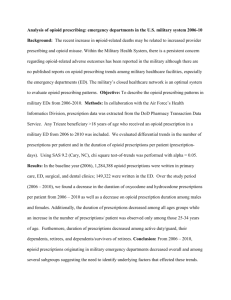
OpiateUseAbuseReport_020312_Draft
advertisement

Opiate Use and Misuse Trends in Texas Abuse of pharmaceuticals is increasing in the United States. According to the National Drug Threat Assessment report, opioid pain relievers are the most widely misused or abused controlled prescription drugs and contribute to most controlled prescription drug-related unintentional poisoning deaths. By 2006, overdoses of opioid analgesics caused more deaths than overdoses of cocaine and heroin combined.1 This report describes the national trends of prescription opiate use and misuse and the corollary trends in Texas. National Problem Scope From 1999 to 2007, the number of U.S. poisoning deaths involving any opioid analgesic (e.g., oxycodone, methadone, or hydrocodone) more than tripled, from 4,041 to 14,459, or 36 percent of the 40,059 total poisoning deaths in 2007 (Figure 1). In 1999, opioid analgesics were involved in 20 percent of the 19,741 poisoning deaths. Figure 1: Number of Poisoning Deaths Involving Opioid Analgesics and Other Drugs or Substances—United States, 1999—20072 In 2009, 1.2 million emergency department (ED) visits involved the nonmedical use of pharmaceuticals or dietary supplements. The most frequently reported drugs in the nonmedical use category of ED visits were opiate/opioid analgesics, present in 50 percent of nonmedical-use ED visits; and psychotherapeutic agents, (commonly used to treat anxiety and sleep disorders), were present in more than one-third of nonmedical ED visits. Among the frequently reported opioids were single-ingredient formulations (e.g., oxycodone) and combination forms (e.g., 1 Harmon, K.; Prescription Drug Deaths Increase Dramatically; Scientific American. Available: http://www.scientificamerican.com/article.cfm?id=prescription-drug-deaths 2 QuickStats: Number of Poisoning Deaths Involving Opioid Analgesics and Other Drugs or Substances --- United States, 1999—2007; Centers for Disease Control; Available: http://www.cdc.gov/mmwr/preview/mmwrhtml/mm5932a6.htm?s_cid=mm5932a6_w DRAFT 1 hydrocodone with acetaminophen). Oxycodone, alone or in combination accounted for 175,949 Emergency Department visits; hydrocodone and methadone accounted for 104, 490 and 70,637 visits respectively.3 From 1991—2009, opioid prescriptions increased four-fold (Figure 2). Figure 2: Total Number of Prescriptions for Hydrocodone and Oxycodone Products Dispensed by U.S. Retail Pharmacies, 1991-20094 Research demonstrates that high opioid prescriptions rates were positively associated with high overdose rates and nonmedical use.5 Nonmedical use of opioid prescriptions costs insurance companies up to $72.5 billion annually in healthcare costs.6 CDC Data The Centers for Disease Control (CDC) Morbidity and Mortality Weekly Report (MMWR) describes the prescription drug overdose problem as an epidemic which has worsened enough that by 2008, drug overdose deaths (36,450) were approaching the number of deaths from motor vehicle crashes (39,973), the leading cause of injury death in the United States. The MMWR describes a four fold increase in opiate pain sales between 2010 and 1999. In 2010, opiate sales were equivalent to 710 mg per person in the United States and enough hydrocodone to medicate every American Adult with 5mg every 4 hours for 1 month. The MMWR also suggests that opiate prescriptions have had a negative impact on mortality based on evidence of increased in opiate prescription sales, opiate abuse treatment, and in admissions to emergency departments.7 3 NIDA InfoFacts: Drug-Related Hospital Emergency Room Visits, National Institute on Drug Abuse, Available: http://www.drugabuse.gov/infofacts/HospitalVisits.html 4 Strategic Plan, National Institute on Drug Abuse, Available: http://www.nida.nih.gov/PDF/StratPlan.pdf 5 Paulozzi, L., Jones, C., Mack, K., Rudd, R.; Vital Signs: Overdoses of Prescription Opioid Pain Relievers—United States, 1999-2008; Centers for Disease Control Morbidity and Mortality Weekly Report; 60(43);1487-1492; Available: http://www.cdc.gov/mmwr/preview/mmwrhtml/mm6043a4.htm 