DNA Vaccines Short Review
advertisement

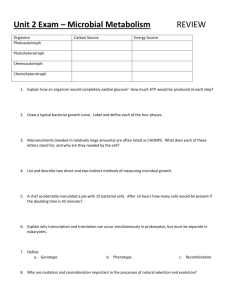
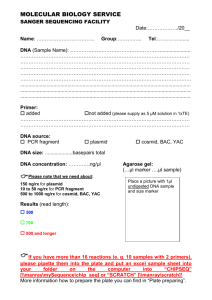
DNA Vaccines: A short little review Julie Smith 2007 Vaccines constitute one of the greatest achievements of modern medicine. They have virtually eradicated smallpox and polio, and significantly reduced the number of occurrences of typhus, measles, tetanus, and other dangerous infections within the world population. However, successful vaccines have yet to be introduced for many other deadly and debilitating disorders including malaria, hepatitis C and AIDS. Unfortunately, standard immunization methods work poorly or pose unacceptable risks when targeted against certain illnesses. Clearly, alternate strategies are needed. One of the most promising creates vaccines out of DNA. In the past 15 years such vaccines have progressed from a laughable idea to being one of the hottest research areas in vaccinology. In order to understand the benefits of DNA vaccines, the actions of traditional vaccines need to be understood. Traditionally, vaccine preparations consist primarily of killed or weakened pathogens. They are designed to prime the immune system to attack dangerous invaders quickly, before the detrimental organism can gain a foothold in the body. Vaccines accomplish this by tricking the body into believing that it has been infected with the microorganism and that the microorganism is multiplying unchecked and raising havoc with the host. In the bodies attempt to protect itself and ward off the invaders, an autonomic series of events occur. The immune system homes in on foreign antigens that are uniquely produced by the invading organism. These antigens are usually specific proteins or protein fragments. The immune system than mounts a double fronted battle plan against the invaders. The humoral front, led by the B lymphocytes, attacks the pathogens that are outside the cell. These B cells secrete antibodies that latch onto the invaders and either neutralize them or tag them for destruction by other parts of the immune system. The cellular front, led by cytotoxic T lymphocytes, eradicates invaders that are inside the cell. Infected cells display pieces of the invaders protein on the cell surface that act as a flag for the cytotoxic T lymphocytes. When the cytotoxic T lymphocytes identify a flagged cell, they often destroy the cell and the invaders within. Once the immune system is activated, it leads to the creation of memory cells that can lay in wait until the same pathogen attacks again. The hosts immune system is ready to spring in to action should the invader return. Vaccines confer protection by similarly inducing immune responses and the formation of memory cells. Unfortunately, standard vaccines vary in the type of protection that they provide. The vaccines that are based on killed pathogens, such as Salk polio vaccine or antigens isolated from disease-causing agents, such as hepatitis B subunits, cannot make their way inside the cell. Therefore, they cannot activate the hemoral front and do not activate killer T cells. This obviously works for some diseases; unfortunately this type of vaccination is ineffective against organisms that invade cells. Attenuated live vaccines, usually viruses, do enter the cell and make antigens that are displayed by the inoculated cells. Thus, they flag the cell for attack by killer T cells as well as by antibodies. This dual edged attack is essential for blocking future infections by the virus. Based on the fact that attenuated vaccines activate both arms of the immune response, they have long been considered the gold standard in vaccinology. However, live vaccines, even if they are attenuated, can be problematic in their own way. They can fail to provide effective protection or they can cause a full blown illness in individuals that may be immune compromised. Additionally, weakened viruses can, at times, mutate in ways that restore virulence. For some diseases, the risk of reversion to virulence is unacceptable. There are a number of vectors currently being used for genetic vaccine research (Figure 1). The structure and function of these genetic vaccines are quite different from traditional ones. One of the most studied consists of plasmids – small rings of doublestranded DNA- derived from bacterial. Plasmids used for immunization are altered to carry genes specifying one or more antigenic protein that would normally be made by the selected pathogen. At the same time, they lack any of the genes required by a pathogen for self- replication