the_central_nervous_..
advertisement

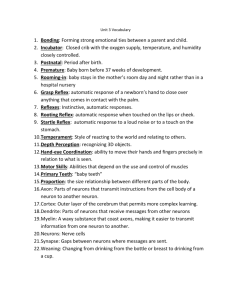
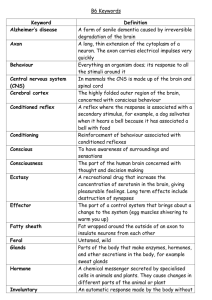
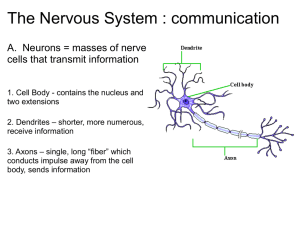
1 THE CENTRAL NERVOUS SYSTEM 1. Introduction The human nervous system has two main divisions: the Central nervous system (CNS), and the Peripheral nervous system (PNS), which includes the somatic Motor nervous system, and the Sensory nervous system. The CNS consists of the brain and spinal cord. It acts as the central control region of the human nervous system, processing information and issuing commands. The Autonomic Nervous System (ANS) is the command network the CNS uses to maintain the body's homeostasis. It automatically regulates heartbeat and controls muscle contractions in the walls of blood vessels, digestive, urinary, and reproductive tracts. It also carries messages that help stimulate glands to secrete tears, mucus, and digestive enzymes… The part of the autonomic nervous system originating in the thoracic and lumbar regions of the spinal cord that in general inhibits or opposes the physiological effects of the parasympathetic nervous system, as in tending to reduce digestive secretions, speeding up the heart, and contracting blood vessels. Neurons are cells that are specialized to receive, propagate and transmit electrochemical impulses. In the human brain alone, there are over a hundred billion neurons. Neurons are diverse with respect to morphology and function. CNS – Belgium - HHRoeselare – A. Houtman 17/02/2016 – Version 1 2 2. Overview of the Central Nervous system Structural Divisions of the nervous system: 1. Central Nervous System (CNS) - the brain and spinal cord. 2. Peripheral Nervous System (PNS) - the nerves, ganglia, receptors, etc. Functions of the nervous system: 1. Control of effectors, both voluntary and autonomic muscles (skeletal, smooth, cardiac), glands 2. Response to stimuli 3. Integration of processes 4. Responsible for conscious thought and perception, emotions, personality, the mind. Functional Divisions of the Nervous System: 1. The Voluntary Nervous System - (somatic division) control of wilful control of effectors (skeletal muscles) and conscious perception. Mediates voluntary reflexes. 2. The Autonomic Nervous System - control of autonomic effectors smooth muscles, cardiac muscle, glands; responsible for "visceral" reflexes. Types of neurons based on function: 1. Motor neurons - these carry a message to a muscle, gland or other effector. They are said to be efferent, i.e. they carry the message away from the central nervous system. 2. Sensory neurons - these carry a message in to the CNS; they are afferent, i.e. going toward the brain or spinal cord. 3. Interneuron (association neuron, connecting neuron); these neurons connect one neuron with another; e.g. in many reflexes interneurons connect the sensory neurons with the motor neurons. CNS – Belgium - HHRoeselare – A. Houtman 17/02/2016 – Version 1 3 3. Neuron A. Introduction A neuron is a particular kind of cell that is specialized for the storage and transmission of information. Neurons are found in the brain as well as in the brainstem and spinal cord; they are also the nerve cells which transmit information to muscles and which register sensory information (e.g. touch stimuli). There are between 10 billion and 100 billion neurons in the brain; each neuron may contact about 1000 others. Most neurons have three recognizable components: a cell body, an axon and dendrites. The cell body contains the machinery needed to convert nutrients to energy and keep the cell alive. The dendrites are input areas that contain receptors; each receptor is specialized to respond to a particular kind of neurotransmitter. If enough receptors are activated, the neuron may become active itself. In this case, an electrical charge is generated and passes down the axon, the output process of the neuron. The axon can vary from a few millimetres to several cm’s (inches) in length, and can branch widely. When the electrical charge reaches the tip of the axon, neurotransmitters are released. These neurotransmitters may in turn activate receptors on the dendrites of neighbouring neurons, passing the message along. Neurons come in many sizes: e.g. a single sensory neuron from the fingertip has an axon that extends the length of the arm, while neurons within the brain may extend only a few millimetres. Neurons have different shapes depending on what they do. Motor neurons that control muscle