6 Ibid. 7 Ibid. DRAFT 2 In addition to the MMWR, the CDC publishes annual reports on drug poisoning deaths in the United States. These reports track drug poisonings resulting from unintentional or intentional overdoses of a drug, being given the wrong drug, taking the wrong drug in error, or taking a drug inadvertently. Deaths were classified using the International Classification of Diseases (ICD), Tenth Revision (ICD-10). The report classified unintentional poising deaths as accidental overdose of drug, wrong drug given or taken in error, and drug taken inadvertently accidents in the use of drugs using the ICD-10 Causes of Death codes X40-X44.8 The CDC used the following ICD-10 codes to identify drug poisoning as the underlying cause: only nonspecified drug(s) (only T50.9); specified drug(s) other than opioid prescription (codes T36–T50.8); and any opioid prescription (codes T40.2–T40.4); and natural and semi-synthetic opioid prescription (T40.2); methadone (T40.3); synthetic opioid, excluding methadone (T40.4); heroin (T40.1); and cocaine (T40.5). The CDC report also evaluated deaths using an age-adjusted death rate which a death rate that controls for the effects of differences in population age distributions. The CDC report found that the incidence of age-adjusted death rate for drug poising deaths has increased from 6.1 deaths per 100,000 to 11.9 deaths per 100,000 (Table 1). Table 1: Age-Adjusted Drug Poisoning Death Rates, by Demographic Characteristics and Intent: United States, 1999–20089 Year 1999 2000 2001 2002 2003 2004 2005 2006 2007 2008 Total 6.1 6.2 6.8 8.1 8.9 9.3 10.0 11.4 11.8 11.9 Male 8.2 8.3 9.0 10.5 11.4 11.7 12.7 14.6 14.8 14.8 Female 3.9 4.1 4.7 5.8 6.4 6.9 7.3 8.2 8.9 9.0 Hispanic 5.5 4.6 4.4 5.3 5.6 5.2 5.7 6.2 5.9 5.9 Non-Hispanic White 6.1 6.6 7.4 9.2 10.1 10.9 11.7 13.5 14.4 14.7 Non-Hispanic Black 7.5 7.3 7.6 8.2 8.2 8.3 9.4 10.9 9.8 8.5 Non-Hispanic American Indian or Alaska Native 6.0 5.5 6.8 8.4 10.6 12.3 12.9 13.9 13.9 15.6 Non-Hispanic 1.2 1.0 1.2 1.4 1.4 1.5 1.7 1.9 1.9 1.8 Sex Race and Ethnicity 8 X40 Accidental poisoning by and exposure to nonopioid analgesics, antipyretics and antirheumatics; X41 Accidental poisoning by and exposure to antiepileptic, sedative-hypnotic, antiparkinsonism and psychotropic drugs, not elsewhere classified; X42 Accidental poisoning by and exposure to narcotics and psychodysleptics [hallucinogens], not elsewhere classified; X43 Accidental poisoning by and exposure to other drugs acting on the autonomic nervous system; X44 Accidental poisoning by and exposure to other and unspecified drugs, medicaments and biological substances. 9 Warner, M., Chen, L., Makuc, D., et al.; Drug Poisoning Deaths in the United States, 1980–2008; National Center for Health Statistics Data Brief Number 81, December 2011; Available: http://www.cdc.gov/nchs/data/databriefs/db81.htm DRAFT 3 Asian or Pacific Islander Intent Unintentional 4.0 4.2 4.6 5.7 6.3 6.8 7.5 8.8 9.1 9.2 Suicide 1.1 1.2 1.2 1.3 1.3 1.4 1.4 1.5 1.5 1.6 Undetermined 0.9 0.9 1.0 1.1 1.2 1.1 1.0 1.1 1.2 1.1 The CDC data also demonstrates that white and Non-Hispanic American Indian or Alaska Native men are disproportionately affected by drug poising deaths, and most of these deaths are accidental. Men have a 7.7 prescription drug death rate, 5.9 opiate drug death rate, and 4.3 illegal drug death rate. This compares to women who have rates of 5.3, 3.7, and 1.4 respectively.10 For non-Hispanic whites, the rates are 8.4, 6.3, and 2.9. For Blacks, the rates were 3.0, 1.9, and 4.0. 