swab which contains 70% v/v isopropyl alcohol. e. Procedures designed to minimise needle-stick injury MUST be followed. Used needles must not be re-sheathed, but discarded immediately into sharps containers for disposal. The use of Spencer-Wells or other suitable clamps is recommended for detaching needles from syringes (i.e. not fingers). f. Using a vacuum collection tube is safer than using a syringe and needle, as the blood does not have to be expelled into a separate container and the outside of the tube cannot be contaminated in the same way as traditional collecting tubes. g. After taking blood, staunch bleeding completely and cover the wound with a waterproof dressing. h. Spilt blood must be mopped up immediately and the area disinfected. Disinfectant should be poured on to the area of spillage, paper towels added and the area left for at least ten minutes before mopping up. The areas should again be cleaned thoroughly with disinfectant. i. Hands should be thoroughly washed after taking blood. NOTE: All blood and blood products must be handled under appropriate containment conditions, typically within a class II cabinet. Accidents with blood or body fluid preparations Accidental wounds caused by contaminated sharps must be dealt with at once: • wash off splashes on skin with soap and water; • encourage bleeding if the skin has been broken; • wash out splashes in the eye preferably using eye wash from a fresh eye-wash bottle (alternatively tap water), or nose or mouth with copious amounts of tap water; • record source of contamination (name/type of fluid/type of injury); • report the incident to the person in charge of the work and the Departmental Safety Officer. Advice must be sought promptly from the Freemen’s Common Health Centre, or alternatively members of University staff working in NHS hospitals may attend the hospital’s Accident and Emergency Unit. Outside normal working hours, and at Bank Holidays or weekends, contact the nearest hospital’s Accident and Emergency Unit. Note that working alone, especially out of normal working hours, with hazardous substances will require risk assessment (ref. 25.) • ensure that the Safety Services Office is informed promptly and that an accident report form is sent. • In the laboratory, every effort should be made to identify the specimen or other material concerned in the exposure, which, if blood serum or plasma, must be retained against any need to test for HIV or HBV infection.