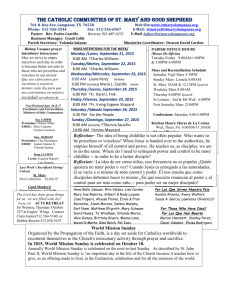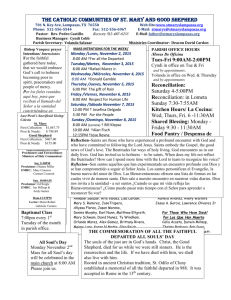
This Week's News
23 January 2009
Weekly news clippings service featuring articles on the Global Health Workforce Alliance and
selection of articles from around the world on the issue of the health workforce crisis
The Global Health Workforce Alliance ¦ Africa & Middle East ¦
Asia & Pacific ¦ North America ¦ Europe ¦ Latin America & Caribbean ¦
News from WHO and partners
This compilation is for your information only and should not be redistributed
News related to Global Health Workforce Alliance
Date
Headline
Publication
24.01.09
2009: a crucial year for progress on the health workforce crisis
The Lancet, UK
Africa & Middle East
Date
Headline
Publication
19.01.09
Stop paying health workers from monthly grants- Dr. Miti
Lusaka Times
17.01.09
WD sponsors TV programme on maternal health
19.01.09
Alas, no frorex for Zimbabwe's health care personnel
17.01.09
Health education, not doctors to keep the poor healthy
Daily News,
Tanzania
Harare Tribune,
Zimbabwe
Swazi Observer
19.01.09
Imperative of primary health care
Nigerian Tribune
20.01.09
2009 health prediction was off the mark
20.01.09
YEMEN: What is blocking progress on MMR?
New Vision,
Uganda
UN IRIN
Asia & Pacific
Date
Headline
Publication
20.01.09
Nurses dead on their feet from too much overtime
The Australian
North America
Date
Headline
Publication
21.01.09
Nurse shortage in Indiana
Carroll County
Comet, IN
20.01.09
Nurses broaden health care vision
S. Antonio
Express, TX
1
01.09
Tackling Human Resources in Africa
The Scientist
18.01.09
Coahoma CC receives $1.99 million federal grant
15.01.09
Are would-be health care workers
17.01.09
UN says Gaza hospitals in crisis
Fort Mill Times,
SC
Michigan
Business Review
Associated Press
16.01.09
Lawsuits Filed Over Rule That Lets Health Workers Deny Care
Washington Post
20.01.09
Study: Clinic staffing at critical low
RecordNet, CA
18.01.09
As Canada greys, health jobs soar
19.01.09
Engager plus d'infirmières ne réglera pas la pénurie
The Vancouver
Province,
Canada
La Presse de
Montréal
Europe
Date
Headline
Publication
13.01.09
Working on the Congolese front line
BMJ
17.01.09
UN provides $5 mln for Zimbabwe health workers
Reuters, UK
17.01.09
Gaza: Need for Protection of Medical Facilities and Personnel in Gaza:
UN
Muslim News, UK
19.01.09
WHO chief says Gaza vulnerable to disease outbreak
Reuters, UK
15.01.09
Poor nations’ health systems must be boosted to improve maternal
and newborn health, Unicef says
BMJ, UK
16.01.09
Lettre ouverte à M. le Président de la République
14.01.09
Milburn is to head initiative to widen entry to medical training
Coordination
Nationale
Infirmière, France
BMJ, UK
13.01.09
Health crisis in Zimbabwe is "man-made" and needs intervention
from all UN states, report says
BMJ, UK
15.01.09
Health is a human right
BMJ, UK
21.01.09
Health workers vote to strike if HSE forces changes
Irish Times
Latin America & Caribbean
Date
Headline
Publication
23.01.09
SALUD-PARAGUAY: Hola Roma, adiós dengue
IPS-Latin America
16.01.09
Dilos instruye a la Alcaldía contratar a personal para hospitales
El Deber, Bolivia
16.01.09
Denuncian falta de personal que pueda brindar primeros auxilios
16.01.09
55% de los recursos de salud se concentran en Asunción
20.01.09
Quedaron sin contrato más de 25 enfermeras
ABC Digital,
Paraguay
Última Hora,
Paraguay
Entorno
Intelligente,
Venezuela
News from WHO and partners
Date
Headline
Publication
20.01.09
Restoring Reproductive Health Services and Addressing PostTraumatic Stress in Gaza
UNFPA
2
07.01.09
International Council of Nurses Announces New Nursing Education
Network
ICN
20.01.09
International Council of Nurses Gaza statement
ICN
13.01.09
Doctors Call Zimbabwe’s Ruined Health System a “Man-Made
Disaster”
PHR
21.01.09
*Measuring inequalities in the distribution of health workers: the
case of Tanzania
HRH Journal
* All links to HRH Journal will be to an external web page - copy is not reproduced in this document.
News related to Global Health Workforce Alliance
2009: a crucial year for progress on the health workforce crisis
The Lancet, UK
24/01/2009
Volume 373, Issue 9660, Page 300
Sigrun Møgedal a, Mubashar Sheikh
2008 was an exceptional year for the response to the global health workforce crisis. The endorsement of the
Kampala Declaration and Agenda for Global Action1 in March, 2008, signalled a milestone. Adopted at the first
ever Global Forum on Human Resources for Health convened by the Global Health Workforce Alliance (GHWA)
in Kampala, Uganda, these agreements provide strategies to help close the health-worker gap over the next
decade.
In its 2008 Declaration,2 the G8 recognised the importance of the Kampala documents in driving forward the
response, and pledged to work towards increasing the health workforce by supporting efforts, such as those of
GHWA, in developing robust health workforce plans, policies, and country-led milestones.2
Specific donor commitments from the UK, the USA, and Japan to train new health workers have boosted this
response. At the UN high-level meeting on the Millennium Development Goals in September, 2008, resolving
the health workforce crisis was underlined as central to the achievement of the health-related targets. A new
taskforce on Innovative Financing for Health was launched, the mandate of which includes finding solutions for
funding more than 1 million additional health workers by 2015.
All of this is very promising, but now the challenge is to transform pledges into action in the context of an
unprecedented global financial crisis. Collective responsibility is needed. Donor countries must live up to,
increase, and sustain their commitment of resources, and low-income countries must find ways to increase
resources while using available resources more effectively and efficiently. Ambitious health and development
plans should not be postponed. GHWA has developed a 3-year framework of strategies and priorities to face
this time of challenging opportunity, based on building synergy between Alliance partners, increasing advocacy,
brokering knowledge, and monitoring progress.
2009 is crucial in many key areas. Country plans with on human resources for health are being developed, but
must be needs-based and fully funded if we are to move beyond rhetoric. Global health initiatives such as the
International Health Partnership and the Global Fund must take steps to ensure that adequate funding is
allocated for health workforce strengthening within their programmes. GHWA will be monitoring progress and
reporting back at its next Forum.
Governments, development partners, international organisations, civil society, the private sector, academia,
and others must maintain momentum and work together. The world will be looking towards the next G8
summit for sustained leadership and improved resource allocation to ensure that the exceptional work of 2008
moves from words to deeds, resulting in concrete progress on the ground in 2009.
We declare that we have no conflict of interest.
References
1 Global Health Workforce Alliance / WHO. The Kampala Declaration and Agenda for Global Action. Geneva:
Global Health Workforce Alliance / World Health Organization, 2008.
2 G8 Hokkaido Toyako Summit Leaders Declaration.
http://www.mofa.go.jp/policy/economy/summit/2008/doc/doc080714__en.html. (accessed Dec 9, 2008).
a Global Health Workforce Alliance, World Health Organization, 20 Avenue Appia, 1211 Geneva 27, Switzerland
Back to top
3
Africa & Middle East
2
Stop paying health workers from monthly grants- Dr. Miti
Lusaka Times
19/01/2009
The Ministry of health has directed District Directors of Health and Executive Directors to stop employing and
paying health workers using monthly grants because the practice is illegal.
Permanent Secretary, Simon Miti sounded the warning in a circular dated 24 November,2008 and made
available to ZANIS in Mazabuka yesterday.
Dr Miti said the continued employing of health workers and paying them using grants is an illegal practice
because the ministry of health is not the employer.
He explained that employment of health workers is the prerogative of the Public Service Commission through
the Public Service Management Division (PSMD).
Dr Miti further reminded the Directors that under the public finance Act 15 of 2004, part XVI clause 191 paying
salaries from the operational grants constitutes misapplication of funds and attracts appropriate sanctions to
the institution.
He said employment application forms should now be channeled through the office of the Permanent Secretary
in the Ministry of health.
Meanwhile, several classified daily employees at Mazabuka District Hospital have lost their jobs following the
directive by Dr. Miti.
The affected workers have however threatened to take legal action against the Ministry of health for breach of
contract.
Mazabuka district hospital administrator, Esau Mujansi refused to comment and referred all queries to district
director of health, Dr Namasiku Siyumbwa who could not be reached by press time.
3
WD sponsors TV programme on maternal health
Daily News, Tanzania
17/01/2009
Women's Dignity (WD) has sponsored a unique TV programme for broadcasting research findings on maternal
health issues in Rukwa region, it has been learnt. A statement issued by WD’s Executive Director, Ms Christine
Matovu in Dar es Salaam yesterday said that the programme would be highlighting major maternal health
problems affecting rural communities in the country.
The statement said the TV programme contracted to Sahara Communications and Publishing Limited and
Tanzania Broadcasting Corporation (TBC) would be aired by Star TV and TBC1 beginning next Saturday. The
seven identified maternal health problems to be aired, according to the statement, include the negative impact
of long distance and transport bottlenecks on pregnant mothers and lack of skilled health workers.
Other maternal tribulations include lack of good working conditions among health workers in the rural
environment, mistreatment of hospitalized expentant mothers and lack of skilled health workers. “The thirty
minutes documentary is exciting as poor people in the remote rural areas of Sumbawanga District express their
own assessment with regard to the provision of maternal health services,” read the statement in part.
It says that the documentary also shows some people acknowledging and commending the government health
workers for saving the lives of ailing pregnant mothers. The statement said that the programme would also
incorporate the views of ordinary citizens, policy makers and government officers working in the health sector.
“WD commends the government’s efforts in implementing the National Strategy for Growth and Poverty
Reduction (MKUKUTA) 2005-2010 which aims at reducing maternal mortality to 263/100,000 live births,” the
statement said.
The statement noted that the major objective of the programme is to raise public awareness and generate
public debate on the problems and seek possible solutions for the continuing high level of maternal deaths.
According to the report of the 2004 Tanzania Health Demographic Survey (THDS) maternal mortality ratio in
the country is still high reaching 578 deaths for every 100,000 live births, while the neonatal mortality rate is
32/1,000 live births.
4
Alas, no frorex for Zimbabwe's health care personnel
Harare Tribune, Zimbabwe
19/01/2009
IVENE CHEUNGA JAMS
4
The government of Zimbabwe has no foreign currency to pay health workers amid information leaks that abuse
of equipment at most referral hospitals is now rife as the suffering workers try to eke out a living.
News that their wages were to be paid in forex had been welcomed by most health care personnel across
Zimbabwe. The workers were demanding salaries averaging US$1 000, but the ministry of health is reportedly
dragging its feet in a bid to buy time.
The ministry, although the UN has offered to pay the salaries of the heath care personnel, says it has no forex
to pay its workers.
The poor salaries the ministry is paying the health care professionals has led to rampant corruption in most
government controlled hospitals and clinics.
“As a result of the delay, nurses and doctors are now conniving and are using theatres and other aligned
equipment to help clients with treatment as they are now required to pay for the services in foreign currency,”
said a source at Parirenyatwa.
He said that instead of paying the required US$300 for a surgical operation and bookings of the theatre room,
they have since slashed their illicit charges that are not known by the superiors by half and most customers are
taking that route.
Patients are now being asked to fork out US$80 as consultation fees. They are further being asked to pay
US$100 admission fees per day at most hospitals the development that has driven most poor people to an
early grave.
It has also emerged that the earlier published reports by the official press that health workers were asked to
open Foreign Currency Accounts (FCAs) were hoax as such a development is still a far cry from reality.
The “minister” of health and child welfare Dr David Parirenyatwa was not reachable for comment at the time of
going to press.
In a related development, Raymond Majongwe the President of the Progressive Teachers of Zimbabwe has also
said that teachers have vowed not to go to work unless they are paid US$2000 salaries per month in line with
the dollarisation of the economy.
The war veterans of Zimbabwe have since dismissed the demand with their leader Joseph Chinotimba saying
using the US dollar as our formal currency amounts to re-colonisation.
Meanwhile the marking of grade seven, Ordinary Level and Advanced Level examinations has been stalled by
shortage of foreign currency as the government has said that it does not have enough resources to meet the
demands of the markers. The markers are demanding US$20 per script while the government is offering US$6
5
Health education, not doctors to keep the poor healthy
Swazi Observer
17/01/2009
By Fanyana Mabuza
The World Health Organisation (WHO) estimates that giving the world’s poor equal access to basic health care
would take an additional 4.3 million doctors, nurses, and other health work staff.
But merely educating more doctors is not the answer, claim physicians in the growing field of global health,
who are championing health care as a human right and essential to economic development.
They see success in public health systems anchored by programmes like the Rural Health Motivators and
investing in their training to be the front line in preventing care and treating diseases, especially among the
rural poor.
Make Lombango Tsabedze of Emkhulamini, in the Manzini region can be said to be among such physicians,
despite her acute lack of training and qualification.
She has been providing health care to the disadvantaged in her community such that residents know where to
knock when they are in health dire straits, even during the middle of the night.
Mkhulamini is a semi-urban village on the outskirts of this central Swaziland city. Despite its close vicinity to
the hub of Swaziland, life is not easy here. Simple travel becomes a nightmare when the downpours come
crashing down and lick the parched earth road that leads from the city.
During the dry spell, when one vehicle passes, thick clouds of dust bellow into the air and eventually nestle on
the window sills of the homesteads nearest to the road.
Although it cannot be said that poverty is rife here, but general desolation is evident all round, hence Make
Tsabedze’s role cannot be underscored. Many homesteads here are still made of timber logs, spot thatched
roofs and dung floors.
There is a growing middle class though, comprising professionals born and bred here. Though residing in the
cities, they were wise enough to remember to build modern houses, which they use when they come for the
Christmas break or when a wedding or funeral calls.