11 Other studies reflect findings similar to those from the CDC. West Virginia A study in West Virginia identified all state residents who died on unintentional drug overdose in the state in 2005. Of unintentional pharmaceutical overdose fatalities, 63 percent of the deaths were from pharmaceuticals obtained without a prescription. The West Virginia Office of the Chief Medical Examiner (OCME) found that 21 percent of deceased individuals had five or more clinicians prescribe controlled substances in the year prior to death (“doctor shopping”). Middleaged white men had the highest risk of overdose from prescription drugs. Women were more likely to have evidence of doctor shopping than men.12 Apparent diversions (persons with no prescribed opioids) were more likely to have a history of substance abuse. Doctor shopping was associated with a history of a previous overdose but a lower risk of prior alcohol use.13 The West Virginia study found that ages 18 through 24 were had the highest prevalence of illegal diversion; while, ages 35 through 44 had the greatest association with doctor shopping.14 Age The CDC data demonstrates that drug poisoning death rates have risen over the past decade and that persons in the prime of their lives, ages 35-54, are disproportionately affected (Figure 3).15 10 Ibid at 5. Ibid at 5. 12 Hall, Aron; Logan, Joseph; et al. Patterns of Abuse Among Unintentional Pharmaceutical Overdose Fatalities. Journal of the American Medical Association; Vol 300 No 22 (2008):2613-2620. 13 Ibid. 14 Ibid. 15 Ibid at 9. 11 DRAFT 4 Figure 3 Drug Poisoning Death Rates by Age: United States, 1999-200816 Veterans Health Administration (VHA) Research from the Veterans Health Administration (VHA) from 2004 through 2008 underscore the conclusion that white men are more likely to have an opioid overdose death. Of a total of 750 opioid overdose decedents, 700 were men, 625 were white, and 610 were between the ages of 40-59. The study examined all opioid overdose deaths matched to a random sample of VHA patients who received opioid therapy for pain. The study found that opioid overdoses were more likely to have chronic or acute pain, substance use disorders, and psychiatric diagnoses; this group was less likely to have cancer. The overdose rate was higher when the maximum dailyprescribed dose was higher. The overdose rate was highest when a patient had concurrent prescriptions (current prescription and a refill) for opioid prescriptions.17 Surveillance Data, Inc. (SDI) Health Investigation of data from Surveillance Data, Inc. (SDI) Health, a data warehouse with access to 50 percent of the national retail prescription data, confirms that most opioid prescriptions (45.7 percent) are for individuals between 40 and 59 years old. Most prescriptions were for hydrocodone and oxycodone (84.9 percent) and issued for 2-3 week courses (65.4 percent). The data demonstrated that most prescribers were primary care physicians who prescribed 28.8 percent of the total prescriptions in 2009. Researchers also demonstrated that 56.4 percent of all prescriptions were dispensed to patients who had already filled at least one opioid prescription within the past month.18 16 Ibid at 9. Bohnert, A., Valenstein, M., Bair, M., et al.; Association Between Opioid Prescribing Patterns and Opioid Overdose-Related Deaths; Journal of the American Medical Association; Vol 305, No. 13 (2011): 1315-1321. 18 Volkow, N., McLellan, T., Cotto, J.; Characteristics of Opioid Prescriptions in 2009; Journal of the American Medical Association; Vol 305, No. 13 (2011): 1299-1301. 17 DRAFT 5 Texas Opiate Data Texas has seen opiate use and misuse trends that mirror those on the national level. A study of the opioid abuse calls to the Texas Poison Center Network (TPCN) confirms Texas has seen increases in opioid abuse similar to national statistics. This system is comprised of the six poison centers that cover the entire state. It is a telephone consultation service that assists in the management of exposures to a variety of substances, including prescription opioids. A single electronic database collects demographic and clinical information on all calls. From 2000-2010 opioid abuse calls increased 160 percent. Hydrocodone, tramadol, morphine, fentanyl, buprenorphine, and hydromorphone calls all increased during that time period; hydrocodone use was associated with almost 60 percent of reported opioid calls to Texas poison centers.19 This section will examine Texas opiate use and misuse trends using data from the Department of State Health Services Center for Vital Statistics, the