PATENT from King Saud University
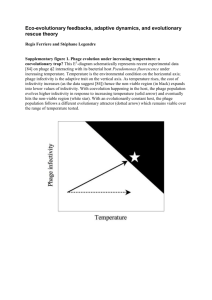
advertisement

King Saud University Faculty of Science Department of Botany and Microbiology The Role of Staphages in The Treatment of Methecillin Resistant Staphylococcus aureus Infection By: Eman Kamel Al-Digs Submitted in partial fulfillment of the requirements for the Doctor of Philosophy Degree in the Department of Botany and Microbiology at the Faculty of Science, King Saud University Supervised By: Dr. Nagwa Mohamed Amin Aref 1425-2004 الحمد هلل رب العالمين To My Family… To My Friends… Thank you for all what you did for me, it means so much أتقدم بالشكر لمدينة الملك عبد العزيز للعلوم والتقنية لدعمها لهذا البحث بمنحة رقم أ ط – 77 - 8 ACKNOWLEDGMENTS The author wishes to express her sincere appreciation to many people who made this endeavor possible. Acknowledgment is due to King Saud University and King Abduaziz University for support of this research. Very special thanks to Dr. Nagwa Aref , Prof. of Virology and my major prof. at the Department of Botany and Microbiology , Faculty of Science , King Saud University for her supervision ,advise , and guidance for this investigation. I would like to thank Dr. M. Hussein for supervision in this work. I would like also to acknowledge Dr. A. Al- Farhan for his understanding, guidance and support. Very sincere thanks go to Dr. M. Al-Ahdal, Dr. S. Althawadi, and G. Kessie; King Faisal Speciallist Hospital and Research Center. Dr. B. Taj, National Guard Hospital; for their helpful discussion, encouragement and providing all necessary facilities and materials. My appreciation goes to all staff members of the department of Botany and Microbiology, Faculty of Science, King Saud University; for their great help and guidance, especially Dr. A. Abu-Taleb. My appreciation is also extended to all hospitals and polyclinics who cooperated in this study, especially Dr. A. Saraweq; King Fahd General Hospital / Jeddah. A special pray for my father who supported me in every step in this work until it is here I shall be for ever grateful to him. To all those who have assisted in this work “THANK YOU VERY MUCH“. Introduction ii Introduction The Staphylococci are ubiquitous colonizers of human, animal skin and mucous membranes causing a variety of syndromes. Staphylococcus aureus is considered the most pathogenic organism. The wide spread of antibiotic resistance among strains of S. aureus is a major concern in the treatment of Staphylococcus infections. It is well known that the organism acquires resistance soon after the introduction of new antibiotics (Lyon and Skurray, 1987). As the incidence of antimicrobial resistance rises, so do costs associated with its consequences. According to estimates, the cost of resistance ranges from $75 million to $ 7.5 billion per year. One study by the Centers for Disease Control and Prevention (CDC) concluded that for both nosocomial and community-acquired infections, those involving drug-resistant strains were at least twice as likely to be associated with morbidity, hospitalization, and increased length of hospital stay as those with drug-susceptible strains. Although it can only be roughly quantities, antimicrobial resistance clearly is an important health problem and an economic burden to society. Methecillin was developed in 1960 for the treatment of such multidrug resistant S. aureus. However in the same year, Jevons (1960) discovered Methecillin Resistant S. aureus (MRSA), which by 1970s iii became spread all over the world; but remained uncommon until 1986 when a marked increase occurred in the number of isolates referred to the Communicable Disease Group Institute of Environmental Science and Research at Porirua (Rajan et al., 2002; and Ito et al., 2003). In Jeddah during 1993 – 1994 Al -Aamodi (1997) found 40.4 % of the S. aureus isolates was MRSA. In the other hand Al -Shammary (1997), in Riyadh revealed 7.2 % MRSA infections from five different hospitals. While the most frequently isolated pathogen from chronic otitis media swabs was 36% S. aureus in the study of Al- farraj (2002) in Riyadh. Bacteria resistant to most or all