5
“Doctors may promote medical care because that is where the money is, but we promote health, however
meagre it could be. Just because it is done with a willing heart, we, in most cases, succeed in saving lives, or
at least facilitating a quick transfer to the nearest hospital, in our case the Raleigh Fitkin Memorial Hospital
about 15 kilometres away,” she disclosed. This mother of seven, who cannot recall her exact age as a result of
illiteracy, mentioned that with the little training she has received in rural health motivation workshops, she now
knows when to administer oral rehydration salts (ORS) or assist in childbirth.
“We work without a budget, limited working tools and in most cases we are forced to dig deep into our own
pockets to assist. In some cases, we run short of even the gloves that are provided by the Ministry of Health
and we have to improvise, since it is always stressed to us that we should never touch a patient with our bare
hands. But sometimes the human being in you forces you to improvise as you cannot fold your hands and
watch a soul suffering.” Another of her colleagues, Fikelephi Kunene from Malindza mentioned that even
though she did not have concrete proof, some of her peers have even ended up catching the dreaded virus
after rushing in to assist an HIV positive person when her supplies of gloves had run dry.
“You realise later that you assisted an HIV positive person without any protection as a result of the will to
serve. We do not look at people as negative or positive but just as human beings, which can be so dangerous.
But with the Lord willing we will persevere against all such odds,” she said.
She closed by stating that they had eventually learnt that in many instances, the people did not really need a
doctor, but basic things like clean and safe drinking water, health education, balanced meals and poverty
alleviation. “These things do more to promote health than diagnostic tests and drugs,” she said.
6
Imperative of primary health care
Nigerian Tribune
19/01/2009
By Emmanuel Monjok
Nigerians need to be educated on what is General Practice (GP) and who is a general practitioner or family
practitioner (USA/Canada). Many people in Nigeria, unfortunately including many doctors, still think general
practitioners(GPs) are “second rate” doctors and general practice speciality is reserved for the “never do well”.
This misconception was the reason why doctors who were unable to pass their postgraduate medical
examinations in surgery and obstetrics and gynaecology at the University of Calabar Teaching Hospital (UCTH)
were transferred to general practice some years back, by the hospital management.
Significant progress has been made, since 1999, in the tertiary and specialist hospitals and the Federal
Government, responsible for this level of health care, should be acknowledged for this. But, it is the primary
and secondary healthcare services that are in total collapse. What represent this level of healthcare are the
general hospitals (secondary level facility) and the Primary Health Care (PHC) systems that is, comprehensive
health centres and the primary health centres . These two levels of healthcare are the preserve of the State
Government (general hospitals) and the Local Government (PHC). For the PHC and secondary health care
system to function adequately , the categories of health personnel at these levels need development, attractive
career service and most importantly efficient management.
A general practitioner/family practitioner is a doctor that has undergone postgraduate specialist training (after
the primary medical degree) in General Practice (UK) or Family Medicine (USA/Canada). His specialization is in
the common diseases and procedures in the community which also includes disease prevention. The training
period is four years in Nigeria, three years (USA /Canada), and recently between three and five yearrs in the
UK. What constitute the training programme in general practice varies from country to country.. Nigeria was
fortunate to have had late Dr Charles Pearson (a British), who started the postgraduate training programme in
GP in 1980, which was a unique model similar to the rural model in USA, Canada and Australia. The late Dr
Pearson advocated the rural model because more than 65% of Nigerians reside in rural areas, with many
remote and hard to reach communities. This gave birth to the Nigerian model of GP training which was unique
because it was intended to close the gaps between primary and secondary healthcare, since both were
rudimentary. The training was also intended to form the base for the development of super-specialities at the
teaching and specialist hospitals. Also, one of the intentions was for general practitioner in Nigeria to have a
well defined career pathway (like in UK or USA) which will be attractive with significant government inputs,
with the aim of a long term medical care programme for the vast population in our country. This unfortunately
has not happened almost 28years since the introduction of the speciality in Nigeria. But, this is what had
occurred in other developed countries, like UK, USA, Canada and developing countries like Cuba, Brazil, India,
China and Oman. In these countries , General Practitioners/Family Practitioners are respected because of the
defined career path laid out by governments, medical councils and politicians.
In Nigeria, GP as a speciality is still looked upon by the populace, not as a speciality but as a transition to other
specialization. This misconception as well as the lack of a defined career pathway explains why many young
doctors are not interested in taking up positions in the PHC system and secondary healthcare systems. In
Cross River State for example, there are very few doctors working in the 18 general hospitals covering the 18
local governments areas of the state ,rather almost 90% of all the doctors in the state are working in
Calabar(state capital), the majority as resident doctors(Postgraduate doctors) at UCTH. There are virtually no
doctors employed in the local government health service since the Local Governments do not employ their own
doctors; they rely on the state Ministry of Health . Also, the postgraduate training in GP in Nigeria, though
officially four years, is most often times completed within an average of six- eight years, which is too long for
any organisation to embark on manpower development. The few doctors sent by the Cross River State Ministry
of Health for postgraduate training at the UCTH never returned to serve the Ministry of Health hospitals
6
because, after spending an average of seven years at the teaching hospital for training, they see themselves as
super-specialists, and so take up jobs at the university or specialist hospitals.
There are so many communities in this country without adequate health care services . Most of the 774 local
governments areas and the various communities are with a collapsed healthcare system.. Therefore, the
development of PHC and secondary health facilities is what this country should be investing financial resources
in, alongside the development of tertiary level facilities. Nigeria has enough financial and human resources to
strengthen these two sectors of healthcare and also change the concept of general practice, community
medicine and public health. All that is required is the political will.
Nigeria is a vast nation, like USA, Canada and Australia. These advanced nations with super –specialization and
high technology medicine with 20% of their population living in remote areas, are still showing more political
will and commitment to General Practice/Family Medicine than Nigeria with more than 65% of the people living
in remote villages with poor network of roads, and poor health services. If Nigeria invests more in primary and
secondary healthcare services, there is no reason why a Nigerian woman should die during pregnancy or child
birth from preventable causes. Nigeria has one of the highest maternal mortality rate in the world (greater
than 1000 deaths per 100,000 live births), in the same category with Sierra Leone, Niger, Chad, Somalia,
Angola, and the Democratic Republic of Congo. These African countries are ravaged by war and conflict, but
Nigeria is not. It is really shocking, especially when you consider the wealth and resources of this country.
According to Late Professor Ransome Kuti, former Health Minister and champion of PHC in Nigeria, “Nigeria is
trying to run before she learns how to sit properly”. The current Minister of Health, the state commissioners for
health, and the 774 Local Government Chairmen as well as the National Postgraduate Medical College of
Nigeria, should please consider the development of PHC, secondary health facilities and short postgraduate
training programmes in GP, as an emergency. It is not too late to start!
Dr Monjok is of the University of Houston, Institute of Community Health, Texas Medical Centre, USA.
© 2004 - 2009 African Newspapers of Nigeria Plc.
7
2009 health prediction was off the mark
New Vision, Uganda
20/01/2009
By Nicholas Kamara
Dr James Tibenderana gave a fair analysis about the state of health in 2009 in your booklet ‘Uganda in 2009’
but failed to capture some aspects. I do not know where Dr Tibenderana works but I guess he is one of the
technocrats at the Ministry of Health who sometimes can be out of touch with the reality on the ground.
Perhaps, he was looking at the situation from a perspective of an epidemiologist, which is different from mine,
a practicing clinician.
I have had a chance to work in a Health Centre IV, a mission hospital and I now work in a regional referral
hospital, in my last eight years of service. Most health workers will agree that there was a time around 20002003 when the Ministry of Health seemed to be getting things right, but it is laughable to say that health will
improve in 2009.
The health situation in the country has never been as bad, in recent years as it was in 2008.
Hospitals experienced the worst shortage of drugs in many years, the Government ensured that fresh
graduates at URA got more salary than senior doctors and the indifference of health workers who were either
demoralised or bored, increased.
Throughout the year, there were several reports of ancient diseases like plague, onchocerchiasis (river
blindness), filariasis and hepatitis ravaging villages and killing the common man. The health workers became
less involved as they saw things fall apart.
For all the failures of government, Dr. Steven Mallinga, the health minister was a rational politician, always
crying about the poor conditions of health workers.
This is what I think about 2009. The AIDS, malaria indicator surveys are unlikely to be accurate in 2009, since
the officials will sit in towns, forge results like the Karamoja census and give us wrong results.
I agree with Dr Tibenderana, though, that donor funding will reduce, making many HIV patients on antiretroviral drugs to stop and make many others die without ever having a chance to access these drugs.
The working conditions of health workers will not improve and the Mbarara Hospital building will not start until
2011 when it will act as a political gimmick to amass votes. Granted, the health budget may increase, but with
creation of new districts in the year 2009, health units will also increase. Must I also mention that Ugandans
are becoming more corrupt?
The officials at the Ministry of Health will prefer to hold seminars in large hotels for capacity building and
consultations.
7
They will have a large budget to fund their avalanche of vehicles. They will make false reports whose results
will never be implemented. All this will be at the expense of the basic services meant for the common man.
They will wait for the end of the year to make new budgets and the situation will continue ad infinitum.
However, one thing will be consistent; our small salaries will come on time and to cover for their inadequacy,
the politicians will continue bashing health workers for stealing drugs and the public will believe them. One or
two big private hospitals in Kampala will close because of increasing running costs.
The doctors will leave the Government hospitals and health units more than ever before and either work in
NGOs, open up private units or go out of the country where their services are appreciated.
In short, 2009 will be a nasty year for health and in my view, this will continue for many, many years.
The writer is a Physician at Mbarara Hospital
9
YEMEN: What is blocking progress on MMR?
UN IRIN
20/01/2009
SANAA, 20 January 2009 (IRIN) - The maternal mortality rate (MMR) remains high as a result of poor health
care and harmful social practices, including child marriage and female genital mutilation, a UN Children’s Fund
(UNICEF) official in Yemen has said.
"Maternal mortality is very high in Yemen. Some 360 women die per 100,000 live births and that figure could
be higher," said Naseem Ur-Rehman, UNICEF’s chief information officer in Yemen, at a press briefing on 18
January to launch the State of the World's Children 2009 report.
Eight women or girls die from pregnancy or childbirth complications every day in Yemen, he said; globally the
figure is 1,500.
According to the UNICEF report, the lifetime risk of maternal death in Yemen is 1:39, making it the highest in
the Middle East.
At the same time Yemen has the lowest percentage of births in the Middle East at which a skilled attendant is
present: Delivery care coverage is 36 percent, and 24 percent of births take place in hospitals.
The report said a study by the World Health Organization (WHO) found that female genital mutilation/cutting,
which is widespread in rural areas, affected the reproductive health of women: It caused severe pain,
prolonged bleeding, infection, infertility and even death.
The report defines maternal mortality as “the death of a woman while pregnant or within 42 days of the
pregnancy’s termination, regardless of the site or duration of the pregnancy, from any cause related to, or
aggravated by, the pregnancy or its management”.
Shortage of health workers
UNICEF's Ur-Rehman said the lack of health workers was one of the reasons for the high MMR and neonatal
mortality rates, adding that Yemen was among 57 countries where “the shortage of health workers is acute”.
“Worldwide, there is a shortage of 4.3 million health workers who provide care at the time of pregnancy and
delivery,” he said, adding that there should be a minimum of 2.28 health workers per 1,000 people.
Yemeni health officials estimate there is one doctor per 10,000 people and that health services reach only 60
percent of the country's 21 million people.
Child marriages
Ur-Rehman said child marriage, which aggravates high fertility rates by giving girls a longer period in which to
have children, added to the risks.
"Yemen faces this problem of child marriages. There are a large number of child marriages and they ultimately
contribute to the deaths of children," he said.
Nabil Mohammed al-Ammari, executive director of the Yemeni Family Care Association, said lack of awareness
about family planning and reproductive health care services also translated into a higher MMR.
He said his association carried out a survey in 2007 in 15 of the 21 governorates on the use of family planning
methods and found that people preferred not to use them for fear of possible side effects.
Al-Ammari said social attitudes also had an impact on MMR. "A father of four or five daughters would love to
have a boy even at the cost of having many children," he said.
According to UNICEF’s Ur-Rehman, three things can reduce the high MMR: better community and family
support for pregnant women; comprehensive health insurance to cover the costs associated with pregnancy,
child birth and post-natal care; and the setting up of establishments where pregnant women from remote
areas can go for advice and help prior to their due date.
8
"Many of these women who are dying are too poor to get to health facilities. Some families take the mother to
hospital, but she turns out to be dead on arrival,” he said.
Back to top
Asia & Pacific
8
Nurses dead on their feet from too much overtime
The Australian
20/01/2009
Lex Hall
NURSE O'Bray Smith knows what it's like to work overtime.
The 28-year-old from Sydney has worked her fair share of consecutive shifts to meet the increasing demands
placed on the labour ward where she has worked for the past five years.
Ms Smith said a lack of skilled workers put extreme pressure on nursing staff, with some nurses working long
hours to ensure wards were kept open and safe.
"It should be a 40-hour week but it's often stretched out to 50," she said. "Otherwise the wards are short of
workers and it's not safe."
Ms Smith said the Government had to urgently address the shortage of skilled workers because of the ageing
nursing population.
"I think it should be the priority and that it should be improved," she said.
"The nursing population is an ageing one -- we need fresh blood and enthusiasm."
Like every health worker, Ms Smith has experienced the strain of staff shortages first hand.
"One day I started work at 1.30pm, finished my shift at 7.30 the next morning, started back at work at 4 that
afternoon, finished that shift at 10 at night.
"Then I went back to work at 7.30am that morning and finished at 10pm. That's two double shifts in three
days. I was knackered.
"Sometimes I think that we are pushed to the capacity and that must have an influence on my care."
Ms Smith said a skilled worker shortage was leading to a breakdown in hospital efficiency and compromising
patient care.
"If you don't have the staff, then you can't open a bed, so patients sit in emergency," she said. "It becomes a
backlog.
"People think there aren't enough beds, but in fact there aren't enough staff to open thebeds."
Do patients notice that health workers are being pushed to such limits? "I hope not," she said.
The upside -- if there is one -- is that such pressure brings workers together. "It makes us closer and stronger
as a team," she said. "But I can't imagine that happens in every ward. It would probably put a lot of pressure
on staff relations."
Ms Smith said that in a field such as nursing, training was a continuing commitment.
In June, she will travel to Melbourne for a two-day workshop in advanced obstetrics -- a course she has
financed herself.