Texas Poison Center Network, the Drug Enforcement Administration Automation of Reports and Consolidated Orders System, and the Texas Department of Public Safety. Hydrocodone The Drug Enforcement Administration’s Automation of Reports and Consolidated Orders System (ARCOS) data collects data about retail drug distribution. ARCOS data on hydrocodone retail distribution shows that Texas has increased three and a half-fold over the last ten years (Figure 4). Figure 4: Hydrocodone retail distribution per 100,00020 20,000.00 Grams 15,000.00 10,000.00 5,000.00 0.00 1997 1998 1999 2000 2001 2002 2003 2004 2005 2006 Year Texas has always been among the top ten states for hydrocodone distribution. The only states that consistently have similar rates to Texas are West Virginia, Florida, Kentucky, and Tennessee. These states have been increasingly targeted by the DEA as states with diversion problems. California and Pennsylvania, which have similar population to Texas, have significantly lower rates than Texas. 19 20 Forrester, M.; Opioid Analgesic Abuse in Texas; Department of State Health Services. Drug Enforcement Administration Automation of Reports and Consolidated Orders System (ARCOS) data DRAFT 6 As retail distribution of hydrocodone increased, data from the TPCN demonstrates a 67 percent increase in hydrocodone exposure calls from 2000 to 2010 (Figure 5). TPCN data also indicates that 60 percent of all calls to the TPCN are for hydrocodone. Figure 5: Hydrocodone calls received by the Texas Poison Center Network by month 21 2000 Number of calls 1800 1600 1400 1200 1000 800 600 400 Ja n98 Ju l-9 8 Ja n99 Ju l-9 9 Ja n00 Ju l-0 0 Ja n01 Ju l-0 1 Ja n02 Ju l-0 2 Ja n03 Ju l-0 3 Ja n04 Ju l-0 4 Ja n05 Ju l-0 5 Ja n06 Ju l-0 6 Ja n07 Ju l-0 7 Ja n08 Ju l-0 8 200 0 Month Other Opioids, Including Codeine, Morphine, and Oxycodone From 1999 to 2009, the number of other opioid deaths, including codeine, morphine, and oxycodone deaths increased nearly fivefold, while the Texas population increased by only 25 percent. In a 10-year period the other opioid deaths, including codeine, morphine, and oxycodone deaths increased from 122 to 555.22 The 2009 other opioid, death data shows that the population abusing these prescriptions is predominantly white (79.63 percent), male (54.77 percent), and between the ages of 40-55 (41 percent) (Figure 6). 21 Department of State Health Services Texas Poison Center Network data Department of State Health Services, Center Vital Statistics data; ICD-10 code T40.2–other opioids includes poisoning by codeine, morphine, oxycodone, vicodin, etc. opioids other than opium (T40.0), heroin (T40.1) 22 DRAFT 7 Figure 6: Texas Other Opioids, including codeine, morphine, and oxycodone deaths by age23 No. of Deaths 100 80 60 40 20 -8 4 80 -7 9 75 -7 4 70 -6 9 65 -6 4 60 -5 9 55 -5 4 50 -4 9 45 -4 4 40 -3 9 35 -3 4 30 -2 9 25 -2 4 20 4 -1 9 15 --1 10 0- -9 0 Age The data also reveals that the greater Houston metropolitan region24 has a higher number of other opioids, including codeine, morphine, and oxycodone deaths than the similarly sized DallasFt.Worth Metroplex (Figure 7).25 The 12 counties that comprise the Dallas-Ft.Worth Metroplex account for only 88 deaths of the total 555 deaths in 2009; the 10 counties that comprise the greater Houston metropolitan region account for 275 deaths of the 555. 23 Ibid United States Census Bureau greater Houston metropolitan region definitions: Harris, Fort Bend, Montgomery, Brazoria, Galveston, Liberty, Waller, Chambers, Austin, and San Jacinto Counties. 25 United States Census Bureau Dallas Ft. Worth Metroplex definitions: Collin, Dallas, Delta, Denton, Ellis, Hunt, Johnson, Kaufman, Parker, Rockwall, Tarrant, and Wise Counties. 24 DRAFT 8 Figure 7: Other Opioids, Including Codeine, Morphine, and Oxycodone deaths per 100,00026 Over the past 10 years, national Oxycodone retail distribution has increased eight-fold (Figure 8). 