available antibiotics are causing increasingly serious problems, raising widespread fears of returning to a preantibiotic era of untreatable infections and epidemics. There was a renewed interest in the possibilities of bacteriophage therapy, where a specific kind of viruses that attack only bacteria used to kill the pathogenic microorganisms (Levin and Bull, 1996; Lederberg, 1996; Radetsky, 1996; Barrow and Soothhill, 1997). Phages are efficacious antibacterial agents due to the lethality and specifity of phages for particular bacteria. The ability to replicate within infected animal hosts, and the boi-safety of phages made them efficacious antibacterial agents. It is likely appeared that phage therapy would regain a iv role in both medical and veterinary treatment of infectious diseases (Duckworth et al., 2002). The concept of bacteriophage therapy is simple; bacteriophages are administrated to the infected animals or humans in an effort to reduce populations of pathogenic bacteria through the natural ability of phage to target and destroy bacterial cells. Although bacteriophages had not been extensively used as antimicrobial agents since the emergence of antibiotics, the rise of multiple antibiotic resistant strains had a renewed interest in phage therapy (Platt et al .,2003). In making the choice to explore the possibilities of phage therapy, it should also considered their many potential advantages: 1. They are both self-replicating and selflimiting, since they will multiply only as long as sensitive bacteria are present and then are gradually eliminated from the individual and the environment. 2. They can be targeted far more specifically than can most antibiotics to the specific problem bacteria, causing much less damage to the normal microbial balance in the body. The bacterial imbalance or "dysbiosis" caused by treatment with many antibiotics can lead to serious secondary infections involving relatively resistant bacteria, often extending hospitalization time, expense and mortality. 3. Phages can possibly be targeted to receptors on the bacterial surface which are involved in pathogenesis, so that any resistant mutants are attenuated in virulence. 4. Few side effects have been reported for phage therapy. 5. Phage therapy v would be particularly useful for people with allergies to antibiotics. 6. Appropriately selected phages can easily be used prophylactically to help prevent bacterial disease in people or animals at times of exposure, or to v sanitize hospitals and help protect against hospital-acquired (nosocomial) infections. 7. Especially for external applications, phages can be prepared fairly inexpensively and locally, facilitating their potential applications to underserved populations. 8. Phage can be used either independently or in conjunction with other antibiotics to help reduce the development of bacterial resistance. 9. For localized uses, phage has the special advantage that they continue multiplying and penetrating deeper as long as the infection is present, rather than decreasing rapidly in concentration below the surface like antibiotics. This work was preformed in tow categories, First: identification of S. aureus samples which were collected from different microbiology labs in Riyadh hospitals to determine their susceptibility to antibiotics, then identifying the isolates with phage typing and molecular typing by pulsed field gel electrophoresis. Second: Characterization of new phages that were isolated by induction with ultra violet radiation to study their plaque morphology, spectrum of infectivity, use of electron microscopy to examine the morphology of isolated phages and identification the nature of the phages nucleic acid by enzyme digestion and pulsed field gel electrophoresis. As such, the objectives of the present study were in to: I. Monitoring the susceptibility of the collected studied isolates of S. aureus vi to different antibiotics. II. Identifying the investigated S. aureus isolates with standard International Phages Set (IPS), (Phage Typing). III. Molecular typing for S. aureus for the more identification of the nontypable isolates after