"This one will cost me $1100, and that's not including the accommodation and airfares."
Back to top
North America
1
Nurse shortage in Indiana
Carroll County Comet, IN
21/01/2009
Comet staff report
9
American Health Care Association (AHCA) recently released a report that indicated Indiana's vacancy rate
among staff registered nurses (RNs) in skilled nursing facilities is 26 percent and 13.7 percent in certified
nurses aides.
In response to the report about the nursing shortage, Indiana Health Care Association (IHCA) will press
congress and the new administration to develop healthcare reform plans.
"Indiana's long-term care workforce is facing a shortage crisis which must be remedied to ensure that our
community is able to provide high quality care to the millions of frail, elderly and disabled Americans we care
for," IHCA President Stephen Smith said.
A study released by AHCA in 2007 found nearly 110,000 full-time equivalent health care personnel were
needed to fill vacant nursing positions nationwide. The shortage has been exacerbated by the challenge of
finding enough nurse educators to train a skilled workforce.
"Funding and expanding training programs to ensure a large, well trained labor pool is essential to growing our
workforce." Smith said.
"Congress and the administration must induce reforms allowing states to hire, train and retain direct care
workers in order to close the gap between current supply and future demand," AHAC President and CEO Bruce
Yarwood said.
2
Nurses broaden health care vision
San Antonio Express, TX
20/01/2009
By Justin A. Woodhouse - Special to the Express-News
The boards of directors of hospitals and health care organizations face unprecedented challenges, including
new requirements to track and improve patient safety and quality of care, calls to improve patient satisfaction
and an aging population, coupled with increased staffing shortages.
Responding effectively to these demands requires the strongest possible leadership team, which might include
lawyers, doctors, finance experts, physicians and community leaders. And who better to provide an
understanding and intimate perspective of patient safety, quality care and the inner workings of a hospital on a
board of directors than a nurse?
In my current post at Fort Sam Houston and throughout my 22 years as a practicing registered nurse (RN), I
have witnessed firsthand how the Army Nurse Corp is impacted by the same nursing shortage that plagues
many of our private health care systems. Our recruitment challenge may even be greater, as the Army Nurse
Corp's active duty nurses all must have a bachelors of science degree in nursing, or BSN. Despite these
challenges, the Army Nurse Corp is very active at the executive levels of the Army in developing and
implementing strategies to better recruit and retain nurses.
Yet in a city known for its medical center, can we say that private sector health care systems and employers
are equally open to the same strategy — learning from, and empowering, nurse leaders on their staffs to help
address the nursing shortage?
According to the Institute of Medicine, nurses are the health care professionals most likely to intercept medical
errors, which cost hospitals nationwide $3.5 billion annually. Nurses have in-depth understanding of the patient
care process and can tell a board which quality improvement and patient safety efforts might be most effective
in reducing medical errors. Nurses manage the entire care delivery process, interact more frequently with
patients and their families and keep the entire caregiver team working together effectively. A nurse brings a
different perspective. And a nurse can tell you what will really work at 2 in the morning.
A recent look at a recent classified ads section highlights the fact that a nursing shortage is a reality. The
competition between large military medical centers (Brooke Army and Wilford Hall) and the private sector for
nurses has created a large, transient nursing population of contract workers; they understandably look for the
organizations offering the best incentives. But this doesn't give us the stable, long-term work force that every
health system needs to meet the highest standards of patient care. Nurse leaders are best equipped to
understand why nurses leave and strategies for getting them to stay. Doesn't it make sense to include nurses
in the executive level decisions about how to recruit and retain nurses?
Today's nurse is often educated in a diversity of fields. They are also likely to have key characteristics that
provide value to a board such as a willingness to be highly engaged in the decision-making process, expert
facilitation skills, the ability to get along with others and strong relationships within the community. In the
Army Nurse Corps, we believe that nurses who are vested in the organization have a direct correlation to
improved patient care, safety and customer satisfaction. And we're proud to say that, even in such a
competitive environment, the Army Nurse Corps has met its nurse recruiting and retention goals for the first
time in the last five years during this past fiscal year.
Involving nurses in executive-level decisions is the optimal way to obtain critical input on management issues
or quality improvements. Health care leaders in San Antonio should use the example set by leaders in the
10
Army Nurse Corps and acknowledge the unique contribution nurses can make in governance positions and look
within their communities to find candidates who can broaden the perspective of their governing boards.
Justin Woodhouse is the officer responsible for recruiting nurses for the U.S. Army across a 10-state area.
3
Tackling Human Resources in Africa
The Scientist
01/2009
Developing countries are suffering severely from a lack of human resources in medicine and the biomedical
sciences. Africa in particular has a crisis, with many countries experiencing chronic shortages of biomedical
engineers, medical and research laboratory technicians, medical doctors and basic scientists. The problem was
officially acknowledged at an emergency meeting in Douala, Cameroon, in June 2007, attended by delegates
from 18 west and central African countries.
Several initiatives have now been launched, including one in our country of Cameroon. Measures at the
national level include more competitive salaries and part-time positions for Cameroonians or experts of
Cameroonian origin working in developed countries. The part-time opportunity allows experts to keep their
positions in developed countries while spending several weeks to months every year working in Africa. This
program is being implemented at our institute, the the Chantal Biya International Center for Research and
Prevention of HIV/AIDS (CIRCB).
Launched in February 2006 by Chantal Biya (the first lady of the state) with the support of eminent researchers
such as Luc Montagnier, Robert Gallo and Vittorio Colizzi, the CIRCB has sought solutions to the crisis in human
resources from the outset. The first scientists recruited were lured back from Italy, in part by state-of-the-art
equipment, competitive salaries (compared to regular civil servants) and open-ended contracts. CIRCB
maintains strong partnerships and collaborations with eminent Italian scientists and institutions.
Notwithstanding the success of CIRCB, it has been difficult to attract highly qualified Cameroonians to positions
in research institutions and universities in the country. While the package currently offered at CIRCB is
attractive to professionals who are at the early stage of their career, it is less attractive to advanced experts
who are established in developed countries and in many cases hold leadership positions. For this other group of
émigré professionals, returning to settle back home permanently may not be a realistic option. Nonetheless,
many overseas researchers remain strongly attached to their country and an increasing number have made
career-changing decision to abandon basic science for applied research which is a lot more relevant to the
research environment back home. In doing so, they can help develop skills that are needed throughout Africa
without the need to permanently relocate.
The CIRCB will give émigré professionals short-term consulting contracts. Some tasks, such as grant and
manuscript writing, conference participation, research with collaborating institutions, can be performed abroad
while other tasks—laboratory work, supervision and auditing, transfer of new technologies and knowledge and
training of staff—are performed during short visits at the CIRCB.
Such arrangements are "win-win" situations. For the consultant, spending 2 to 8 weeks in his home country
that he may have left many years ago as a student is an opportunity to make a significant contribution.
Indeed, having a professional linkage with his/her home country is usually more highly valued than the
remuneration associated with it. For the host institution, these agreements provide access to expertise that is
not readily available on the ground but is absolutely necessary for achieving its goals.
The first phase of this approach will soon be evaluated with a comprehensive assessment of the contribution
made by émigré scientists and others with skills needed at the CIRCB. Such a review will suggest adjustments
with an emphasis on promoting both productivity and the CIRCB competitiveness at the international level.
We anticipate important policy gains through this initiative to contribute to the mitigation of the effects of
"brain drain" throughout developing countries.
Odile Oukem-Boyer, Giulia Cappelli, and Pierre Fouda are a part of the Chantal Biya International Center for
Research and Prevention of HIV/AIDS (CIRCB) in Yaounde, Cameroon; Appolinaire Djikeng is a part of the J.
Craig Venter Institute in Rockville, Md.
4
Coahoma CC receives $1.99 million federal grant
Fort Mill Times, SC
18/01/2009
JACKSON, Miss. — The U.S. Department of Labor has awarded a nearly $2 million job training grant to
Coahoma Community College for health care training programs.
The funding was among the nearly $123 million in federal grants awarded to 68 community colleges and
community-based institutions.
The Department of Labor announced the funding Saturday.
Officials say the $2 million will allow Coahoma Community College to produce qualified health care workers to
help eliminate the shortage of workers in the industry.
11
The 68 grants will support projects in 36 states under President Bush's Community-based Job Training Grants
Initiative.
5
Are would-be health care workers
Michigan Business Review
15/01/2009
by Lynn Stevens | Business Review Western Michigan
For at least four years, the state has been telling Michiganders that health care is a great career field. Job
openings are plentiful and the future looks stable.
Suddenly-unemployed people in other fields, notably manufacturing, heard the message. However, despite
reported shortages of qualified applicants, getting into some training programs can require waits of several
months or even a couple of years.
Downsized workers from Muskegon-area manufacturing and other businesses are arriving at Baker College of
Muskegon's door, looking for new career fields, said President Mary Ann Herbst. Enrollment is really strong for
the semester that began this month, she said.
"They're saying, 'My job doesn't exist anymore, maybe it's time for me to look at doing something else,'" she
said. "And they're looking for something they can do relatively quickly, and the majority of our programs are
two-year programs."
Admission to the new registered-nurse program is highly competitive, she said, and only people at the same
point in their prerequisite courses may apply. The college cannot take a student who is on a waiting list at
another school, she said.
For jobs such as nursing that require licensing, there are caps on the number of students an accredited
program can accept, Herbst said. Each licensed field has its own accrediting body that sets a size limit on a
given institution's classes.
"They don't want any one school to saturate a market," Herbst explained. "They try to monitor it so we have
various numbers of graduates from various sections of every state.
"We watch the competition, as well -- the other schools that are providing programs -- so we don't produce
graduates who can't find employment."
Baker College of Muskegon makes a five-county needs assessment before starting any career program.
"The last thing we want to do is produce graduates and have nobody hiring," she said.
Lake Michigan College in Benton Township upped admissions requirements for its nursing programs and saw its
graduation and hiring rates rise sharply. So many of its graduates are working for Lakeland Healthcare, the
May graduating class will find only a handful of openings, said Robert Harrison, interim president of the
community college.
Harrison worked in health care before changing to an education career. He was president of Pawating Hospital
in Niles, now part of Lakeland. He began his health care career as an emergency medical technician.
"The advisers here (at LMC) send me all the calls they get for paramedic programs," Harrison said. "I ask them
if they've ever been on an ambulance. They want to commit years of their lives to a program they think they
might like."
People who think they want to work in those types of jobs would do better for themselves and the health care
industry if they had some firsthand knowledge of what's involved before choosing a new path.
Some people find the work too physically or emotionally demanding, Harrison said. Others leave the field after
four or five years.
"When you look at the registered nurse, for example, society's made a huge investment in them," Harrison
said. "Tuition doesn't pay all the costs. When we invest all that time and money in them and it doesn't work,
everyone loses."
There are other types of jobs in health care that may be better long-term fits, Harrison suggested.
"For every front-line soldier there's a huge infrastructure behind the lines," he said.
"There's the same type of pyramid in a hospital."
People outside the industry may define health care jobs only as those related to direct patient care, such as
doctors, nurses, paramedics or therapists. Redefining a health care job may enable a career changer to enter
the field quicker.
"They don't know there are I.T. folks, billing-and-coding folks, radiology technicians, people who perform
sterile processing,, radiology," said Craig Nobbelin, regional skills coordinator for the West Central Michigan
Health Care Regional Skills Alliance, hosted by Alliance for Health in Grand Rapids. Sterile processing is an
example of a process that might look familiar to anyone with a background in assembly work, he said.
"If folks have been in manufacturing where they've had quality control, they could take that step (to sterile
processing) without much education," Nobbelin said. "From there, they could move into a surgical
technologist's position or nursing. It's just a career ladder, where you could take these steps. There's a whole
range of different skill sets that are required to operate this little city known as a hospital system."
The Regional Skills Alliance also recognizes that not all people interested in health care will be content with the
reality of many types of jobs. It is developing a guidance process, using the ACT WorkKeys tests and a certified
career coach, to help displaced workers find which types of jobs will work.
6
12
UN says Gaza hospitals in crisis
Associated Press
17/01/2009
By TAMER SALIBA and PATRICK QUINN – 2 days ago
GAZA CITY, Gaza Strip (AP) — The medical system in Gaza is close to being overwhelmed and the Palestinian
enclave faces a humanitarian catastrophe unless a cease-fire is reached soon, a senior U.N. health official said
Friday.
Sixteen health facilities, including hospitals and clinics, have been damaged by shelling and fighting during the
3-week-old Israeli offensive, said Tony Laurance, head of the World Health Organization office in Gaza.
The attacks are a "grave violation of international humanitarian law," Laurance said by telephone. "If this
continues it will be a humanitarian catastrophe, especially for the health care system."
On Friday, health workers went through the smoldering wreckage of the five-story Al Quds hospital run by the
Palestinian Red Crescent Society, which was hit by three Israeli shells the day before.
There was nothing left to salvage inside the blackened hulk.
"They shelled the building, the hospital building. It caught fire. We tried to evacuate the sick people and the
injured and the people who were there. Firefighters arrived and put out the fire, which burst into flames again
and they put it out again and it came back for the third time," paramedic Ahmad Al-Haz told Associated Press
Television News outside the building.
Khaled Abu Zeid, a medic reached by phone at the hospital Thursday, said the attack set the pharmacy ablaze
and about 400 patients and staff were briefly trapped inside the main building.
Laurance said most of the patients were transferred to Gaza's City's already crowded Al Shifa hospital.
Israeli officials declined to comment. In the past, the Israeli army has accused Hamas militants of putting
people at risk by either firing from densely populated areas or using civilians as human shields.
The Red Cross movement condemned the shelling of the hospital.
The damage caused was "completely and utterly unacceptable based on every known standard of international
humanitarian law," the International Federation of Red Cross and Red Crescent Societies said in a statement
issued in Geneva.
More than 1,100 Palestinians have been killed and 4,900 wounded in the assault Israel launched against Gaza's
Hamas rulers to halt Palestinian rocket fire on Israel. Thirteen Israelis have been killed and more than 70
wounded since the offensive began Dec. 27.
"These latest attacks on hospitals in Gaza are an outrage and have put at risk the lives of patients and staff
and prevented access to health care for a system that is already coping with a flood of seriously wounded
people," Laurance said.
He said 13 medical workers have been killed and 22 wounded during the offensive, and that 16 ambulances
were destroyed.
"Emergency rooms, intensive care wards are already at maximum capacity. In terms of beds we are almost
there," Laurance said.