26 Ibid. DRAFT 9 Figure 8: Oxycodone retail distribution per 100,00027 5000 Grams 4000 3000 2000 1000 0 1997 1998 1999 2000 2001 2002 2003 2004 2005 2006 Year From 2000 to 2010, the TPCN reported a 165 percent increase in the number of total exposure calls for oxycodone (Figure 9). Figure 9: Oxycodone calls received by the Texas Poison Center Network by month 28 300 Number of calls 250 200 150 100 50 Ja n98 Ju l-9 Ja 8 n99 Ju l-9 Ja 9 n00 Ju l-0 0 Ja n01 Ju l-0 1 Ja n02 Ju l-0 2 Ja n03 Ju l-0 Ja 3 n04 Ju l-0 Ja 4 n05 Ju l-0 5 Ja n06 Ju l-0 6 Ja n07 Ju l-0 7 Ja n08 Ju l-0 8 0 Month While some of the exposure calls, hospital admissions for oxycodone are from illegally obtained prescriptions, legal oxycodone prescribing in Texas increased 6.5 percent from 2007, 442,255 27 28 Drug Enforcement Administration Automation of Reports and Consolidated Orders System (ARCOS) data Department of State Health Services Texas Poison Center Network data DRAFT 10 prescriptions, to 2010 to 471,588 per year.29 Exposure calls increased 32.5 percent during that same time period from 298 calls in 2007 to 395 calls in 2010.30 Methadone Deaths from methadone prescribed for pain have increased 8-fold during 1999-2007 (from 27 in 1999 to 224 in 2007) and then leveled off to just under a 7-fold increase by 2009 (183) (Figure 10).31 Figure 10: Methadone Deaths per Year 250 No. of Deaths 200 150 100 50 0 1999 2000 2001 2002 2003 2004 2005 2006 2007 2008 2009 Year The distribution of the deaths is not as regionally concentrated as the deaths for other opioids (Figure 11). There are a handful of counties with high death rates; however, those counties have relatively small populations. 29 Department of Public Safety Texas Prescription Monitoring Program data. Department of State Health Services Texas Poison Center Network data 31 Department of State Health Services, Center Vital Statistics data; ICD-10 code T40.3 Methadone 30 DRAFT 11 Figure 11: Methadone Death Rate per 100,00032 ARCOS data of methadone by distribution by population in Texas has increased nearly 14 fold (Figure 12). 32 Department of State Health Services, Center Vital Statistics data; ICD-10 code T40.3 Methadone DRAFT 12 Figure 12: Methadone retail distribution per 100,00033 1600 1400 Grams 1200 1000 800 600 400 200 0 1997 1998 1999 2000 2001 2002 2003 2004 2005 2006 Year TPCN data demonstrates a 168 percent increase in Methadone exposure calls between 2000 and 2010 (Figure 13). Figure 13: Methadone calls received by the Texas Poison Center Network by month 34 140 Number of calls 120 100 80 60 40 20 Ja n98 Ju l-9 Ja 8 n99 Ju l-9 Ja 9 n00 Ju l-0 Ja 0 n01 Ju l-0 Ja 1 n02 Ju l-0 Ja 2 n03 Ju l-0 Ja 3 n04 Ju l-0 Ja 4 n05 Ju l-0 5 Ja n06 Ju l-0 Ja 6 n07 Ju l-0 7 Ja n08 Ju l-0 8 0 Month 33 34 Drug Enforcement Administration Automation of Reports and Consolidated Orders System (ARCOS) data Department of State Health Services Texas Poison Center Network data DRAFT 13 Buprenorphine, Fentanyl, Meperidine Deaths of persons using buprenorphine, fentanyl, meperidine more closely tracked than the geographic distribution of the deaths involving other opioids including codeine, morphine, and oxycodone (Figure 14). Buprenorphine is typically used to treat opioid addiction in higher dosages and to control acute pain and moderate chronic pain in lower doses. Fentanyl and Meperidine are used mainly to treat acute and chronic pain. Figure 14: Buprenorphine, Fentanyl, Meperidine Death Rate per 100,000 35 35 Department of State Health Services, Center Vital Statistics data; ICD-10 code T40.4 Buprenorphine, Fentanyl, and Meperidine DRAFT 14 While buprenorphine exposure calls have increased 2900 percent from 2000 to 2010 (from 5 calls in 2000 to 150 in 2010), meperidine exposure calls have decreased by 59 percent during that same time. However, meperidine exposure calls hardly exceeded two or three dozen calls per year. Fentanyl exposure calls increased 181 percent during that time (from 26 calls to 73 calls). While the fentanyl graph appears to show much more variability month to month in the number of calls, the total number of calls is far below those of other prescriptions and the variability is only an artifact of the smaller sample (Figure 15). Figure 15: Fentanyl calls received by the Texas Poison Center Network by month 36 Number of calls 25 20 15 10 5 Ja n98 Ju l-9 8 Ja n99 Ju l-9 9 Ja n00 Ju l-0 0 Ja n01 Ju l-0 1 Ja n02 Ju l-0 2 Ja n03 Ju l-0 3 Ja n04 Ju l-0 4 Ja n05 Ju l-0 5 Ja n06 Ju l-0 6 Ja n07 Ju l-0 7 Ja n08 Ju l-0 8 0 Month Unspecified Deaths In Texas, many overdose deaths will not specify any particular drug. This lack of uniformity in how drug deaths may be coded leads undercounts the number of deaths for any specific drug category. Geographical mapping of unspecified drug deaths demonstrates that the east Texas counties of Montgomery, Orange, Jefferson, and Liberty are disproportionately affected (Figure 16). This distribution mirrors that of the deaths by other opiates. The distribution also reflects DPS and DEA reports of pill mill problems in that region. Unspecified drug deaths have nearly doubled from 1999 to 2009. 36 Department of State Health Services Texas Poison Center Network data DRAFT 15 Figure 16: Unspecified Drug Death Rate per 100,00037 Mechanisms of Diversion Most pharmaceuticals diverted in the U.S. are diverted by doctor shopping, forged prescriptions, theft, and through the internet.38 Doctor shopping is when individuals visit numerous doctors (usually defined as five or more) in an attempt to obtain multiple prescriptions for the drugs, particularly prescription narcotics. Prescription fraud includes a variety mechanisms used to divert 37 Department of State Health Services, Center Vital Statistics data; ICD-10 code T50.9 Unspecified Drug Death Kraman, P.; Trends Alert: Drug Abuse in America –Prescription Drug Diversion; The Council of State Governments (2004); Available: http://www.csg.org/knowledgecenter/docs/TA0404DrugDiversion.pdf 38 DRAFT 16 pharmaceuticals such as forging or altering prescriptions, producing counterfeit prescriptions, and calling in fictitious prescriptions to pharmacies by impersonating a physician.39 Prescription Drug Monitoring As of October 2011, 37 states have PDMPs that have the capacity to receive and distribute controlled substance prescription information to authorized users.40 Eleven states (Alaska, Arkansas, Delaware, Georgia, Maryland, Montana, Nebraska, New Jersey, South Dakota, Washington, and Wisconsin) and one U.S. territory (Guam), have enacted legislation to establish a PDMP, but are not fully operational. In 1982, the Texas Legislature created the Texas Prescription Program to monitor Schedule II controlled substance prescriptions. The program was created to be an efficient, cost effective tool for investigating and preventing drug diversion. In 2008, the Texas Legislature expanded the Program to include the monitoring of Schedule III through Schedule V controlled substance prescriptions. The Texas Department of Public Safety (DPS) operates the Texas Prescription Program. Practitioners and pharmacists can use this program to verify their own records and to inquire about their patients, as well as to generate and disseminate information regarding prescription trends. Access to information is statutorily restricted. It is available to practitioners and pharmacists who are inquiring about their patients and to various regulatory and law enforcement personnel via mail or facsimile request. An electronic request system is expected to be activated in 2012. Other Legislation SB 911 (81R) requires pain management clinics to register and be certified by the Texas Medical Board in order to operate within the state. It also allows the Medical Board to inspect and fine facilities that are in violation of the statute.41 The Texas Medical Board now licenses and regulates pain management clinics that operate in Texas. SB 158 (82R) creates criminal penalties for individuals who “doctor shop” for narcotic medication.42 The rapid increase of deaths and “pill mills” prompted a recent collaborative enforcement effort by the Texas Medical Board (TMB), the Department of Public Safety (DPS), and the Drug Enforcement Administration (DEA) to investigate pill mills, storefronts that often provide powerful narcotics