typing with the IPS. IV. Induction of new phages from Saudi local S. aureus isolates, with ultra violet radiation. V. Isolation of temperate and virulent phages after induction according to their effect on different S. aureus strains. VI. Analyze the spectrum of the isolated phages infectivity for S. aureus isolates. VII. Provide morphological and molecular characteristics of the new induced S. aureus phages. VIII. Provide base line data for application of phage therapy for the first time in Saudi Arabia and Middle East, to evaluate the efficacy of phage therapy in medical cases of methecillin resistant S. aureus skin infection in patients of wounds (surgical and accidental), diabetic foot infections, burn and abscess cases since MRSA is one of the most resistant organisms for antibiotics. Abstract Abstract Over a period of one year (from February 2000 to may 2001) 173 Staphylococcus aureus isolates collected from microbiology lab hospitals in Riyadh and Jeddah. Distribution of Methecillin Resistant Staphylococcus aureus (MRSA) isolates among clinical departments and isolations from different specimens, showed that the wound infections resemble the highest percentage of the clinical sites (26%). The all over percentage of MRSA topical infections (70%) was higher than MSSA infections. All isolates were sensitive to vancomycin which is the drug of choice for MRSA infections. Mupirocin showed low degree of resistance, which was 6%. Susceptibility to other commonly used antibiotics was variable. Resistance oxacillin was the highest 34%. Some degrees of resistance to sulphomethoxazole / trimethoprim and fusidic acid (34%) were noticed. Terms like boarder line resistant, low-level mutation, and boarder- line susceptible had also been obtained in our studied isolates of S. aureus for methecillin using Minimum Inhibitory Concentration test; which was observed in the percentage of MRSA isolates in our data that had MICs of 256µg/m1 (30.83%). Studying the distribution of phage type patterns among Staphylococcus patients isolates in Saudi cohort; it was found that only 30.56% were typable with different degree, and 69.7% were non typable. Differentiation increased in the phage typing, and genome typing yielding 20 and 23 different S.aureus types, respectively. A 61.71% of the MRSA isolates were genetically typed by PFGE resulting one type of MRSA with one genetic difference. Genome typing by PFGE was a powerful tool not only for strain identification but also for the resolution of clonal relationships of S. aureus strains. Observation on UV induction of a S.aureus strains showed that the number of infective centers increased by more than 100%. As seen in our electron micrographs, our studied phages designated from ph1 to ph10; five of these phages ph2, ph4, ph5, ph7, and ph10 were morphotype A, present in Myoviredae group, their DNAs were in the range 43.6kb-48.5kb that is very close to this size range with minor differences in phage strain. Ph9 and ph10; had more than one band in their pattern. A mixture of ten phages differed in their virulence to MRSA isolates were used with all patient isolates (30) that were lysed completely by spot-test. Phage therapy for 30 patients of MRSA in different skin infection cases, showed that phage therapy were highly effective. Using a mixture of 10 phages daily (7-10 days), treatment gave us a close success rate of 90%. Table of Contents Page # I. II. Introduction. Review of Literature Antibiotic Resistance -The over prescribing of antibiotics 7 - Emergence of multiresistant S. aureus 9 - The importance of MRSA 12 Phage typing 15 - Requirements of a typing method 15 - Phage typing of S. aureus. 17 - S. aureus epidemic types 19 - Staphylococcus carrier state. 21 - Selection of typing phages. 22 Molecular typing by pulsed field gel electrophoresis. Induction in lysogenic S. aureus. - Bacteriophage plaque morphology. 23 27 30 Electron microscopy of staphages 32 -Classification and frequency in staphages. Characterization of phage nucleic acid. 35 Phage therapy. - Historical aspects of phage therapy. 