Gaza's health system will face a long-term burden, he warned. "We have an extensive number of serious
injuries, amputations and head injuries that will have serious long-term repercussions."
Laurance said Gaza does not need more doctors or medicine.
"More doctors are likely to be a hindrance rather than help. General doctors are not necessarily helpful," he
said. "What we need is cash."
Quinn reported from Jerusalem.
© 2009 The Associated Press. All rights reserved
7
Lawsuits Filed Over Rule That Lets Health Workers Deny Care
Washington Post
16/01/2009
By Rob Stein; Washington Post Staff Writer
Seven states and two family-planning groups yesterday asked a federal court to block a controversial new
federal regulation that protects health workers who refuse to provide care that they find objectionable.
13
In three lawsuits filed in U.S. District Court in Connecticut, the states and groups sought an immediate court
order preventing the regulation from going into effect Tuesday and a permanent decision voiding the rule.
"On the way out, the Bush administration has left a ticking political time bomb that is set to explode literally on
the day of the president's inaugural and blow apart women's rights," said Connecticut Attorney General Richard
Blumenthal, who filed one of the suits on behalf of his state, California, Illinois, Massachusetts, New Jersey,
Oregon and Rhode Island. "This midnight rule is a nightmare for hospitals and clinics, as well as women."
Blumenthal's lawsuit challenges the regulation on several grounds, charging that it is too vague and overbroad
and conflicts with other federal laws and state laws. The Planned Parenthood Federation of America filed a
second suit on behalf of its affiliates, while the American Civil Liberties Union filed sued on behalf of the
National Family Planning & Reproductive Health Association, which represents many state and county health
departments, among other providers.
"We filed this lawsuit today on behalf of the millions of women whose health care has been put in jeopardy by
the Bush administration's parting shot at women's health," said Planned Parenthood President Cecile Richards.
"The courts must strike down this unconscionable, unconstitutional last-minute midnight rule."
Rebecca Ayer, a spokeswoman for the Department of Health and Human Services, which issued the regulation
in December, said officials "have not had an opportunity to review the lawsuits, and we will respond to the
court on any pending litigation. The department followed appropriate procedures to put the regulation in place,
and the regulation is fully supported by law."
The regulation empowers federal officials to cut off federal funding for any state or local government, hospital,
health plan, clinic or other entity that does not abide by existing federal laws requiring them to accommodate
doctors, nurses, pharmacists and other employees who refuse to participate in any care they consider
objectionable on ethical, moral or religious grounds.
Conservative groups, abortion opponents and others sought the rule to safeguard workers who refuse to
provide such care from being fired, disciplined or penalized in other ways, and they defended the regulation
yesterday.
"The regulation is important, because we increasingly are seeing discrimination against health-care personnel
who hold religious beliefs having to do with abortion and contraception," said David Stevens, chief executive of
the Christian Medical & Dental Associations. "Unless these conscience rights are protected, people are going to
be driven out of health care."
Women's health advocates, family-planning proponents, abortion rights activists and others say it will create a
major obstacle to providing many health services, including abortion, emergency contraception for rape
victims, family planning, infertility treatment and end-of-life care, as well as possibly a range of scientific
research.
President-elect Barack Obama has voiced objections to the regulation and could repeal it, and legislation has
been introduced in Congress to block the rule, but both of those steps could take months to complete
"We are seeking a court order as quickly as possible," Blumenthal said. "We need this immediate order to
prevent confusion and chaos."
© 2009 The Washington Post Company
8
Study: Clinic staffing at critical low
RecordNet, CA
20/01/2009
By Joe Goldeen; Record Staff Writer
STOCKTON - California's nonprofit community medical clinics - a critical link in the maze of safety net health
care providers - are having a difficult time hiring and retaining skilled health care workers.
The problems are stressing clinics' resources and staffs when patient loads are growing due to rising
unemployment and fewer people with adequate insurance.
Findings from a new statewide survey of community clinics - funded through a grant from the California
Wellness Foundation - show that more than eight in 10 reported challenges involve keeping health positions
filled with qualified, trained personnel. Positions such as licensed vocational nurses, dental assistants and case
managers are among the hardest to keep staffed.
The allied health sector represents more than 200 job types in California that provide a range of diagnostic,
technical and therapeutic direct patient care and support services. Many include entry-level occupations
requiring a minimal educational investment, such as a certificate training program or an associate's degree
from a community college.
"Community clinics represent the front lines of our health care system," said Carmela Castellano-Garcia,
president and CEO of the California Primary Care Association, a membership organization of more than 700
nonprofit community clinics and health centers.
14
Mike Kirkpatrick is the chief executive officer of Stockton-based Community Medical Centers Inc., a Federally
Qualified Health Center that operates 10 medical clinics and one dental clinic in San Joaquin, Solano and Yolo
counties, with more than 325 employees and a $23million annual operating budget.
"Recruiting and retaining allied health workers, especially registered nurses for our clinics, has been a growing
challenge for us and other health care providers in the Valley counties," Kirkpatrick said, agreeing with the
survey results.
He said that while demand for health personnel by clinics, hospitals and other health facilities continues to
grow, the supply has not kept up.
"This has created a highly competitive marketplace for nurses and others, driven up salary and benefit costs
and placed more responsibility on nursing staff. Mandated nurse-to-patient-bed ratios further impact our
recruitment and retention," he said.
"Our clinics need not only qualified medical and dental assistants, social workers, nutritionists, but those with
the cultural and linguistic skills to effectively deliver care to the diverse communities we serve," Kirkpatrick
said.
Community Medical Centers' 11 clinics were visited 175,000 times last year by 52,000 patients. Of those, more
than half were Medi-Cal beneficiaries, and more than 30 percent were uninsured, paying for services out of
pocket on a sliding fee scale. More than two-thirds of Community Medical Centers' patients survive on incomes
of less than 200 percent of the federal poverty level, which in 2008 was $10,400 for an individual and $21,200
for a family of four.
According to survey responses, the scarcity is causing clinics to take on various measures to bridge the gap.
More than half (55 percent) of surveyed clinics reported having hired temporary workers or outsourced their
work, while 72 percent have had to increase overtime for existing staff.
Many clinics are finding innovative solutions to the challenge. Almost 70 percent are partnering with training
programs to provide clinical training sites, a popular practice among health care providers that helps increase
the pool of trained health workers.
"I am hopeful that we will see an expansion in training programs, especially here in the Valley, to begin to
reverse the shortage. Unlicensed allied health professionals are also difficult to recruit and retain," Kirkpatrick
said.
Susan Chapman of the Center for the Health Professions at the University of California, San Francisco, said
long-term planning is critical to solving the chronic health care worker shortage as the state's population ages
and the population adds 10 million residents by 2020.
"We tend to look at these shortages as short term. This is really about collaborative, long-term planning with
community colleges, private educators, key employers, policymakers, work force investment boards. The
regional approach is the best approach. All of these partners need to come together in a sustained way," said
Chapman, who is also an associate professor at the UCSF School of Nursing.
Contact reporter Joe Goldeen at (209) 239-6606 or jgoldeen@recordnet.com.
9
As Canada greys, health jobs soar
The Vancouver Province, Canada
18/01/2009
Iris Winston, For Canwest News Service
The greying of the population is setting off alarms through the health-care industry across the country.
Older people require more services even as an increasing number of older workers are reaching retirement
age.
"We are in a real crunch," says Nicole Jantzi, regional manager of recruitment for Vancouver Coastal Health.
"As the population ages, people need more care. The baby boomers are retiring, so we have a huge shortage
of people in most areas. Our whole service is based on people providing care and, without people, we can't
provide care."
The personnel issue is likely to worsen, and not just because of the retiring boomers. There are also fewer
graduates coming on stream, and these factors Jantzi says are why "recruitment is a priority" for Vancouver
Coastal Health and similar organizations across the country.
"We are hiring pretty well all the time for different types of positions," she says. "Nursing is No. 1 because
there is a huge shortage of nurses provincially, nationally and around the world, but there are also challenges
for other groups, some more critical than others."
15
Jacques Guerette, vice-president of communications at the University of Ottawa Heart Institute, says that while
the Heart Institute is "doing a very good job of keeping and attracting people, the health-care industry in
general is bracing for changes. In our case, we are looking at a continuing growth of 15 per cent a year in
patient load and a growing need of staff in a number of health-care disciplines."
He adds that job seekers are looking at "fairly healthy circumstances in health care" because, as well as the
increase in the patient load and the growing number of baby-boomer retirements, the mid-range of the
workforce is closer to retirement. Therefore, "the demand is not just for doctors and nurses but also for
managers, technicians and technologists."
Judy Clark, director of recruitment for B.C.'s Provincial Health Services Authority, and Darleen Odegard, a
human resources managing consultant with the Fraser Health Authority, echo the concerns about personnel
shortages in health care.
"More people are getting sick because the population is aging. Baby boomers are retiring and there are fewer
grads," says Clark. "We have to be far more creative in the way we offer an entry into corporate service or
clinical practice. We employ student nurses, take on residents, fellows and offer co-op opportunities. We also
recognize that seasoned operators are of tremendous value to us and have opportunities for many different
age groups and levels of experience."
"We need people in almost every area," agrees Odegard, noting that the three B.C. organizations frequently
place joint advertisements internationally in their search for qualified personnel.
All say that while the shortages are greatest for nurses, pharmacists and physiotherapists, the problem runs
through the entire industry. Filling jobs in this fast-growing employment sector is further complicated by the
increasing technical complexity of many health-care jobs.
Speech pathologists, medical radiation technologists and perfusionists are among the many available positions
that are difficult to fill. (Cardiovascular perfusionists are responsible for maintaining a patient's circulation and
respiration during surgery through the preparation and operation of extra-corporeal circulation equipment.)
As well as positions directly related to patient care, numerous other health-care jobs are available across the
board.
"Health care has become a profession that can offer the A to Z of job opportunities for such a diverse range of
talent," says Clark. "There are corporate service positions, everything from very exciting information
management and information technology roles to finance, human resources and communications."
"Typically, when you think of health care, you think of doctors, nurses and pharmacists first, but you don't
think of all the behind-the-scenes positions," says Jantzi. "The team approach in health care means that there
are many different options and careers."
Online applications are preferred.
"We encourage everyone to apply online," says Jantzi. "It's the fastest way to get a response and learn about
the company."
"Online applications are definitely preferred," agrees Clark. "Almost all health authorities have applicant
tracking systems in place. Applicants' resumés are attached to more than one application. Our policy is to
resumé-mine in our database for future positions. Before we spend a cent externally on advertising, my team
checks our database. We see it as our responsibility to the people who have applied to us to look at their
resumés first."
Potential jobs
Types of jobs in health care:
- Admitting clerks
- Biomedical engineers
- Diagnostic medical sonographers
- Health record administrators
- Human resources specialists
- Information services specialists
- Medical laboratory technologists
- Medical laboratory assistants
- Medical radiation technologists
- Mental health workers
- Nuclear medicine technologists
- Nurses
- Occupational therapists
- Ortho-technicians
- Paramedics
- Payroll clerks
- Perfusionists
- Pharmacists
- Pharmacy technicians
- Physicians
- Physiotherapists
16
- Practical nurses
- Purchasing clerks
- Radiology technicians
- Rehabilitation assistants
- Resident care aides
- Respiratory therapists
- Social workers
- Speech pathologists
- Speech/language technologists
- Sterile supply technicians
- Telecommunications specialists
- Trades specialists (e.g. electricians, maintenance workers, plumbers)
- Unit clerks
Nursing: Profession filled with possibilities
Types of nursing occupations:
- Emergency
- Geriatric
- Home care
- Intensive care
- Management
- Maternity
- Medical
- Neurosciences
- Operating room
- Pediatric
- Prevention
- Psychiatric
- School
- Street
- Surgical
- Teaching
-- Information from Vancouver Coastal Health
© The Vancouver Province 2009
10
Engager plus d'infirmières ne réglera pas la pénurie
La Presse de Montréal
19/01/2009
Ariane Lacoursière
Selon les calculs du ministère de la Santé et des Services sociaux (MSSS) du Québec, il faudrait engager 1807
infirmières pour éliminer les heures supplémentaires obligatoires. Mais même si le gouvernement engageait
demain matin des centaines d'infirmières, les listes d'attente continueraient de s'allonger, selon l'économiste
Mathieu Laberge du groupe de recherche CIRANO.
M. Laberge estime que le gouvernement évalue mal la pénurie d'infirmières. Sans entrer dans les détails, il
explique que si, un ajustement méthodologique était appliqué, la pénurie diminuerait de 16 à 18%.
Et si l'on prenait des mesures pour encourager les infirmières à travailler 10% de plus, la pénurie pourrait être
réduite jusqu'à 25%, croit-il.
Le MSSS estime qu'il manque actuellement 671 infirmières à Montréal. L'ajustement méthodologique et une
hausse de l'intensité du travail des infirmières feraient baisser la pénurie à 492, estime le chercheur.
Pour diminuer encore plus la pénurie d'infirmières, M. Laberge propose d'autres solutions. Il n'écarte pas l'idée
d'un ticket modérateur qui permettrait de réduire la demande de services.
Soumissionner les heures supplémentaires
Il croit aussi qu'un système de soumission des heures supplémentaires devrait être instauré dans les hôpitaux.
«Les infirmières intéressées à combler un quart de travail devraient déposer une mise, explique-t-il. Celle qui
aurait mis l'enchère la plus basse gagnerait. L'établissement paierait moins cher ses heures supplémentaires et
les infirmières intéressées seraient payées plus cher que le salaire normal.»
M. Laberge reconnaît toutefois que les conventions collectives des hôpitaux limiteraient de telles mesures. Il
rappelle que les infirmières à temps partiel qui voudraient travailler à temps plein devraient aussi être
accueillies dans le réseau.
Surtout, il martèle que l'embauche de centaines d'infirmières ne réglera pas à elle seule le problème des listes
d'attente. «On calcule combien ça prendrait d'infirmières pour éliminer les heures supplémentaires, mais
jamais on ne calcule combien il faudrait d'infirmières pour éliminer les listes d'attente», dit-il.
Back to top
17
Europe
1
Working on the Congolese front line
British Medical Journal
13/01/2009
Brigitte Breuillac
1 Médecins Sans Frontières
For Paul Kanulambi Walelu, dealing with gunshot wounds, open fractures, emergency caesarean sections,
peritonitis, and typhoid perforations is all in a day’s work. Or, quite often, all in a night’s work. For as well as
working seven days a week, Mr Walelu, an anaesthetic nurse, works every other night, for the medical aid
organisation Médecins Sans Frontières at the busy Rutshuru Hospital in North Kivu, the war-torn province on
the eastern border of the Democratic Republic of Congo.