contractions have a cell body on one end, a long axon in the middle and dendrites on the other end; sensory neurons have dendrites on both ends, connected by a long axon with a cell body in the middle. Neurons generate electrical impulses or changes in voltage of two types: graded potentials and action potentials. Graded potentials occur when the membrane potential depolarizes and hypolarizes in a graded fashion relative to the amount of stimulus that is applied to the neuron. An action potential on the other hand is an all-or-none electrical impulse. Despite being slower than graded potentials, action potentials have the advantage of traveling long distances in axons with little or no decrement. CNS – Belgium - HHRoeselare – A. Houtman 17/02/2016 – Version 1 4 B. Anatomy of the Nerve a. Neurons have three basic parts: Cell body: This main part has all of the necessary components of the cell, such as the nucleus (contains DNA), endoplasmic reticulum and ribosomes (for building proteins) and mitochondria (for making energy). Axon: This long, cable-like projection of the cell carries the electrochemical message (nerve impulse or action potential) along the length of the cell. (Depending upon the type of neuron, axons can be covered with a thin layer of myelin, like an insulated electrical wire. Myelin is made of fat, and it helps to speed transmission of a nerve impulse down a long axon. Myelinated neurons are typically found in the peripheral nerves (sensory and motor neurons), while non-myelinated neurons are found in the brain and spinal cord. ) Dendrites or nerve endings: These small, branch-like projections of the cell make connections to other cells and allow the neuron to communicate with other cells or perceive the environment. Dendrites can be located on one or both ends of the cell. CNS – Belgium - HHRoeselare – A. Houtman 17/02/2016 – Version 1 5 b. Neurons also vary with respect to their functions: Sensory neurons carry signals from the outer parts of your body (periphery) into the central nervous system. Motor neurons carry signals from the central nervous system to the outer parts (muscles, skin and glands) of your body. Receptors sense the environment (chemicals, light, sound, touch) and encode this information into electrochemical messages that are transmitted by sensory neurons. Interneurons connect various neurons within the brain and spinal cord. Interneuron CNS – Belgium - HHRoeselare – A. Houtman 17/02/2016 – Version 1 6 CNS – Belgium - HHRoeselare – A. Houtman 17/02/2016 – Version 1 7 c. Structure of a nerve: A peripheral nerve is arranged much like a muscle in terms of its connective tissue. It has an outer covering which forms a sheath around the nerve, called the epineurium. Often a nerve will run together with an artery and vein and their connective coverings will merge. Nerve fibers, which are axons, organize into bundles known as fascicles with each fascicle surrounded by the perineurium. Between individual nerve fibers is an inner layer of endoneurium. The myelin sheath in peripheral nerves consists of Schwann cells wrapped in many layers around the axon fibers. Not all fibers in a nerve will be myelinated, but most of the voluntary fibers are. The Schwann cells are portrayed as arranged along the axon like sausages on a string. (A more apt analogy would be like jelly rolls!) Gaps between the Schwann cells are called nodes of Ranvier. These nodes permit an impulse to travel faster because it doesn't need to depolarize each area of a membrane, just the nodes. This type of conduction is called saltatory conduction and means that impulses will travel faster in myelinated fibers than in unmyelinated ones. d. The myelin-sheath does several things: 1. It provides insulation to help prevent short circuiting between fibers. Diseases which destroy the myelin sheath lead to inability to control muscles, perceive stimuli etc. (One such disease is multiple sclerosis, an autoimmune disorder in which your own lymphocytes attack the myelin proteins.) 2. The myelin sheath provides for faster conduction. 