which can lead to infection. The antigenic proteins can elicit humoral immunity when they escape from the cell and they can elicit cellular immunity when they are displayed on the cell surface. DNA vaccines emerged as a fluke (Brown, 1996). In a 1990 experiment, Wolff and associates injected a control group of mice with “naked” viral DNA. Unexpectedly, the control mice began producing significant amounts of viral protein. Thus, the field of DNA vaccines was born. Further research was conducted and it was reported that a DNA vaccine could indeed prevent influenza infection in mice (Ulmer et al, 1993). Wang and his colleagues with the Naval Medical Research Institute in Bethesda, Maryland reported in 1998 that injections of plasmid DNA encoding for a protein from malaria parasite provoked a strong immune response in humans. Genetically modified DNA vaccines are being explored against an number of diseases such as: cancer (Lowe et al, 2006, Haupt et al, 2002), tuberculosis (Bhattacharya , 2005), influenza (Drape et al, 2006), mycoplasma (Barry et al, 2002), AIDS (Barouch et al, 2002), Ebola (Vanderzanden et al, 1998) just to name a few. The first license for the commercial use of a DNA vaccine in the United States was granted in July of 2005 to Fort Dodge Laboratories. The product licensed was vaccine against West Nile virus for horses (CIDRAP, 2005). DNA vaccines have also successfully been administered to endangered California Condors to protect them against West Nile Virus (Gunderson, 2005). At nearly the same time Canada, based on research by Traxler (1999) and associates, licensed a DNA vaccine developed to prevent infectious hematopoietic necrosis virus in the commercially farmed Pacific salmon population. DNA vaccines offer many advantages over traditional vaccines (McDonnell and Askari, 1996). DNA is very amenable to manipulation and it is relatively easy to insert the desired gene(s) into the plasmid. Due to the nature of plasmids, researchers are not limited to just a single pathogen, as is the case with traditional vaccines. Plasmids have the capability of holding multiple genes for multiple pathogens (Forde, 2005). DNA vaccines are beneficial in that they encode only for a few specifically selected antigen(s) thus completely eliminating the possibility of mutation to its original virulent form. Another advantage is that DNA vaccines may be able to outsmart ever changing viruses. Designing DNA vaccines that code for non-mutating proteins within a virus, may provide immunity for multiple mutated strains of a virus. DNA vaccines are more economical and easier to produce than previous forms of vaccinations (Guilherme et al, 2000). The stability of DNA vaccines makes them very advantageous. They do not require a coldchain. Cold-chain refers to the refrigerators required to maintain the viability of traditional vaccine during its distribution. Currently, 80% of the cost of providing vaccinations in developing countries is due to the need for refrigeration. DNA vaccines can be stored either dry or in an aqueous solution at room temperature, so there is no need for the cold-chain. This dramatically increases the ability of providing vaccinations in remote areas where refrigeration is not available (Rangarajan, 2002). The variety in the modes of administration lends itself to the diversity of potential vaccines. Researchers are not limited to the traditional modes of administering vaccines (Gurunathan et al, 2000). DNA vaccines can be administered via a variety of routes: injection (Fynan et al, 1993), epidermal delivery by scarification ((Raz et al, 1994), oral (Niethammer et al, 2001), intranasal (Oh et al, 2001), vaginal (Livingston et al, 1997), electroporation (Heller, 2003) and biolistic vaccination to the skin (Schmaljohn, 2006). With the proliferation of potential DNA vaccines came concerns over the safety associated with the introduction of foreign DNA into a host. One of the issues raised was the potential integration of the foreign DNA from the pathogen into the genomic DNA of the host and causing in insertional mutatagenesis. It has been shown that plasmid DNA generated insertional mutations at a far lower rate than what spontaneously occurs within the genome (Ledwith et al, 2000). Another area of safety concern is that injections of DNA will stimulate a systemic autoimmune response. Again, numerous non-primate and human studies did not detect any increase in antinuclear or anti-DNA antibodies (MacGregor et al, 1998; Klinman et al, 2000). To date, there has been no convincing evidence from