It is Mr Walelu who in October last year helped the British surgeon David Nott in a forequarter amputation on a
16 year old boy who was close to death (BMJ 2008;337:a2958, 10 Dec, doi:10.1136/bmj.a2958). The boy had
previously had an operation to remove the upper part of his arm, but his stump was septic and gangrenous
when Dr Nott arrived for a month’s voluntary service at the hospital. Mr Nott made headlines across the world
for carrying out the operation with the help of instructions sent by text message from Meirion Thomas, a
consultant surgeon at the Royal Marsden Hospital, London, who was more familiar with the rarely performed
procedure.
Mr Walelu is nonchalant about what he describes as the "very intense" pace of work at Rutshuru Hospital. The
two surgical theatres deal only with emergencies, and their workload can multiply 10-fold when fighting in the
region intensifies, he says.
"We operate on an average of 350 patients a month for a wide range of surgeries. We do laparotomies
following typhoid perforations, peritonitis, or traumas. When there are gunshot victims we often find ourselves
with abdominal wounds and open fractures on upper and lower limbs. We also perform a lot of caesarean
sections and other obstetric emergencies. We do not take on elective surgery, only emergency operations,"
says Mr Walelu.
"Even when the fighting and violence intensified in October and November, and the number of wounded
increased dramatically, we still managed to work without interruption. Usually we see about 15 gunshot
injuries every month. But in just one day in October we saw 40 wounded people in two hours. Another day we
had 98 injured patients and had to sort them out according to the seriousness of their condition."
The two surgical teams at Rutshuru generally operate with three Congolese anaesthetists (two nurses and one
doctor) and two surgeons (one Congolese and one foreign visitor).
"We sometimes happen to have three surgeons, like in October [when Mr Nott was there], but this is rare,"
says Mr Walelu. "Occasionally we have an obstetrician gynaecologist. We work seven days a week, are on duty
every other night, and get two weeks off every three months."
Mr Walelu, who is aged 43, studied anaesthetic nursing in Kinshasa and has built up more than 13 years’
professional experience, working initially in the capital’s hospitals and for the last two years at Rutshuru for
Médecins Sans Frontières.
The operating theatres in the hospital are very well equipped, he says. "For the anaesthesia we have an
oxygen concentrator in each theatre, an anaesthetic machine with a halothane vaporiser and a ventilator, a
multifunction monitor (oxygen saturation, pulse, heart rate monitor, blood pressure, spirometer, and ECG
[electrocardiogram]). And also—which is rare in DRC [the Democratic Republic of Congo]—we have two syringe
drivers. Really we have everything we need to perform anaesthetics in good conditions. Moreover, the hospital
has a blood bank, and we have, on average, three units of blood available for each operation."
Adjusting to the different working methods of volunteer surgeons from all over the world, who like Mr Nott
tend to spend one month at a time working for Médecins Sans Frontières, might present extra demands for
surgical teams already working a gruelling schedule. But Mr Walelu welcomes the incoming doctors with the
same tranquil grace with which he appears to accept his demanding workload.
"Generally the expatriate surgeons are only here in Rutshuru for a month or so. The older and more
experienced surgeons perform all kinds of surgeries, while the younger ones tend to be more specialised, such
as in orthopaedic surgery, or general (visceral) surgery. But they adapt very quickly, and even if they have
different work methods it is never a problem for us. I am now used to this rhythm of work."
Cite this as: BMJ 2009;338:b63
________________________________________
The BMJ has chosen Médecins Sans Frontières as its Christmas appeal charity. Details on how to donate can be
found at www.msf.org.uk/bmjappeal.aspx.
4) Published 13 January 2009, doi:10.1136/bmj.b100
Cite this as: BMJ 2009;338:b100
2
UN provides $5 mln for Zimbabwe health workers
Reuters, UK
17/01/2009
By Nelson Banya
18
HARARE (Reuters) - The U.N. children's fund UNICEF said on Saturday it had set up a $5 million fund to
provide salaries for workers in Zimbabwe's ailing health sector.
Health workers in the southern African country -- where many public hospitals have been forced to close due to
a shortage of staff, drugs and equipment -- have been refusing to turn up for work, demanding salaries in
foreign currency.
They recently rejected a government offer of $50 for the lowest paid and $850 for doctors per month.
"I'm pleased to announce today that the United Nations will be providing $5 million for salaries for health
workers. We want to provide resources for health care workers so they remain in their jobs," UNICEF executive
director Ann Veneman told a news conference in Harare.
"It (the money) is going through a trust fund set up by some of the donors to provide incentives for health care
workers to continue turning up for work."
Veneman and UNICEF officials would not give details about how the fund would work, except to say payments
would be made to workers through the trust, not the government.
Veneman, who met President Robert Mugabe on Friday, is the first head of a U.N. agency to visit Zimbabwe in
three years.
She said a cholera outbreak that has killed more than 2,000 people was worsening.
"It is still not under control. It's still expanding in some communities. There's an issue of water and sanitation
systems, which are old. There's an urgent need to make sure people have access to clean and safe water,"
Veneman said.
"TIP OF THE ICEBERG"
U.N. figures show that 2,225 people have died from the cholera epidemic out of 42,675 cases. The outbreak
has piled pressure on politicians to bury their differences and try to ease the suffering of millions.
"The cholera outbreak is the tip of the iceberg. The economy in Zimbabwe is crumbling, with the highest
inflation rate in the world above 231 million (percent)," Veneman said.
"Over half the population is receiving food aid, health centres have closed and when the term starts there is no
guarantee that there will be enough teachers."
Critics blame the economic meltdown on government mismanagement, including the seizure and redistribution
of thousands of white-owned farms.
Mugabe, 84, in power since independence from Britain in 1980, says Western sanctions are the main cause of
the economic crisis and worsening humanitarian situation.
Political analysts say the establishment of a unity government between Mugabe's ZANU-PF party and the
opposition Movement for Democratic Change (MDC) is the best hope of reversing the economic slide and the
humanitarian crisis.
But power-sharing talks are deadlocked over the control of key ministries.
© Thomson Reuters 2009 All rights reserved
3
Gaza: Need for Protection of Medical Facilities and Personnel in Gaza: UN
Muslim News, UK
17/01/2009
Statement by Mr. Max Gaylard, the United Nations Humanitarian Coordinator for the occupied Palestinian
territory:
Yesterday witnessed the most intense fighting to date in the Gaza Strip, with Israeli ground forces advancing
deeper into densely populated areas, particularly Gaza City with an estimated population of 500,000 people.
Intense Israeli shelling hit the main UNRWA compound in Gaza City and three hospitals - Al Wafa, Al Fata, and
Al Quds.
Two ambulances were also hit by Israeli fire.
The Al-Quds hospital was surrounded by Israeli forces and the administrative and pharmacy buildings of the
hospital were shelled and badly damaged. Fires broke out and all of the patients and staff were evacuated. The
patients were later transferred to Shifa hospital.
This is not the first time that Gazan health facilities have been attacked and damaged.
19
Sixteen health facilities have been damaged and sixteen ambulances have been damaged or destroyed since
the start of the Israeli military operation on 27 December 2008 and 13 health workers have been killed and 22
have been injured.
Medical relief workers face extremely dangerous conditions when trying to reach injured Palestinians in combat
zones or areas made inaccessible by the Israeli army.
Densely populated Palestinian areas have been turned into combat zones, causing significant risk to the civilian
population, including hospitals, medical facilities and emergency relief workers.
The dangers posed by Israeli bombardment and fighting between the Israeli army and Palestinian militants
compound the already difficult situation of the Gaza health system.
Hospitals are already overwhelmed due to the volume of injured Palestinians and the severity of their wounds.
There is limited space in Intensive Care Units, shortages of staff, medicines, equipment, power and clean
water.
The situation for hospitals, medical workers and the injured in Gaza is alarming and deteriorating. Hospitals
must be protected and remain neutral areas under any circumstances. Civilians and the injured must have
access to medical care.
Violations of international humanitarian law by one party to a conflict offer no justification for non-compliance
by other parties. Allegations of violations must be fully investigated and those responsible held to account.
4
WHO chief says Gaza vulnerable to disease outbreak
Reuters, UK
19/01/2009
GENEVA, Jan 19 (Reuters) - Israel's offensive in Gaza has left Palestinians vulnerable to disease outbreaks, the
head of the World Health Organisation (WHO) said on Monday, warning that severe health risks will persist
beyond any ceasefire.
WHO Director-General Margaret Chan said in a speech she was "deeply concerned" about an interruption of
immunisations and other life-saving care in the densely populated territory.
There are now only 2,000 hospital beds for 1.5 million people in Gaza, and many hospitals and primary care
clinics serving civilians are badly damaged or destroyed, she said.
Some 1,300 Palestinians have died in the assault, which began on Dec. 27 when Israel launched air strikes on
Gaza to stop Hamas rocket attacks. Israel and Hamas separately declared ceasefires on Sunday, ending 22
days of fighting.
Israel put its dead at 10 soldiers and three civilians.
"Right now, we very sadly see ideal conditions for outbreaks of disease," Chan told the WHO's executive board,
citing health and sanitary risks from broken sewerage pipes, scarce drinking water, and garbage piling up in
the streets.
Cholera is among the deadly diseases that can spread quickly in such conditions.
The emergency needs of the wounded have overwhelmed the capacity of health facilities to treat those with
cancer, heart disease and diabetes, as well as pregnant women who now lack hospital beds to safely deliver
babies, Chan said.
"We need to be deeply concerned about the health of Gaza's civilian population," she said.
Chan also appealed for safe corridors to evacuate the severely wounded from Gaza as well as added protection
for health workers, hospitals, ambulances and humanitarian aid supplies.
The WHO's 34 member executive board is due to discuss the health situation in Gaza on Tuesday, as part of its
preparatory session for the agency's annual World Health Assembly in May. (For more information about
humanitarian crises and issues, please visit www.alertnet.org) (Reporting by Laura MacInnis; Editing by Nick
Vinocur)
5
Poor nations’ health systems must be boosted to improve maternal and newborn health, Unicef
says
British Medical Journal
15/01/2009
John Zarocostas
1 Geneva
20
Health systems in poor countries, especially in Africa and south Asia, need to be substantially strengthened to
improve care of the newborn and to reduce mortality in women during pregnancy and childbirth, a Unicef
report says. "Every year more than half a million women die as a result of pregnancy or childbirth
complications, including about 70 000 girls and young women aged 15 to 19," said Ann Veneman, Unicef’s
executive director.
"Since 1990, complications related to pregnancy and childbirth have killed an estimated 10 million women,"
she said.
The report says that most maternal and neonatal deaths can be averted through interventions that have been
proved to work.
Essential services that are needed, it says, include better nutrition and safe water, sanitation, and hygiene
facilities; adequate antenatal care; skilled assistance at delivery; basic and comprehensive emergency obstetric
and newborn care; postnatal care; neonatal care; and integrated management of neonatal and childhood
illnesses.
The report notes that severe infections often associated with unhygienic delivery practices and unsafe water
and sanitation "accounted for 36% of neonatal deaths in 2000."
Unicef and the World Health Organization recommend that all women have a minimum of four antenatal visits,
which enable them to receive interventions such as tetanus immunisation, screening for and treatment of
infections, and crucial information during pregnancy and delivery. The report says that "no substitute exists for
the assistance of skilled health personnel at delivery."
Most maternal deaths, says the report, are related to obstetric complications, including postpartum
haemorrhage infections, eclampsia and prolonged or obstructed labour, and complications of abortion.
Most of these direct causes of maternal mortality, it says, "can be readily addressed if skilled health personnel
are on hand and key drugs, equipment and referral facilities are available."
From 2000 to 2007, the report says, skilled health workers attended 61% of all births in the developing world,
but it adds that the regions with the lowest coverage—sub-Saharan Africa, with 45%, and South Asia, with
41%—also registered the highest maternal mortality.
It says that healthcare systems in many poor nations suffer from weak administration, low technical and
logistical capacity, inadequate investment, and a lack of skilled healthcare personnel.
"Scaling up key interventions—for example, antenatal HIV testing, increasing the number of births attended by
skilled health personnel, providing access to emergency obstetric care for mothers and babies—could sharply
reduce both maternal and neonatal deaths," the report says.
Ms Veneman said that a stronger focus on Africa and Asia, which together account for an estimated 95% of
maternal and about 90% of neonatal mortality, "is imperative to speed up progress on maternal and newborn
health."
The report says that advances in maternal and neonatal health "have not matched those of child survival,
which registered a 27% reduction in the global under-five mortality rate between 1990 and 2007."
UN inter-agency estimates for 2005 show that more than 99% of maternal deaths occurred in poor nations, of
which 265 000 were in Sub-Saharan Africa and 187 000 in south Asia.
The report says that a woman in the developing world has a 1 in 76 lifetime risk of death during pregnancy or
childbirth, whereas the risk in developed countries is just 1 in 8000. To help close this gap and to reduce infant
mortality the report recommends that essential services be provided through healthcare systems that integrate
home, community, outreach, and facility based care.
This will also require expanding the healthcare workforce, upgrading infrastructure, providing equitable
financing solutions, and social mobilisation.
"Social inclusion should be a priority in health systems development," the report notes, and it also argues that
removing direct charges to service users may markedly improve poor people’s access to care.
Cite this as: BMJ 2009;338:b120
________________________________________
The State of the World’s Children 2009: Maternal and Newborn Health is at www.unicef.org.
6
Lettre ouverte à M. le Président de la République
Coordination Nationale Infirmière - France
/01/2009
Monsieur le Président,
Consciente de votre attachement à faire accepter et appliquer par les Français les réformes que vous vous
êtes engagés à mener pendant votre mandat présidentiel, la Coordination Nationale Infirmière tient à vous
faire part de ses remerciements concernant le soutien aux professionnels soignants et en particulier à celui des
infirmières au cours de votre discours du 9 janvier 2009 à Strasbourg. Mais nous tenons également, et c’est là
le but de nos propos, à vous faire part de toutes les difficultés auxquelles notre profession est aujourd’hui
confrontée.