3. The myelin sheath provides for the possibility of repair of peripheral nerve fibers. Schwann cells help to maintain the micro-environments of the axons and their tunnel (the neurilemma tunnel) permits re-connection with an effector or receptor. CNS – Belgium - HHRoeselare – A. Houtman 17/02/2016 – Version 1 8 C. Neuron Function and Potential - Neurons communicate with one another via synapses. Synapses are specialized junctions between two cells in close apposition to one another. In a synapse, the neuron that sends the signal is the presynaptic neuron and the target cell receives that signal is the postsynaptic neuron or cell. Synapses can be either electrical or chemical. Electrical synapses are characterized by the formation of gap junctions that allow ions and other organic compound to instantaneously pass from one cell to another. - An action potential in the squid giant axon has been the basis for much of the current understanding of the ionic bases of action potentials. Briefly, the model states that the generation of an action potential is determined by two ions: Na+ and K+. An action potential can be divided into several sequential phases: threshold, rising phase, falling phase, undershoot phase, and recovery. Following several local graded depolarizations of the membrane potential, the threshold of excitation is reached, voltage-gated sodium channels are activated, which leads to an influx of Na+ ions. - As Na+ ions enter the cell, the membrane potential is further depolarized, and more voltage-gated sodium channels are activated. Such a process is also known as a positive-feedback loop. CNS – Belgium - HHRoeselare – A. Houtman 17/02/2016 – Version 1 9 - As the rising phase reaches its peak, voltage-gated Na+ channels are inactivated whereas voltage-gated K+ channels are activated, resulting in a net outward movement of K+ ions, which repolarizes the membrane potential towards the resting membrane potential. Repolarization of the membrane potential continues, resulting in an undershoot phase or absolute refractory period. The undershoot phase occurs because unlike voltage-gated sodium channels, voltage-gated potassium channels inactivate much more slowly. Nevertheless, as more voltage-gated K+ channels become inactivated, the membrane potential recovers to its normal resting steady state - When an impulse reaches the end of an axon, it triggers the formation of synaptic vesicles at that terminal. Synaptic vesicles are specialized vacuoles that contain neurotransmitters (such as acetylcholine). - The vesicles transport the neurotransmitters to the end of the axon and release them into the synaptic cleft. These neurotransmitters attach to receptor sites on the cell membrane of the receiving neuron. When enough receptor sites are filled, the firing threshold of the receiving neuron is reached and a depolarization event is triggered. Transport of Neurotransmitters, movement of K+ ion and Na+ ion - Before the neuron depolarizes, it is held steady in its resting potential. This potential, which is achieved by maintaining a relatively high concentration of sodium ions outside of the cell membrane, represents an approximately -70 millivolt discrepancy between the negatively charged interior and positively charged exterior. CNS – Belgium - HHRoeselare – A. Houtman 17/02/2016 – Version 1 10 - As neurotransmitters attach to the receptor sites and overcome the firing threshold, small molecular gates open along the cell membrane allowing the sodium ions to rapidly flood the neuron. This sudden change in polarity from the influx of positive ions triggers an action potential that moves like a wave down the axon triggering another nerve, muscle cell, etc. - At this point, a different series of molecular gates open which allows potassium ions to rush out of the neuron. The potassium ions, which have a positive charge as well, create a negatively charged cell interior by their absence. This event stops the depolarization process. The sodium ions are pumped more slowly to the cell exterior by active transport, resulting in the fully restored resting potential once again. - Neurons communicate with one another via synapses. Synapses are specialized junctions between two cells in close apposition to one another. In a synapse, the neuron that sends the signal is the presynaptic neuron and the target cell receives that signal is the postsynaptic neuron or cell. Synapses can be either electrical or chemical. Electrical synapses are characterized by the formation of gap junctions that allow ions and other organic compound to instantaneously pass from one cell to another. Chemical synapses are characterized by the pre-synaptic release of neurotransmitters that diffuse across a synaptic cleft to bind with postsynaptic receptors. - A neurotransmitter is a chemical messenger that is synthesized within neurons themselves and