without thorough patient exams often on a cash-only basis. The east Texas area, in particular, has seen a number of investigations of pill mills. In addition, the DEA tracks the prescription medications from the manufacturer to the dispenser. DEA tracks up to the pharmacy. This tracking information can be communicated to DPS. And the DEA may also inform DPS of unusual amounts of prescriptions shipped to a pharmacy. In Texas, DPS tracks prescription medical from the pharmacy to the user. Licensing boards may use the 39 Ibid. Alabama, Arizona, California, Colorado, Connecticut, Florida, Hawaii, Idaho, Illinois, Indiana, Iowa, Kansas, Kentucky, Louisiana, Maine, Massachusetts, Michigan, Minnesota, Mississippi, Nevada, New Mexico, New York, North Carolina, North Dakota, Ohio, Oklahoma, Oregon, Pennsylvania, Rhode Island, South Carolina, Tennessee, Texas, Utah, Vermont, Virginia, West Virginia, and Wyoming; Available: http://www.deadiversion.usdoj.gov/faq/rx_monitor.htm 41 http://www.capitol.state.tx.us/tlodocs/81R/billtext/pdf/SB00911F.pdf#navpanes=0 42 http://www.capitol.state.tx.us/tlodocs/82R/billtext/pdf/SB00158F.pdf#navpanes=0 40 DRAFT 17 prescription information and registrants can use it for themselves or for their patients. DPS also tracks the shipping of prescription medications if the prescription is manufactured in Texas. Best Practices The American Academy of Pain Medicine recently developed best practice guidelines on the initial prescription and subsequent monitoring of opioids. Best practices should include the following: 1. Standardized screening procedures and special provisions for managing pain in those most at risk for abuse; 2. indications for when and for how long to prescribe opioids vs nonopioids; 3. guidelines for when to prescribe short vs long-acting opioids; 4. limits on the number of pills prescribed so that it matches the number of treatment days required; 5. when and how to use urine screening to manage risk of diversion, abuse, and addiction; 6. when an how to use patient contracts to manage risk; 7. proper use of prescription drug monitoring programs to reduce doctor shopping; and 8. criteria for deciding whether and under what circumstances to refill or discontinue opioid prescriptions.43 The Affordable Care Act provides states new authority to monitor diversion in the Medicaid program. It allows states to establish enrollment moratorium periods when providers are suspected as being a risk for diverting drugs. It also requires states to suspend payment and billing when there is a credible allegation of diversion.44 CMS has guidelines about appropriate management of diversion in the Medicaid program. CMS advocates using a Drug Utilization Review (DUR) process that has access to a database of all controlled substance prescriptions filled. It allows regulatory agencies identify outliers in prescriptions and utilization. CMS recommends greater coordination with state and national prescription drug regulatory agencies.45 A GAO report titled Medicare Part D: Instances of Questionable Access to Prescription Drugs identified that there was evidence of doctor shopping in the Medicare Part D program. The report found that 1.8 percent of the beneficiaries acquired frequently abused drugs (including hydrocodone and oxycodone) from five or more medical practitioners during 2008 accounting for $148 million in drug costs. The report indicated that a DUR process in conjunction with a restricted recipient program has been effective in curtailing prescription drug abuse and misuse. A restricted recipient program restricts beneficiaries who have been identified as drug abusers to one prescriber, one pharmacy, or both for receiving prescriptions.46 Experts recommend individuals dispose of their unused prescription medication. Unless the medication indicates that can be flushed away, prescriptions should be disposed of in the manner 43 Volkow, N., McLellan, T.; Curtailing Diversion and Abuse of Opioid Analgesics Without Jeopardizing Pain Treatment; Journal of the American Medical Association; Vol 305, No. 13 (2011): 1346-1347. 