Suite aux dramatiques accidents survenus en cette fin d’année 2008, et la mise en examen prolongée d’une de
nos collègues, nous sommes en devoir pour notre profession, pour tous nos collègues de travail de vous
interpeller sur « le mal être » infirmier ainsi que sur la gestion budgétaire actuelle de nos hôpitaux qui se
traduit par des injonctions de retour à l’équilibre pour nos établissements alors que le principal poste de
dépense concerne le personnel (70% du budget). Ce retour à l’équilibre ne peut se solder que part des
suppressions de poste, de non remplacement de départ en retraite, les emplois en CDD non renouvelés…
21
Les services de soins sont au bord de l’asphyxie. Pour pallier à ce manque de recrutement et de remplacement,
les directions n’hésitent pas à fermer des lits, à réorganiser les temps de travail (travail en 12 h, coupé, heures
supplémentaires qui accroissent le manque de vigilance et diminuent les temps de repos). Par manque de
personnel, les agents sont dans l’impossibilité de participer à la formation continue qui a pourtant été rendue
obligatoire par le législateur.
Votre discours porte sur les moyens financiers mis par l’Etat ces 10 dernières années dans les dépenses de
l’assurance maladie. Ces moyens auraient augmenté de 50 % ! Mais cela n’est il pas dût à un accroissement
normal des besoins de santé, aux nouvelles technologies, aux molécules onéreuses, à l’allongement de la
durée de vie, au renouvellement du parc hospitalier ?
De plus, l’hôpital public est lui aussi confronté à la hausse du coût de la vie et notamment en ce qui concerne
le budget chauffage de nos établissements.
Vous déclarez que l’organisation est la clé qui ouvrira la porte à plus d’efficience pour l’hôpital public !
Permettez nous de penser et de souligner que depuis bien longtemps les infirmières sont organisées.
Organisées dans leur temps de travail, organisées pour leurs familles quand elles travaillent les dimanches et
jours fériés, les vacances scolaires… Mais quand vous croulez sous le poids des tâches à accomplir, que vous
n’avez plus le temps de prendre et de tenir une main que l’on vous tend ! Que vous n’avez plus l’impression du
travail bien fait ! Qu’humainement vous êtes dans l’impossibilité de répondre aux demandes des patients !
Alors, nous disons stop !
Aujourd’hui, Monsieur le Président, la coupe est pleine.
Si une réorganisation de l’hôpital public est nécessaire, elle doit se faire en concertation avec tous les acteurs,
en s’adaptant aux nouvelles techniques sans mettre en péril la prise en soins par des coupes franches
budgétaires qui ne prennent pas en compte notre quotidien hospitalier.
Sans ouvrir de polémique sur les accidents gravissimes qui ont été médiatisés au cours des fêtes de fin
d’année, nous vous demandons de veiller à ce que toute la lumière soit faite et que la chaîne de responsabilités
soit établie. Conscients que le risque zéro n’existe pas, nous demandons néanmoins à ce que des mesures
soient prises afin de prévenir et de tendre vers une sécurité maximale notamment en ce qui concerne le circuit
du médicament et l’étiquetage. Dans ce domaine, notre syndicat professionnel infirmier force de propositions,
demande à être entendu par notre ministre de tutelle Mme Bachelot.
Face aux dysfonctionnements croissants et généralisés à tous les hôpitaux, nous ne pouvons pas cautionner
des conditions de travail qui mettent en jeu la sérénité et la sécurité de notre travail, de nos patients et de
notre propre personne.
Nous ne pouvons accepter cela.
Aussi, par cette lettre et par la voix de milliers d’infirmiers nous vous demandons aujourd’hui Monsieur le
Président, de prendre les mesures indispensables pour enrayer cette dégradation des conditions de travail dans
le système hospitalier.
Il est impératif d’assouplir l’étau budgétaire de nos hôpitaux.
Il est indispensable d’appliquer des mesures que notre organisation syndicale revendique depuis plus de vingt
ans en faveur de la profession infirmière :
•
Une amélioration de nos conditions de travail et d’études en prenant compte notre demande
d’intégration de nos études au système LMD avec la création d’une discipline en sciences infirmières
•
Une adéquation entre les effectifs soignants et la charge de travail réelle
•
Une reconnaissance de notre travail, de nos compétences par une augmentation salariale
correspondant à nos responsabilités et à notre niveau d’études.
•
Une sensibilisation des différents partenaires médico sociaux avec une véritable prise en compte de la
parole infirmière (pharmacie, ergonomie…).
•
Un accès à la formation continue, clé de voute de soins efficaces et sécurisés.
•
Une spécialisation en psychiatrie (Master).
La réforme portée par Madame Bachelot au travers de la Loi Hôpital Patients Santé Territoire va être présentée
dans les prochains mois au parlement. Le renforcement des pouvoirs d’autonomie et de décision du directeur
d’établissement, création des ARS, les nouvelles formes de coopération entre professionnels de santé ne
peuvent servir de pansement sur un système déjà à la dérive.
Monsieur le Président, nous vous demandons de prendre en compte le malaise grandissant de l’hôpital public et
de ses personnels. Nous vous demandons de reconsidérer « le chantier en cours » et de porter des choix
politiques pour une santé à la hauteur de notre XXIe siècle
« Comme toujours en France, on ne regarde pas ce qui se passe dans le moteur, on dit qu’il faut plus ! » Et
bien aujourd’hui Monsieur le Président, le moteur des hôpitaux français est bien malade et si vous n’entendez
pas la souffrance exprimée par chacun de ses rouages, nous craignons vivement que le traitement annoncé ne
soit qu’un palliatif à l’effet bien peu antalgique !
Dans l’attente de votre réponse, avec nos respectueux hommages, nous vous prions d’agréer, Monsieur le
Président, l’expression de notre très haute considération.
Nathalie Depoire, Présidente CNI
7
Milburn is to head initiative to widen entry to medical training
British Medical Journal
14/01/2009
Adrian O’Dowd
1 London
22
The former health secretary Alan Milburn has been chosen to head a new commission for social mobility that
will aim to widen access to people from all backgrounds to professions such as medicine.
The need to widen the field for future doctors was underlined in a report commissioned by the Liberal
Democrat party and published on 12 January by the children’s charity Barnardo’s. It showed that a child’s life
chances still depend largely on background and parents’ earnings.
Prime Minister Gordon Brown announced at the weekend that Alan Milburn, Labour MP for Darlington and the
health secretary from 1999 to 2003, would head the government’s drive to boost social mobility.
Mr Milburn will chair a panel of representatives from the professions to bring forward proposals on what more
can be done. Issues the panel will consider include:
•
Financial obstacles to entry to and progression in the professions and ways to overcome them, such as
scholarships
•
The role of work experience as an entry route into the professions and in particular unpaid internships
•
Recruitment practices, and
•
Action to encourage new applicants and those seeking promotion.
The government’s drive to improve social mobility was outlined in a white paper published by the Cabinet
Office on 13 January (www.hmg.gov.uk/newopportunities/download.aspx).
Part of Mr Milburn’s task will be to ensure that professions such as medicine, the law, the civil service, the
armed forces, and the media recruit more young people from poorer backgrounds.
The BMA supports the commission’s intentions and said last year in a report called A Need for Change that the
medical workforce should be more representative of the diverse society it serves.
Louise McMenemy, a member of the executive of the BMA’s medical students committee, said that inequalities
in the education system meant that people from poorer backgrounds were less likely to become doctors.
She said, "If you look at the number of students that come from the lowest socioeconomic groups in
comparison with higher socioeconomic groups, the percentages are vastly different. There’s not one single
reason for that. It’s not just the case that people are in a lower socioeconomic group: it can be to do with
schooling or aspiration."
Ms McMenemy, a fourth year medical student in Guy’s, King’s and St Thomas’ School of Medicine, London, said
that some universities already had initiatives to widen access for students, such as running extended six year
courses.
"There are schemes running, but a lot more needs to be done to ensure we have doctors that represent the
population they serve. It’s going to take a lot of work," she said.
The Barnardo’s report said there was a dire need for such a drive.
Martin Narey, head of Barnardo’s, who chaired its inquiry, said, "Despite progress in reducing child poverty and
heavy investment in education, a child’s chances of success in Britain today are still largely dependent on the
background and earnings of its parents."
Cite this as: BMJ 2009;338:b116
________________________________________
A Need for Change is at www.bma.org.uk/images/Needforchangereport_tcm41-162833.pdf. The Barnardo’s
report, Report from the Independent Commission on Social Mobility, is available by e-mailing
info@socialmobilitycommission.org .
8
Health crisis in Zimbabwe is "man-made" and needs intervention from all UN states, report says
British Medical Journal
13/01/2009
Peter Moszynski
1 London
The collapse of Zimbabwe’s formerly world class healthcare system is a "man-made disaster," says an
emergency report from the US based charity Physicians for Human Rights. It says that life expectancy at birth
in the country has plummeted over the past 20 years, from 60 to 36, and it warns that the situation continues
to deteriorate, as the country no longer has any functioning public hospitals.
In the report’s preface Mary Robinson, former UN human rights commissioner, Richard Goldstone, former UN
chief prosecutor for Rwanda and Yugoslavia, and Archbishop Desmond Tutu say: "The Mugabe regime has used
any means at its disposal, including politicizing the health sector, to maintain its hold on power. Instead of
fulfilling its obligation to progressively realize the right to health for the people of Zimbabwe, the Government
has taken the country backwards, which has enabled the destruction of health, water, and sanitation—all with
fatal consequences."
The charity sent a delegation to Zimbabwe last month to investigate the collapse of the country’s healthcare
systems. It concluded that the "health and nutritional status of Zimbabwe’s people has acutely worsened this
past year due to a cholera epidemic, high maternal mortality, malnutrition, HIV/AIDS, tuberculosis, and
anthrax."
Frank Donaghue, chief executive of Physicians for Human Rights, said that although his team entered the
country legally and was transparent about its purpose of conducting a health assessment, the team members
had to go into hiding and secretly flee the country overland after state media announced their arrests.
Mr Donaghue believes that these actions were "a desperate attempt by Robert Mugabe to conceal the appalling
situation of his country’s people and to prevent the world from knowing how his government’s malignant
policies have led to the destruction of infrastructure, widespread disease, torture, and death."
23
The report points out that the continuing cholera epidemic "is an outcome of the health system’s collapse, and
of the failure of the state to maintain safe water and sanitation." It concludes that "this disaster is man-made,
was likely preventable, and has become a regional issue since the spread of cholera to neighbor states."
The report further claims that "the health crisis in Zimbabwe is a direct outcome of the violation of a number of
human rights, including the right to participate in government and in free elections and the right to a standard
of living adequate for one’s health and well being, including food, medical care, and necessary social services."
The researchers maintain that "a causal chain runs from Mugabe’s economic policies, to Zimbabwe’s economic
collapse, food insecurity and malnutrition, and the current outbreaks of infectious disease.
"These policies include the land seizures in 2000, a failed monetary policy and currency devaluations, and a
cap on bank withdrawals."
The preface’s authors describe the report as "yet another wake-up call to Zimbabwe’s neighbors and all UN
member states for urgent intervention to save lives and prevent more deaths. These findings add to the
growing evidence that Robert Mugabe and his regime may well be guilty of crimes against humanity."
Cite this as: BMJ 2009;338:b100
________________________________________
Health in Ruins: A Man-Made Disaster in Zimbabwe is available at www.phrusa.org. Video footage of the
delegation’s visit to Zimbabwe is at www.youtube.com/watch?v=iaXowZh-XCM&fmt=22.
9
Health is a human right
British Medical Journal
15/01/2009
Editor's Choice
Fiona Godlee, editor, BMJ
fgodlee@bmj.com
Alex Jadad and Laura O’Grady’s call for a debate on the definition of health has stimulated fascinating
responses to both their editorial (doi:10.1136/bmj.a2900) and their blog
(http://blogs.bmj.com/bmj/2008/12/10/alex-jadad-on-defining-health). I particularly like Richard Smith’s
response to the blog, in which he suggests that health is "the capacity to do what matters most to you"
(http://blogs.bmj.com/bmj/2009/01/05/richard-smith-can-poetry-define-health).
Two other responses appear in this week’s Letters. Peter Mansfield recalls the Peckham experiment in London
in the 1930s and 1940s, which aimed to investigate the nature of health (doi:10.1136/bmj.b83). An expanded
vision of health is unlikely to come from within medicine, he says. "Economic and climatic constraints will force
healthy living on us eventually, or we shall perish." Peter Davies calls on us to embrace the wider context of
health beyond the absence of disease (doi:10.1136/bmj.b28). "For too long we as a society have allowed
politicians to get away with shunting health off to a ‘medical domain,’ thus avoiding focus on the large scale
social and political forces that create health and illness."
There is no doubting the political forces at play in the world’s major conflict zones. Médecins Sans Frontières’
annual list of the most neglected humanitarian disasters, released last month
(http://doctorswithoutborders.org/publications/topten), highlights Somalia, the Democratic Republic of Congo,
Iraq, Sudan, Pakistan, Zimbabwe, and Burma. That was before this month’s terrible events in Gaza. All these
disasters are man made, a point hammered home in an emergency report from the US based charity
Physicians for Human Rights on the collapse of Zimbabwe’s healthcare system (doi:10.1136/bmj.b100). The
authors say that Zimbabwe’s health crisis is a direct result of violations of human rights, including the right to
vote and the right to a standard of living adequate for health.
In the Democratic Republic of Congo, at the hospital made famous last month for the text messages that
guided a forequarter amputation by a surgeon working for Médecins Sans Frontières (doi:10.1136/bmj.a2958),
there is no elective surgery, only emergency operations, with sometimes nearly 100 casualties a day
(doi:10.1136/bmj.b63). Meanwhile in Gaza, medical workers are overwhelmed by the number of casualties,
reports John Zaracostas (doi:10.1136/bmj.b87). They are hampered by shortages of critical medical supplies
and fuel as Israel’s air and land offensive adds to the already debilitating consequences of a long blockade.
What can the world’s medical profession do in the face of such powerful, longstanding, and complex political
forces? Shrink back into the confines of the medical model? Or, as I believe we must, embrace the wider
responsibility of championing the right to health in all parts of the world. For this we do need a workable
definition of health however hard it is to achieve. And for my part I endorse last week’s call in the Lancet
(doi:10.1016/S0140-6736(09)60015-5) for all doctors to see themselves as médecins sans frontièrs—doctors
without borders—and to live up to this name "by calling on their national governments and the international
community—perhaps through their national medical organisations—to ensure that civilians injured or affected
by conflict receive the medical attention they need."