released by these same neurons to communicate with their postsynaptic target cells. A receptor is a transmembrane protein molecule that a neurotransmitter or drug binds. Chemical synapses are slower than electrical synapses. CNS – Belgium - HHRoeselare – A. Houtman 17/02/2016 – Version 1 11 CNS – Belgium - HHRoeselare – A. Houtman 17/02/2016 – Version 1 12 4. The spinal Cord A. Anatomy - The spinal cord is the connection centre for the reflexes as well as the afferent (sensory) and efferent (motor) pathways for most of the body below the head and neck. The spinal cord begins at the brainstem and ends at about the second lumbar vertebra. The sensory, motor, and interneurons discussed previously are found in specific parts of the spinal cord and nearby structures. - Sensory neurons have their cell bodies in the spinal (dorsal root) ganglion. Their axons travel through the dorsal root into the grey matter of the cord. Within the grey matter are interneurons with which the sensory neurons may connect. Also located in the grey matter are the motor neurons whose axons travel out of the cord through the ventral root. CNS – Belgium - HHRoeselare – A. Houtman 17/02/2016 – Version 1 13 CNS – Belgium - HHRoeselare – A. Houtman 17/02/2016 – Version 1 14 - The white matter surrounds the grey matter. It contains the spinal tracts which ascend and descend the spinal cord. Surrounding both the spinal cord and the brain are the meninges, a three layered covering of connective tissue. - The dura mater is the tough outer layer. - Beneath the dura is the arachnoid which is like a spider web in consistency. The arachnoid has abundant space within and beneath it (the subarachnoid space) which contains cerebrospinal fluid, as does the space beneath the dura mater (subdural space). This cerebrospinal fluid supplies buoyancy for the spinal cord and brain to help provide shock absorption. - The pia mater is a very thin layer which adheres tightly to the surface of the brain and spinal cord. It follows all contours and fissures (sulci) of the brain and cord. - At 31 places along the spinal cord the dorsal and ventral roots come together to form spinal nerves. Spinal nerves contain both sensory and motor fibers, as do most nerves. Spinal nerves are given numbers which indicate the portion of the vertebral column in which they arise. There are 8 cervical (C1-C8), 12 thoracics (T1-T12), 5 lumbar (L1-L5), 5 sacral (S1-S5), and 1 coccygeal nerve. Nerve C1 arises between the cranium and atlas (1st cervical vertebra) and C8 arises between the 7th cervical and 1st thoracic vertebra. - All the others arise below the respective vertebra or former vertebra in the case of the sacrum. Since the actual cord ends at the second lumbar vertebra, the later roots arise close together on the cord and travel downward to exit at the appropriate point. These nerve roots are called the cauda equina because of their resemblance to a horse’s tail. CNS – Belgium - HHRoeselare – A. Houtman 17/02/2016 – Version 1 15 CNS – Belgium - HHRoeselare – A. Houtman 17/02/2016 – Version 1 16 B. Plexus Spinal nerves join together in plexuses. A plexus is an interconnection of fibers which form new combinations as the "named" or peripheral nerves. There are four voluntary plexuses (there are some autonomic plexuses which will be mentioned later): they are the cervical plexus, the brachial plexus, the lumbar plexus, and the sacral plexus. Each plexus gives rise to new combinations of fibers as the peripheral nerves. The nerves and plexuses you need to know are: 1. Cervical Plexus: The phrenic nerve travels through the thorax to innervate the diaphragm. 2. Brachial Plexus Axillary nerve - innervates the deltoid muscle and shoulder, along with the posterior aspect of the upper arm. Musculocutaneous nerve - innervates anterior skin of upper arm and elbow flexors. Radial nerve - innervates dorsal aspect of the arm and extensors of the elbow, wrist, and fingers, abduction of thumb. Median nerve - innervates the middle elbow, wrist and finger flexors, adducts the thumb. Ulnar nerve - innervates the medial aspect wrist and finger flexors. 3. Lumbar Plexus genitofemoral - to the external genitalia obturator - to the adductor muscles femoral - innervates the skin and muscles of upper thigh, including the quadriceps. 