44 Centers for Medicare & Medicaid Services; Drug Diversion in the Medicaid Program: State Strategies for Reducing Prescription Drug Diversion in Medicaid; Available: https://www.cms.gov/MedicaidIntegrityProgram/Downloads/drugdiversion.pdf 45 Ibid. 46 United States Government Accountability Office; Medicare Part D: Instances of Questionable Access to Prescription Drugs; Report to Congressional Requesters; (2011): Available: http://www.gao.gov/assets/590/585424.pdf DRAFT 18 indicated on the label. This may mean removing the medication from its container and mixing it with coffee grounds or other undesirable substances to make the medication less appealing to children or people who may intentionally go through trash. Unfortunately, there is no provision in the Controlled Substances Act or Code of Federal Regulations (CFR) for a DEA registrant, pharmacy, physician, to acquire unused dispensed prescriptions from an individual patient. DEA registrants can return the controlled substance to the pharmaceutical manufacturer who, as a service to its customers, accepts returns of outdated/damaged controlled substances. Under 21 CFR 1307.21, a registrant may request permission to dispose of controlled substances without the benefit of a DEA or State witness. In some cases, the DEA may issue ongoing permission for disposal of controlled substances. The DEA must authorize the disposal in writing and may require a set schedule. Other registrants are granted disposal authority on a case-by-case basis. DEA normally requires that the registrant provide two designated responsible individuals to accompany the drugs to the disposal site and witness the destruction. The DEA also allows a distributor, dispenser, or manufacturer to distribute controlled substances to a reverse distributor to take control of the controlled substances for the purpose of returning them to the manufacturer or, if necessary, disposing of them.47 There are two DEA registered reverse distributors in Texas: one in Fort Wroth and another northeast of the Dallas–Fort Worth Metroplex. A Controlled Substances Act exemption allows law enforcement to collect previously dispensed prescription drugs.48 Individuals can dispose of medications themselves or they can participate in some of the National Drug Take Back activities.49 The Texas Tech School of Pharmacy also operates a medication disposal service with assistance from law enforcement.50 Next Steps 1) Create a workgroup of law enforcement, regulatory entities, public benefits programs, and providers to create solutions for increase collaboration and eliminating service and information gaps. 2) Conduct quality of care studies by providers in Texas. 3) Increase the speed of data from the Texas Prescription Program. 4) Increase educational programs for providers/prescribers and the public. 5) Partner with insurers (public and private) and prescription drug monitoring plans to evaluate use in different populations. 6) Consider setting guidelines for providers about requirements for maximum prescribed dosages, specialist consultation, pain management agreements, and required follow-up for pain medication prescriptions. Look to best practice models in other states or entities such as Washington State. 7) Implement best practices programs around the state. 47 http://www.deadiversion.usdoj.gov/fed_regs/rules/2005/fr0502.htm http://www.deadiversion.usdoj.gov/fed_regs/rules/2009/fr0121.htm http://www.deadiversion.usdoj.gov/drug_disposal/takeback/takeback_102911.html 50 http://medicationcleanout.com/default.aspx 48 49 DRAFT 19 Conclusion Achieving the appropriate balance between therapeutic mitigation of pain and unintended abuse and misuse of opiates will require coordination between law enforcement, professional trade groups, community health providers, Texas Medicaid, and many other groups and entities. Their collaboration will allow Texas to monitor prescription drug diversion, emphasize appropriate treatment guidelines, target opiate abuse treatment, and assist in responsible disposal of prescriptions. DRAFT 20