numerous clinical trials of DNA associated autoimmunity. In additions, there are numerous and very stringent governmental regulations in place for the development of any DNA vaccines development. (Smith & Klinman, 2001). Although DNA vaccines have been proven to be safe and elicited immune responses, they have been rather disappointing in the magnitude of immune response that is generated. Despite promising results in rodent models, DNA vaccinations have proven less effective in primate studies. It has become evident that simply injecting DNA does not sufficiently stimulate the immune system. Clinical trials of DNA vaccines have shown that DNA vaccines need to be made much more potent to be candidates for preventive immunization of humans. Several approaches have been taken to improve the vaccines. One approach being looked at is the incorporation of immunostimulatory sequences into the backbone of the plasmid (Garmory, Brown, & Titball, 2003). Another strategy that is being researched is the addition of adjuvants, mostly through the use of biologically active molecules such as cytokines, chemokines and co-stimulatory molecules (Ivory & Chadee, 2004). Prime boost (Radcliffe et al, 2006) is another technique that is has recently begun being investigated. DNA vaccines are injected to prime the immune system then attenuated pathogens are injected to boost the immune system Volumes of research are currently being conducted on methods to improve the potency of DNA vaccines and the number of clinical trials of DNA vaccines grows yearly as researchers strive to concoct the magic potion that is an effective DNA vaccine (Figure 2). Early reports of the immunogenicity of plasmid DNA vaccines in laboratory animals sparked interest because of the simplicity and their ability to stimulate the immune response. DNA vaccines have proven extremely useful as a laboratory tool for studying immune responses to a wide variety of viruses, bacteria and parasites. However, it has yet to be determined whether researchers will ever be able to overcome technical hurdles and develop a DNA vaccine with clinical applications. DNA vaccines have rapidly advanced to clinical trials with second generation formulations, delivery devices, and mixed modality approaches and hold great promise for new vaccines and immunotherapeutics against a barrage of depilating diseases. There are certainly numerous promising Phase I and II clinical trials (www.clinicaltrials.gov lists 97 currently recruiting and over 300 active trials) underway that will help advance the field of DNA vaccines. Unfortunately, it will more than likely take years before a FDA approved DNA vaccine is marketed for human use in the United States. The concept of DNA vaccines is efficient and elegant. However, the practically application is proving to be a bit of a challenge. Figure 1 Figure 2 Plot showing increasing usage of naked/plasmid DNA in gene therapy trials throughout the world (Journal of Gene Medicine, 2004) Both the number of trials and the percentage of total trials using naked or plasmid DNA has been increasing since 2000. No data were available later than 2003. Barouch, D.H., Santra, S., Tenner-Racz, K., & et al, (2002). Potent CD4+ T Cell Responses Elicited by a Bicistronic HIV-1 DNA Vaccine Expressing gp120 and GM-CSF. The Journal of Immunology, 168, 562-568 Barry, M.A., Lai, W.C., & Johnston, S.A. (2002). Protection against mycoplasma infection using expression-library immunization. Nature. 377, 632 - 635. Bhattacharya , S. (February 2005). DNA vaccine offers hope against tuberculosis. New Scientist, Retrieved March 15, 2007, from http://www.newscientist.com/article.ns?id=dn6966 Brown, K.S. (1996). DNA vaccines: A fluke emerges. The Scientist, 10[7], Retrieved March 12, 2007, from http://www.geocities.com/issues_in_immunization/developments/dna_vaccines_j enner.htm Center for Infectious Disease Research and Policy, (2005, July 21 ). West Nile shot for horses is first licensed DNA Vaccine. Retrieved March 19, 2007, from CIDRAP Web site: http://www.cidrap.umn.edu/cidrap/content/other/wnv/news/july2105wnv.html Donnelly, J.J. (2003). DNA Vaccines. In R. W. Ellis and B. R. Brodeur (Eds.), New Bacterial Vaccines. Austin, TX: Landis Bioscience ISBN 0-306-47832-3 Drape, R.J., Macklin, M.D., Barr, L.J., Jones, S., & Haynes, J.R. (2006). Epidermal DNA vaccine for influenza is immunogenic in humans . Vaccine. 