Cite this as: BMJ 2009;338:b136
10
Health workers vote to strike if HSE forces changes
Irish Times
21/01/2009
MARTIN WALL, Industry CorrespondentABOUT 9,500 health sector workers in Dublin have voted
overwhelmingly for industrial action in the event of the Health Service Executive (HSE) seeking to introduce
changes in pay and conditions without agreement.
24
Ninety-eight per cent of members of Siptu’s Dublin health services branch, who include porters, caterers,
security staff and healthcare assistants, voted in favour of industrial action.
No date has been set as of yet for the commencement of any industrial action.
Siptu health sector organiser Paul Bell said the impetus for the ballot had come from comments made by a
senior HSE manager to the effect that health sector workers were inefficient, too expensive and inflexible.
“He went on to say he intended tearing up or ignoring collective agreements, which enshrine our agreed terms
and conditions of employment, and . . . to ignore existing third-party procedures for resolving disputes,” he
said.
“This was tantamount to a declaration of war . . . We had only one way of preparing for such an attack and
that was to obtain a strike mandate,” Mr Bell said.
The vote for industrial action comes against the backdrop of proposals by HSE management to introduce
significant changes in working practices for staff as part of a bid to save more than €320 million this year.
Mr Bell said that the timing of the attack on his members by the senior manager coincided with efforts by
senior trade union officials to negotiate a framework document and protocol agreement, which would allow new
efficiencies to be introduced on a partnership basis, with the right to full consultation for workers affected in
each hospital and agency.
An outline of this framework was reached between health sector unions and management over Christmas.
However, its implementation was conditional on talks with the Government on a number of high-level policy
issues.
Mr Bell said that as a result of the ballot result, the union was now equipped to protect members “should
management implement their threats”.
He said that his members were willing to engage in far-reaching discussions with employers and would not be
found wanting. He said that the proper way to do this was not “by declaring war on workers but by a speedy
and concentrated engagement to identify and address issues”.
“Our members are not afraid to make sacrifices in order to protect and improve the health service for the
general public. We have already demonstrated our willingness to help our nation’s economy by accepting a
one-year pay freeze. However, it is important for health service employers to recognise that sustainable
progress can only come through dialogue and engagement.
“We therefore call on the HSE to continue to engage with us to bring about a mutually acceptable outcome to
the great crisis we are facing,” he said.
Back to top
Latin America & Caribbean
2
SALUD-PARAGUAY: Hola Roma, adiós dengue
IPS-Latin American/Caribbean
23/01/2009
Por David Vargas
ASUNCIÓN, abr (IPS) - Mientras en el pasillo del Hospital de Clínicas de Paraguay decenas de pacientes con
síntomas de dengue aguardan ser atendidos, en la sala de enfermeras hay una fiesta. Mirian López, licenciada
con varios años de experiencia y especializada en terapia intensiva, acaba de saber que hay un puesto
esperándola en Italia.
López se sumará muy pronto al contingente de casi 400 enfermeros paraguayos que desde 2000 han emigrado
a ese país europeo para trabajar en hospitales públicos y privados.
Esa cantidad representa más de 10 por ciento de la fuerza laboral de un sector que, en los registros del
Ministerio de Salud Pública, comprende 3.500 puestos entre enfermeras, auxiliares de enfermería y de
obstetricia y asistentes técnicos.
De ellos, sólo 1.567 puestos son para licenciadas en enfermería. Pero como la ley permite al personal de salud
ocupar hasta dos puestos en diferentes servicios, las enfermeras profesionales son menos aun, explicaron
fuentes del Ministerio.
Lo que para López es una satisfacción, para las autoridades sanitarias es una preocupación creciente, más aun
tras el brote de la epidemia de dengue.
La migración del personal sanitario hacia Europa y Estados Unidos ha acentuado el ya grave déficit de recursos
humanos calificados en los hospitales públicos.
25
En Paraguay, según datos oficiales, el promedio de enfermeras es de 1,2 por cada 10.000 habitantes, muy por
debajo de otros países de la región, como Argentina o Uruguay, donde la media es de 12 por cada 10.000,
apenas por encima de la proporción mínima recomendada por la Organización Mundial de la Salud (OMS), de
10 por cada 10.000 personas.
Los servicios más afectados por la fuga de profesionales son clínica médica y terapia intensiva, explica a IPS la
presidenta de la Asociación Paraguaya de Enfermeras (APE), María Concepción Chávez.
Los cupos vacantes se llenan, en el mejor de los casos, con auxiliares de enfermería sin experiencia o técnicos
sin suficiente preparación. "La funcionalidad de muchos sistemas está seriamente amenazada. Tenemos varias
unidades de terapia intensiva cerradas por falta de personal, y la especialización lleva entre dos a tres años",
se lamenta.
Desde que se declaró la epidemia de dengue a principios de este año, el Ministerio de Salud registró 25.856
casos de la forma clásica de la enfermedad y 52 del tipo hemorrágico. Hay 14 muertos, y más de 3.535
enfermos tuvieron que ser hospitalizados. Aunque las autoridades afirman que la situación está bajo control, la
cantidad de afectados es de unos 200 por día.
La representante de la Organización Panamericana de la Salud (OPS), Carmen Serrano, fue de las primeras en
dar el toque de alerta. Ella califica el fenómeno de la emigración de enfermeras como grave, aunque no
exclusivo de Paraguay. "A nivel mundial hay una crisis, porque este recurso humano en salud no es reconocido
en los países en desarrollo. Hay países como Bolivia, donde la situación es mucho peor", dice a IPS.
El problema fue abordado en la Asamblea de la OMS el año pasado, cuando se debatió la necesidad de
implementar un sistema de resarcimiento a los países más pobres por el "robo" de sus recursos humanos de
salud por parte de las naciones ricas. Serrano señala que lo ideal sería devolver "con algunos otros
componentes e insumos a los países que están perdiendo al personal de salud".
Según la APE, el salario de una enfermera en Paraguay ronda en promedio los 300 dólares. Setenta por ciento
de las que forman parte de la red pública trabajan bajo el régimen de contratación, es decir, no tienen seguro
médico, jubilación ni estabilidad laboral, y deben renovar sus contratos cada seis meses o un año.
En Italia, el contrato inicial de un año, renovable, le asegura a López un sueldo de 1.500 euros (unos 2.000
dólares), e incluye además seguro médico, vacaciones pagas por 30 días y aguinaldo.
"Es una oportunidad única", dice a IPS esta enfermera que durante un año tomó clases intensivas de italiano,
uno de los requisitos excluyentes para obtener el trabajo. Los postulantes también deben someterse a un
proceso de validación de las matrículas profesionales y a un riguroso examen de admisión preparado por el
Colegio Italiano de Enfermeras.
Los contactos se logran a través de firmas reclutadoras como Obiettivo Lavoro, una consultora italiana que
hace dos años se instaló en este país y que también cuenta con sucursales en Bolivia, Perú y Brasil.
Esta empresa se encarga de explorar las oportunidades laborales en los hospitales italianos, reclutar y
adiestrar al personal en Paraguay y hacer los tramites de visa y permisos laborales correspondientes.
"Las enfermeras paraguayas tienen una excelente llegada al paciente. Entre las sudamericanas es la
mayormente considerada, es muy buscada en hospitales y clínicas por su alta capacidad profesional", dice a
IPS el representante de la firma en este país, Jorge Romero.
De acuerdo con la OMS, la demanda insatisfecha global de trabajadores de la salud supera los cuatro millones.
En los países industriales, la escasez de enfermeras es mayor debido sobre todo al envejecimiento de la
población. La organización estima que en Italia, por ejemplo, se necesitan 50.000 enfermeras para cubrir las
necesidades, en Canadá, 60.000, y en Estados Unidos, 168.000.
Y esta brecha, advierte la OMS, irá en aumento a medida que el promedio de vida se prolongue.
El sindicato de estos trabajadores de la salud en Paraguay quiere poner énfasis en la capacitación. "Se necesita
más y mejor personal de enfermería, para que la profesión no envejezca ni se descalifique", dijo la titular de la
APE. Pero el problema es complejo, sobre todo en un país como éste, donde anualmente el promedio de
licenciadas en enfermería que se incorporan al mercado laboral no alcanza siquiera a 200, según datos
oficiales.
La formación de una enfermera en la Universidad Nacional de Asunción tiene un costo aproximado de 14.000
dólares por cuatro años de carrera. La mayoría de los reclutados para trabajar en el exterior son egresados de
esa institución, que, pese a los problemas de presupuesto e infraestructura, es el principal centro de formación
profesional en este campo.
La titular de la APE afirma que la principal preocupación del sindicato es que la mayoría de las enfermeras que
emigran tienen entre 30 y 35 años. "Estos profesionales, dentro de 10 a 15 años regresarán al Paraguay sin
posibilidades de trabajo, sin jubilación, sin seguro social, y eso va a generar inestabilidad social", lamenta.
Pero ese pronóstico es secundario para Mirian López y otros 21 postulantes que están en lista de espera de la
agencia Obiettivo Lavoro para viajar e iniciar una nueva vida en Italia. "Con el sueldo que gano acá no voy a
ningún lado, y si bien me es difícil dejar a mi familia y mis amigos, el sacrificio vale la pena", señala López.
26
La fiesta de despedida termina rápidamente. El dengue no da respiro, y la cantidad de pacientes aumenta
conforme pasa la mañana. Al salir, López no puede ocultar su alegría: "Ciao Roma, arrivederci dengue".(
3
Dilos instruye a la Alcaldía contratar a personal para hospitals
El Deber, Bolivia
16/01/2009
El Directorio Local de Salud (Dilos) emitió una resolución en la que instruye al gobierno municipal de Santa
Cruz de la Sierra la contratación de médicos y trabajadores de salud para paliar la carencia de personal que
confrontan los hospitales públicos, que tocó fondo con el problema de la falta de reemplazos para vacaciones y
bajas.
De acuerdo con el Dilos, los nuevos funcionarios deberán ser contratados por un año, debiendo el Servicio
Departamental de Salud (Sedes) realizar en este lapso las gestiones ante el Ministerio de Salud para la
dotación definitiva de ítems, que supla la necesidad de reemplazos en todos los nosocomios públicos.
Asimismo, ordena a la Prefectura a través del Sedes cubrir las deudas por reemplazo de personal médico y
paramédico, previa verificación de los casos.
Según el Dilos, un estudio sobre los recursos humanos determina que los hospitales precisan
aproximadamente 167 nuevos funcionarios de salud, pero el Sedes definió que ese número puede reducirse a
100. /DO
4
Denuncian falta de personal que pueda brindar primeros auxilios
ABC Digital, Paraguay
16/01/2009
Guillermo Trovato Fleitas denunció a nuestro diario que el pasado domingo 11 de enero, una niña que estaba
andando en bicicleta se accidentó en el Parque de la Salud del IPS.
“Ella sufrió un golpe en la cabeza y se encontraba en el piso. Todos los que nos encontrábamos cerca acudimos
al auxilio, y felizmente se encontraba presente un estudiante de medicina del 5° año”, indica la nota remitida
por el denunciante.
“Luego de pedir camilla, dado que el percance ocurrió lejos de la entrada, se necesitaban conocimientos
médicos para alzar a la niña. ¡Y aquí ocurre lo más lamentable! La camilla es traída por dos personas
aparentemente paramédicos; y digo paramédicos, porque al llegar uno de ellos pregunta a los presentes:
¿quién es médico aquí? Pregunta a lo que un joven respondió: ‘Yo soy estudiante del 5° año de Medicina’. El
paramédico ni corto ni perezoso le espetó diciendo ‘Bueno, encárguese usted”, expresa la denuncia.
En la carta también se relata que el estudiante guió el procedimiento para alzar a la pequeña y que para
movilizarla se necesitaba un collar cervical “que también brilló por su ausencia”.
“La ambulancia llegó cinco minutos después de ocurrido el percance, con la niña ya ubicada en la entrada”,
añadió.
Al respecto, la Dra. Teresa León, directora interina del parque, indicó que en el sitio existe un puesto de
enfermería, con un personal que realiza atención a nivel comunitario como toma de presión, etc. Añadió que
las enfermeras están capacitadas como para brindar los primeros auxilios y deben llamar a la ambulancia para
derivar al accidentado a un centro asistencial.
León indicó que, en el caso de que se trate de un asegurado, acuden las ambulancias del Hospital Central y lo
derivan hasta allí. Este mecanismo también se utiliza en los casos de los no asegurados cuyos cuadros
representen un peligro de muerte.
En caso contrario, aquellos que no son beneficiarios del seguro social son trasladados en una ambulancia del
Ministerio de Salud Pública hasta el Centro de Emergencias Médicas, mediante un convenio que tiene el parque
con el MSP.
TEMPORADA ALTA
En estos días, el Parque de la Salud del IPS registra entre 700 a 1.000 visitantes por día, que aprovechan el
local para realizar caminatas, andar en bicicleta o jugar en el parque infantil.
La mayoría de los visitantes destaca la frescura y los largos trechos de sombra que conforman los árboles a lo
largo de todo el circuito de caminata.
Las personas que desean visitar el Parque de la Salud (Cabo 1° Marecos y Federación Rusa) deben llevar su
cédula de identidad o, en el caso de los extranjeros, su pasaporte para poder ingresar.
León indicó que uno de los inconvenientes que se presentan actualmente es que, aprovechando la seguridad
que existe en el lugar, algunos padres dejan a sus niños jugando durante todo el día sin la supervisión de una
persona responsable.
5
55% de los recursos de salud se concentran en Asunción
Última Hora, Paraguay
27
16/01/2009
Paraguay tiene un déficit de 5,7 profesionales de blanco. Las zonas más olvidadas del país son Alto Paraná e
Itapúa. Los servicios sanitarios del interior del país tienen graves problemas estructurales.
A pesar de que en Asunción y Central se concentra solo el 36% de la población del país, la Capital cuenta con
el 55% del personal de blanco del que dispone el Ministerio de Salud Pública.
Estas cifras no hacen más que desnudar una realidad de carencias. Prácticamente, todos los departamentos del
país, exceptuando Ñeembucú, tienen un déficit en relación al indicador de cantidad de profesionales de salud
(médicos, bioquímicos, odontólogos, licenciados y auxiliares en enfermería y obstetricia, etc.), que debería
haber por cada 10.000 habitantes, según las recomendaciones de la Organización Mundial de la Salud (OMS).