38 - Specific problems in early phage therapy work. 40 - Properties of phages subjected to therapy. - Bacteriophages as antibacterial agents. 42 - Applying phage therapy in humans world wide. III. 43 1. Polish academy of Sciences, Worslaw. 43 2. Soviet Research on phage therapy. 50 3. British work. 54 4. French company L`Oreal. 56 5. U.S.A work. 56 MATERIAL and METHEODS : 1. Sample collection and Bacterial Isolation. 62 a. Identification of S. aureus Sample. 62 1..2 Pure bacterial cultures for propagation. 1..3 Glycerol cultures for preservation. 63 b. Antibiotic susceptibility tests: 2.1. Disc diffusion method. 2.2. Minimum Inhibitory Concentrations (MICs) 2.3. Detection of MRSA homogenicity / Heterogenicity. 64 64 3. Typing the Staphylococcus aureus isolates: 3.1. Phage typing for the 69 MRSA isolates 3.2. Molecular typing by Pulsed Field Gel 3.3. 63 65 65 electrophoresis. 66 3.3.1. Selection of bacterial isolates. 67 3.3.2. Preparation of agarose embedded 3.3.3. bacteria. 3.3.4. Lysis step. 68 3.3.5. Proteolysis step. 68 3.3.6. Restriction digestion step. 68 3.3.7. Preparation of 1% agarose gel. 69 3.3.8. Casting the gel. 69 3.3.9. Electrophoresis conditions. 69 4. Isolation of new Staphylococcus phages. 4.1. 67 Detection of lysogeny by cross – culture. 70 70 4.2. Isolation of phages from sewage samples. 70 4.3. Ultra-Violet induction of lysogenic S.aureus. 71 4.3.1. Induction on plate. 71 4.3.2. Induction on broth. 71 5. Phage propagation. 5.1. 72 Selection of sensitive S. aureus strain to 5.2. studied phages for propagation. 72 5.3. Propagation on cultures of agar plates. 72 5.4. Propagation on broth cultures. 73 5.5. Routine Test Dilution (RTD). 73 5.6. Phage preservation. 74 5.7. Spectrum of isolated phage infectivity. 74 6. S. aureus phages characterization. 74 6.1. Precipitation of the phage by Poly Ethylene Glycol. 74 6.2. Electron Microscopy examination. 75 6.3. Characterization of phage Nucleic acid by Agarose 75 Gel Electrophoresis 8.1. Isolation of phage DNA for PFGE. 75 8.2. Electrophoresis conditions. 75 9. Phage Therapy. 9.1. Evaluation of phage efficacy for phage therapy In vitro. 76 9.1.1. Preliminary phage concentration 76 9.1.2. Phage stock. 77 9.1.3 Preparation of phage dressing. 77 9.2. In vivo phage dressing therapy. IV. 9.2.1 Skin infection cases. 77 9.2.2. Clinical Application of phage 78 dressing therapy. 78 RESULTS: a. Staphylococcus isolates. 1.1. 2. 81 S. aureus identification. 81 Antibiotic susceptibility test. 81 MRSA screening. 81 1.2. Disc diffusion method. 89 1.3. Minimum inhibitory concentrations (MICs). 89 1.4. MRSA homogenicity / hterogenicity. 99 3.1. Phage typing. 99 3.2. PFGE. 102 4.2. Phage isolates from sewage samples. 106 4.3.1. Induction on plate. 109 4.3.2. Induction on broth. 109 5.6. Spectrum of isolated phages infectivity. 116 7. Electron Microscopy. 118 8. Phages Nucleic Acid. 130 9.1 Phage therapy in vitro. 133 9.2. Phage therapy in vivo 136 I. Staphage therapy for MRSA in diabetic foot cases. 136 II. Staphage therapy for MRSA in post-operative infections. 138 III. Staphage therapy for MRSA in accedintal septic wound Infections. 146 IV. Staphage therapy for MRSA in abscess cases. 150 V. Staphage therapy for MRSA in burn cases. 150 IV. DISCUSSION. 155 V. Appendix I . Appendix II . VI. Refrences. Arabic summary. List of Figures List of Tables Table# 2 Page# Numbers of S. aureus isolates from each clinically infected site and thedistribution of 173 S. aureus isolates on different clinical site. 71 3 Antibiogram of S. aureus to all testedantibiotics. 76 4 S. aureus Methecillin MICs . 78 5 A comparison between criteria of local MRSA solated Antibiogram typing phage typing and molecular typing. 87 6 Morphological Charecteristics of staphages. 101 7 Chracterization of Staphages induced from local Isolates DNA size, Morphology, plaques, Range of activity, bacterial isolate site, typing and induction. 8 104 Staphage therapy in MRSA diabitic foot infection cases Staphage therapy for MRSA in Post operative infection cases. 115 9 Staphage therapy for MRSA in accidental septic Wound infection cases. 118 10 Staphage therapy for MRSA in abscess cases. 120 11 121 Staphage therapy for MRSA in burn cases.