24, 4475-4481. Forde, G.M. (2005). Rapid-response vaccines—does DNA offer a solution?. Nature Biotechnology, 23, Retrieved March 12, 2007, from http://www.nature.com/nbt/journal/v23/n9/full/nbt0905-1059.html Fynan, E.F., Webster, R.G., Fuller, D.H., & et aL, (1993). DNA Vaccines: Protective Immunizations by Parenteral, Mucosal, and Gene-Gun Inoculations. Proceedings of the National Academy of Sciences of the United States of America, 90, No. 20, 11478-11482. Garmory, H.S., Brown, K.A., & Titball, R.W. (2003). DNA vaccines: improving expression of antigens. Genetic Vaccines and Therapy, 1:2, Retrieved March 12, 2007, from http://www.gvt-journal.com/content/1/1/2. Gunderson, D. (2005). Genetic research finds success in Fargo. Retrieved March 12, 2007, from Minnesota Public Radio Web site: http://news.minnesota.publicradio.org/features/2005/12/30_gundersond_aldevron/ Gurunathan, S., Klinman, D.M., & Seder, R.A. (2000). DNA vaccines: immunology, application and optimization. Annual Review of Immunology. 18, 927-974. Haupt, K., Roggendorf, M., & Mann, K. (2002). The Potential of DNA Vaccination against Tumor-Associated Antigens for Antitumor Therapy . Experimental Biology and Medicine. 227, 227-237. Heller, R. (2003).Delivery of plasmid DNA using in vivo electroporation. Preclinica. Vol 1 No. 4, 198-208. Ivory, C., & Chadee, K. (2004). DNA vaccines: designing strategies against parasitic infections. Genetic Vaccines and Therapy. 2:17, http://www.gvtjournal.com/content/2/1/17. Klinman, D.M., Takeshita, F., Kamstrup, S., Takeshita, S., & et al, (2000). DNA vaccines: capacity to induce autoimmunity and tolerance. Developmental Biology. 104, 45-51. Ledwith, B.J., Manam, S., Troilo, P.J., & et al, (2000). Plasmid DNA vaccines: assay for integration into host genomic DNA.. Developments in Biologicals, 104, 33-43. Livingston, J.B., Lu, S., Robinson, H., & Anderson, D.J. (1997). Immunization of the Female Genital Tract with a DNA-Based Vaccine . Infection and Immunity, 66, No.1, 322-329. Lowe, D.B., Shearer, M.H., & Kennedy, R.C. (2006). DNA vaccines: Successes and limitations in cancer and infectious disease. Journal of Cellular Biochemistry. 98, 235-242. MacGregor, R.R., Boyer , J.D., Ugen , K.E., Weiner , D.B., & et al, (1998). First human trial of a DNA-based vaccine for treatment of human immunodeficiency virus type 1 infection: safety and host response.. Journal of Infectious Diseases. 178(1), 92-100. McDonnell, W.M., & Askari, F.K. (1996). DNA Vaccines. New England Journal of Medicine. 334, 42-45. Niethammer, A.G., Primus, F.J., Xiang, R., & et al, (2001). An oral DNA vaccine against human carcinoembryonic antigen (CEA) prevents growth and dissemination of Lewis lung carcinoma in CEA transgenic mice.. Vaccine, Nov 12:20(3-4), 421429. Oh, Y.K., Hwang, T.S., Ko, J.J., & et al, (2001). Nasal absorption and biodistribution of plasmid DNA: an alternative route of DNA vaccine delivery.. Vaccine, Aug 14; 19(31), 4519-4525. Radcliffe, J.N., Roddick , J.S., Friedmann, P.S., Stevenson, F.K., & Thirdborough, S.M. (2006). Prime-boost with alternating DNA vaccines designed to engage different antigen presentation pathways generates high frequencies of peptide-specific CD8+ T cells.. Journal of Immunology. 177(10), 6626-6633. Raz, E., Carson, D.A., Parker, S.E., & et aL, (1994). Intradermal Gene Immunization: The Possible Role of DNA Uptake in the Induction of Cellular Immunity to Viruses. Proceedings of the National Academy of Sciences of the United States of America, 91, No. 20, 9519-9523 Schmaljohn, C. (2006March). DNA Vaccination by gene gun. Retrieved March 26, 2007, from Thomson Pharma Web site: http://www.powdermed.co.uk/pdf/Thomson%20Pharma%20April%202006.pdf Smith, H.A., & Klinman, D.M (2001). The regulation of DNA vaccines . Current Opinion in Biotechnology . 12(3), 299-303. Traxler, G.S., Anderson, E., LaPatra, S.E., Richard, J., & Shewmaker, B. (1999). Naked DNA vaccination of Atlantic salmon Salmo salar against IHNV.. Diseases of Aquatic Organisms. 38(3), 183-190. Ulmer, J.B., Donnelly, J.J., Parker, S.E., Rhodes, G.H., Felgner, P.L., & Dwarki, V.J. (1993). Heterologous protection against influenza by injection of DNA encoding a viral protein. Science 259, 1745 - 1749. Vanderzanden, L., Bray, M., Fuller, D., & et al, (1998). DNA Vaccines Expressing either the GP or NP Genes of Ebola Virus Protect Mice from Lethal Challenge. Virology, 246, 134-144. Wang, R., Doolan, D.L, Le, T.P., et al (1998). Induction of antigen-specific cytotoxic T lymphocytes in humans by a malaria DNA vaccine . Science, 282 Issue 5388, 476-480. Wolff, J.A., Malone, R.W., Williams, P., Chong, W., & Acsadi, G. (1990). Direct gene transfer into mouse muscle in vivo. Science. 247(4949, Pt. 1), 1465-8.