En general, Paraguay tiene un déficit de 5,7 profesionales de blanco por cada 10.000 personas, según un
análisis de la disponibilidad, el acceso y la exclusión social en Salud Pública, realizada por el doctor Diego
Gamarra, director de Servicios de Salud Pública.
Pero, como sucede en varios aspectos de la sociedad en el país, esa cifra sufre importantes altibajos,
dependiendo de la zona del territorio de la que se esté hablando.
Mientras Asunción, por ejemplo, supera la media de 25 profesionales de blanco por 10.000 habitantes,
llegando a un total de 62 (37 de más), a otros como Alto Paraná e Itapúa les falta 16 profesionales para poder
alcanzar la deseada cifra.
MEJORAS. El problema es conocido. Los profesionales de blanco no quieren ir al interior, ya sea por la falta de
infraestructura de los establecimientos de salud, o de las ciudades en sí.
"Para mejorar la distribución de los recursos humanos vamos a trabajar desde dos aristas. Una es la mejora de
la infraestructura de los establecimientos de salud. Hay que mejorar el clima laboral para que la gente esté
estimulada. La otra arista es la redistribución en sí de los recursos humanos, para lo que tenemos que trabajar
en contra del sistema laboral fraccionado, de profesionales que trabajan simultáneamente en la seguridad
social y en los ámbitos público y privado, percibiendo salarios bajos", expresó Gamarra.
Él afirma que los servicios sanitarios del interior tienen demasiados problemas estructurales, y que es
necesario además mejorar la dotación de equipamientos médicos con los que cuentan las instituciones.
Para el Ministerio de Salud, lo más importante es reorganizar las cuatro especialidades calificadas como las
más importantes: pediatría, gineco-obstetricia, cirugía y clínica médica, de modo a que en todo el territorio del
país se cuente uniformemente con estos especialistas.
Otra especialidad importante es la de anestesiología, quienes difieren de los anestesistas, en que los primeros
son profesionales médicos, y los segundos técnicos.
En este sentido, un punto muy importante es la formación de los médicos que se gradúan de las universidades.
En los hospitales especializados, y en algunos regionales del país se cuenta con residencias en las cinco
especialidades previamente mencionadas.
Según explica Gamarra, sin embargo, en lo que se debe hacer hincapié es en la formación de los médicos
generales, conocidos también como médicos de familia, teniendo en cuenta el nuevo enfoque que apunta a una
atención primaria.
APOYO LEGISLATIVO
El Ministerio de Salud apoya institucionalmente el desarrollo de la carrera sanitaria. Actualmente, se está
trabajando en un anteproyecto de ley a través del cual se buscará vincular a cada profesional de la salud a un
solo lugar de trabajo, de modo que realice en este sus 8 horas laborales diarias, teniendo allí todos los
beneficios laborales. Esto beneficiaría tanto a las dependencias de Salud como al Instituto de Previsión Social
(IPS).
El doctor Diego Gamarra agrega un comentario positivo. "Dentro de la ley de presupuesto actual ya se
contempla la posibilidad de que los profesionales concentren sus cargas horarias en una sola institución. Esto
quiere decir que un pediatra que hace una guardia en un hospital, consultorio en otro y atención de pacientes
internados en otro, podrá concentrar esos tres cargos en un solo lugar", apuntó.
6
Quedaron sin contrato más de 25 enfermeras
EntornoInteligente, Venezuela
20/01/2009
El Gobierno de Carabobo luego de ordenar el cese de contrato a 13 profesionales de la salud en días pasados,
anunció mediante uno de sus voceros que no podrá mantener en contratación a 15 enfermeras más de Insalud
en Puerto Cabello por supuesta falta de presupuesto, así lo denunció Nelson Díaz, dirigente comunal del sector
Santa Cruz.
28
"Es la excusa más descarada y abrumadora por parte del Ejecutivo regional, que pretende tomar venganza con
el estomago del porteño y más aún jugar con la salud del pueblo, porque esos puestos están vacíos creando
así déficit de enfermeras y por ende de atención para los pacientes", continuó el ex candidato a la concejalía.
De igual forma asegura que ya el mandatario regional tiene la nueva nómina preparada como parte de los
compromisos que adquirió en su campaña electoral, lo que le parece injusto con el personal que venía
ejerciendo sus labores en los distintos centro de salud del municipio.
Nelson Díaz realizó un llamado al presidente de la República, Hugo Chávez, para que tome medidas en el
asunto y además recuerde el caso del Instituto Puerto Autónomo, ya que el mismo no se encuentra a cargo de
personas de la entidad porteña.
Back to top
News from WHO and partners
1
Restoring Reproductive Health Services and Addressing Post-Traumatic Stress in Gaza
UNFPA
20/01/2009
United Nations — In a visit to the Gaza Strip today, UN Secretary-General Ban Ki-moon voiced shock and anger
at the ‘heartbreaking’ devastation, according to Reuters. Israeli attacks reportedly killed 1,300 and made
thousands homeless before the ceasefire took affect on 17 January.
As UNFPA Executive Director Thoraya A. Obaid told her Executive Board today, these reports do not include
deaths and delivery-related injuries of pregnant women who had no services to fully support them during the
conflict. “These are silent deaths and injuries that are forgotten because they are invisible to our eyes,” she
told the board. Some 3,700 women went into labour during the 22 days of conflict, she said.
In this early recovery phase, UNFPA, as part of a coordinated interagency effort, will be working on two main
fronts: restoring reproductive health care, including maternal and neonatal services, and providing
psychosocial support to traumatized survivors. UNFPA plans are contingent on being able to move
humanitarian supplies and building materials as well as technical experts into Gaza. For the time being, the
movement of people and goods, is severely restricted.
Restoring reproductive health services
In the early recovery phase, UNFPA will focus on rehabilitating and restoring reproductive health infrastructure
and services, including emergency obstetric and newborn care units. This includes reconstructing and
refurbishing key primary care clinics and five hospitals that were damaged in the incursion. The Fund’s
assistance will be tailored to needs identified in a broad-based assessment carried out by the UN early recovery
cluster.
UNFPA support will be provided for infrastructure repair, medical equipment and reproductive health supplies to
maternity units. Reproductive health care will be linked to psychosocial support and care for dealing with posttraumatic stress.
Providing psychosocial support
The entire population of Gaza, including health professionals, is at risk of post-traumatic stress in varying
degrees, according to UNFPA reports from the field. Since the ceasefire, the scale of the devastation and the
need for humanitarian aid have become ever more apparent, according to the International Committee of the
Red Cross. Entire families have lost everything and feel as if they are “waking up from a nightmare,” according
to the ICRC.
UNFPA’s partners already have teams of trained professionals in psychosocial counselling, outreach and referral
in Jabalia, Beit Lahia, Bureij, Khan Younis and Rafah. Additionally, UNFPA will deploy social workers to work
with affected families with special focus on women and young people. An already- existing network of 60
volunteer peer educators will provide community-based support in the five locations. An assessment outlining
the types of stress facing different sectors of the population and mapping out existing coping mechanisms has
been initiated by a UN interagency team.
Hygiene kits (a package of basic hygiene and household materials such as blankets, soap and towels) will be
distributed to displaced families to support their well-being and preserve their dignity. Target beneficiaries also
include households headed by women and those that are sheltering extended family and friends but without
additional resources to cope.
Many health professionals also will require help to overcome their own trauma and to recognize post-traumatic
stress syndrome in women. UNFPA, in partnership with an international NGO, will organize debriefing sessions
with counsellors and social workers, as well as with health professionals who served in hospitals and other
facilities during the incursion.
2
International Council of Nurses Announces New Nursing Education Network
International Council of Nurses
29
07/01/2009
Geneva, Switzerland, 07 January 2009 – A new International Council of Nurses (ICN) Network has been
established to promote excellence in nursing education to prepare a diverse 21st century nursing workforce.
New realities of international migration, easier movement across and between countries, advanced
communication technology, global health care, and a worldwide nursing shortage make the preparation of a
diverse nursing workforce a critical priority. ICN has responded positively to strong interest from several of its
member national nurses associations (NNAs), coordinated by the National League for Nursing (NLN)*, to
establish the ICN Nursing Education Network. The new network will provide a forum to address nursing
educational issues worldwide.
“The ICN Education Network is a significant step forward in addressing nursing education and strengthening its
contribution to the global health agenda,” stated ICN President Hiroko Minami. “We need the voice of
educators as we deal with the challenges of regulation and practice.”
“ICN advocates for nursing education to ensure that graduates enter clinical practice equipped to successfully
manage the conditions of health care delivery they encounter. We are pleased to stimulate an interest and
marshal commitment to the establishment of this network. We look forward to working and supporting ICN
towards a successful launch in Durban in 2009,” asserted NLN CEO Beverly Malone.
The network’s inaugural meeting will be held during the 24th ICN Quadrennial Congress, 27 June- 4 July 2009,
in Durban, South Africa. Several countries have already signaled interest in collaborating on the development
of an agenda, and the NLN has offered to work with ICN, its member NNAs and interested individuals and
educational organizations in moving forward. Among the primary items for exploration will be the international
shortages in the nursing workforce and in nursing faculty that exist in many countries.
*Dedicated to excellence in nursing, the National League for Nursing is the premier organization for nurse
faculty and leaders in nursing education, offering faculty development, networking opportunities, testing and
assessment, nursing research grants, and public policy initiatives to its 27,000 individual and 1,200
institutional members.
ICN Contact:
NLN Contact:
Linda Carrier-Walker; carrwalk@icn.ch ; +41 22 908 0100
Karen R. Klestzick; kklestzick@nln.org; +1 212 812 0376
3
International Council of Nurses Gaza statement
International Council of Nurses
20/01/2009
Geneva, Switzerland, 20 January 2009 – ICN is greatly concerned about the serious degradation of health
services and health supplies in Gaza amid the ongoing military action and the resulting impact on civilians,
including unacceptably high mortality rates, injuries resulting in devastating disability and long term physical
and psychological morbidity, outbreaks of communicable diseases and increasing maternal and new born
fatality.
ICN is calling for:
Immediate enforcement of International Humanitarian Law requiring all health personnel and facilities be
protected at all times, even during armed conflict. Attacks on them are grave violations of International
Humanitarian and Human Rights laws.
Immediate increased access to Gaza, overland and through ports, for the importation of essential medicines
and health care supplies and facilitation for the distribution of these supplies.
Increased periods of cease fire to allow for movement of patients, emergency services health personal,
medical supplies and delivery of health services.
Replacement health personnel, including trauma care teams, to sustain the provision of life-saving services
and relieve exhausted health personnel now working up to 24 hours a day.
Evacuation outside of Gaza of the critically injured and those suffering chronic condition that require extended
care (e.g. cancer, cardiac, neo-natal).
4
Doctors Call Zimbabwe’s Ruined Health System a “Man-Made Disaster”
Physicians for Human Rights
13/01/2009
In a new report released today, Physicians for Human Rights (PHR) finds that a causal chain runs from
Mugabe’s economic policies to Zimbabwe’s economic collapse, food insecurity and malnutrition and the current
outbreaks of infectious disease. The report is based on a health assessment by PHR public health and human
rights experts who travelled to Zimbabwe in December 2008.
The 45-page report, Health in Ruins: A Man-Made Disaster in Zimbabwe asserts that “the Government of
Zimbabwe has abrogated the most basic state functions in protecting the health of the population – including
the maintenance of public hospitals and clinics and the support for the health workers required to maintain the
public health system.” These services have been in decline since 2006, but the deterioration of both public
health and clinical care has dramatically accelerated since August 2008. PHR calls for emergency international
intervention to address the water, sanitation, food and health crisis.
30
PHR’s team, which included two public health physicians and two human rights advocates, documented the
closure of hospitals and clinics, breakdown in sanitation and water purification systems, the ensuing and
unchecked cholera epidemic, food scarcity, interruptions in HIV/AIDS treatment, untreated tuberculosis, and
new outbreaks of anthrax and diseases of malnutrition not seen in years in Zimbabwe. PHR asserts that the
2008 cholera epidemic continuing into 2009 is an outcome of the state’s failures in governance and in
protecting the basic rights of Zimbabweans.
“This disaster is man-made, was likely preventable, and has become a regional issue since the spread of
cholera to neighbour states,” stressed Dr. Chris Beyrer, one of the report’s authors and a professor at Johns
Hopkins School of Public Health. The report also documents that the Mugabe regime intentionally suppressed
initial reports of the cholera epidemic and has since denied or underplayed its gravity.
Dr. David Sanders, a team member and Professor of Public Health at the University of the Western Cape
stated, “The ZANU-PF government has exacerbated food insecurity for Zimbabweans in 2008 by blocking
international humanitarian organizations from delivering food aid and other succor to populations in the worstaffected rural areas.”
At the end of the PHR team’s visit to Zimbabwe, the state-controlled media falsely reported the delegation’s
arrest. “Not only does the government actively disregard the plight of its people, it also seeks to prevent the
horrific results of its actions being publicly disclosed. Our team was under constant surveillance,” noted PHR
researcher Richard Sollom.
The PHR report, which includes a preface by Justice Richard Goldstone, Mary Robinson and Archbishop
Desmond Tutu, accuses the Mugabe ZANU-PF regime of the systematic violation of a wide range of human
rights, including the rights to life, health, food, water and work. “When examined in the context of 28 years of
massive and egregious human rights violations against the people of Zimbabwe under the rule of Robert
Mugabe, they constitute added proof of the commission by the Mugabe regime of crimes against humanity,”
states the report. In the report PHR calls for the urgent resolution of the political impasse in Zimbabwe, an
emergency international health intervention equivalent to putting the health system into receivership, a UN
Security Council referral to the International Criminal Court to investigate crimes against humanity, and a
summit to address disruptions in HIV-AIDS and tuberculosis prevention and treatment.
The delegation to Zimbabwe consisted of:
Frank Donaghue, Chief Executive Officer of PHR.
David Sanders, MBChB, MRCP, DCH, DTPH, PHR Consultant, and Professor of Public Health, University of the
Western Cape, Cape Town, South Africa
Richard Sollom, MA, MPH, PHR researcher and lead author of the report.
Chris Beyrer, MD, MPH, PHR Consultant and Director, Johns Hopkins Center for Public Health and Human
Rights.
Read the related Press Release Health System Collapse Requires International Intervention, Concludes PHR
Report
Download PHR’s Health in Ruins: A Man-Made Disaster in Zimbabwe (PDF): Full report - Summary
PHR released a short online video entitled La Fleuve du Mal which is available on YouTube.
PHR’s photographs are also available on Flickr.
31