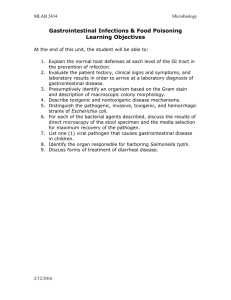
Non-occlusive mesenteric ischemia: a new gastrointestinal
advertisement

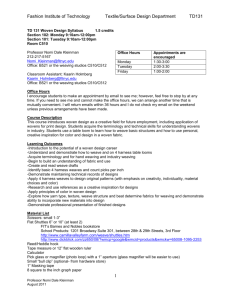
Clinical effect of vasodilating agents in patients diagnosed with non-occlusive mesenteric ischemia A. Sana MD1, L.M.G. Moons MD PhD1, P.B.F. Mensink MD PhD1, E.V. Rouwet MD PhD3, D. Van Noord MD1, T.C. Leertouwer MD PhD2, H.J.M. Verhagen MD PhD3, Ernst J. Kuipers MD PhD1,4 Departments of Gastroenterology and Hepatology1, Intervention Radiology2, Vascular Surgery3, Internal Medicine4, Erasmus MC - University Medical Center, Rotterdam, The Netherlands Chronic non-occlusive mesenteric ischemia (NOMI) is referred to as presence of confirmed mucosal ischemia in patients with open gastrointestinal arteries. NOMI is thought to develop secondary to a low flow state or vasospasm, and to be part of the clinical spectrum of chronic gastrointestinal ischemia (CGI). It has been suggested that vasodilating medication can be effective. The aim of this study was to evaluate the therapeutic effect of vasodilating medication in NOMI patients. Patients referred for evaluation of CGI were prospectively included. All patients had a standard work-up, consisting of evaluation of symptoms, angiography for evaluation of gastrointestinal arterial patency and functional assessment of mucosal perfusion by tonometry or visible light spectroscopy. Patients were diagnosed with NOMI if the symptoms suggested CGI, and functional testing revealed mucosal ischemia, in the absence of gastrointestinal artery stenosis. NOMI was treated with escalating doses of isosorbide dinitrate (ISD; 20 or 40 mg), followed by ketanserin (KTS; 20 or 40 mg) if ISD was not successful or tolerated. A positive treatment response was defined as loss of pain. In 3.5 years, 353 pts were referred for evaluation of suspected CGI. NOMI was diagnosed in 59 (17%) pts; 37 (63%) females, mean age 56 (17-82) yrs. The characteristics were: postprandial pain 46 (78%), weight loss 40 (68%), nausea 23 (39%), diarrhea 13 (22%), the history of cardiac and vascular disease 23 (39%) and diabetes 12 (20%). Vasodilation therapy was initiated in 42 (71%) patients. Of the remaining 17 patients, 11 had conservative treatment with proton pomp inhibition, 5 patients were diagnosed with cardiac dysfunction and were treated accordingly, and one patient with severe COPD had intensification of pulmonary treatment. Sustained response was achieved in 11/42 (26%) pts treated with ISD (mean follow-up 21 months). Of 31 non-responders to ISD, 22 (71%) were treated with KTS. Six (27%) of them had a sustained response (mean follow-up 8 months). Intention to treat and per protocol analysis showed an overall therapy response of 41% and 55%, respectively. There was no difference in baseline characteristics between responders and non-responders. Responders had a median weight gain of 1 (IQR: -1 – + 6) kg, whereas the non-responders had median weight loss of – 0.6 (IQR: -4 – + 1) kg. Side effects were reported in 18/42 patients (43%), in particular headache, and dizziness. Vasodilating medication is of benefit to approximately half of patients with chronic NOMI. Further studies are needed to optimize the effectiveness of vasodilating agents in these patients, and predict therapeutic response.