4. Sacral Plexus gluteal nerves (superior and inferior) - superior innervates the gluteus medius and minimus, inferior innervates the gluteus maximus. Sciatic nerve - the body's largest nerve, consisting of two major branches, the tibial and common peroneal. Together they innervate most all of leg including the flexors of the knee, part of adductor magnus, muscles for plantar flexion, dorsiflexion, and other movements of the foot and toes. CNS – Belgium - HHRoeselare – A. Houtman 17/02/2016 – Version 1 17 Cervical Plexus Sacral plexus Brachial Plexus Lumbar Plexus CNS – Belgium - HHRoeselare – A. Houtman 17/02/2016 – Version 1 18 C. The Reflex A reflex is a direct connection between stimulus and response, which does not require conscious thought. There are voluntary and involuntary reflexes. It is the voluntary reflexes we are considering here. As discussed earlier, a reflex involves at least 2 or 3 neurons. The typical components of a reflex are shown in. The 3-neuron reflex requires three types of neurons: a sensory, an interneuron, and a motor neuron. It is also called a withdrawal reflex because it is commonly involved in withdrawing from painful stimuli. Withdrawing from painful stimuli does not require thought. But the interneuron does send a fiber through the spinothalamic tract to the brain where the pain is perceived. 1. The Stretch Reflex: The stretch reflex in its simplest form involves only 2 neurons, and is therefore sometimes called a 2-neuron reflex. The two neurons are a sensory and a motor neuron. The sensory neuron is stimulated by stretch (extension) of a muscle. Stretch of a muscle normally happens when its antagonist contracts, or artificially when its tendon is stretched, as in the knee jerk reflex 2. The Deep Tendon Reflex: Tendon receptors respond to the contraction of a muscle. Their function, like that of stretch reflexes, is the coordination of muscles and body movements. The deep tendon reflex involves sensory neurons, interneurons and motor neurons. The response reverses the original stimulus therefore causing relaxation of the muscle stimulated (in order to facilitate that the reflex sends excitatory stimuli to the antagonists causing them to contract - reciprocal activation). 3. The Crossed Extensor Reflex The crossed extensor reflex is just a withdrawal reflex on one side with the addition of inhibitory pathways needed to maintain balance and coordination. A reflex action or reflex is a biological control system linking stimulus to response and mediated by a reflex arc. Reflexes can be built-in or learned. For example, a person stepping on a sharp object would initiate the reflex action through the creation of a stimulus, (pain) within specialized sense receptors located in the skin tissue of the foot. The resulting stimulus would be transmitted through afferent, or sensory neurons to the spinal cord. This stimulus is usually processed by an interneuron to create an immediate response to pain by initiating a motor (muscular) response which is acted upon by muscles of the leg, retracting the foot away from the object. This retraction would occur as the pain sensation is arriving in the brain which would process a more cognitive evaluation of the situation. CNS – Belgium - HHRoeselare – A. Houtman 17/02/2016 – Version 1 19 D. Human reflexes Reflex actions seen in adult humans include: 1. The Accommodation reflex is a reflex action of the eye, in response to focusing on a near object, then looking at distant object (and vice versa), comprising coordinated changes in vergence, lens shape and pupil size. It is dependent on cranial nerve II (afferent limb of reflex), higher centres and cranial nerve III) 2. The Achilles reflex (the ankle jerk reflex) occurs when the Achilles tendon is tapped while the foot is dorsi-flexed. A positive result would be the jerking of the foot towards its plantar surface. The Achilles reflex checks if the S1 and S2 nerve roots are intact and could be indicative of sciatic nerve pathology. It is classically delayed in hypothyroidism. This reflex is usually absent in disk herniations at the L5-S1 level. CNS – Belgium - HHRoeselare – A. Houtman 17/02/2016 – Version 1 20 3. The Anocutaneous reflex (the anal wink) is the reflexive contraction of the external anal sphincter upon stroking of the skin around the anus. The absence of this reflex indicates that there is an interruption of the reflex arc, which may be in the sensory afferent limb or the motor efferent limb. The synapse between the afferent and efferent limbs occurs in the lowest sacral segments of the spinal cord. 4. The Biceps stretch reflex examines the function of the C5 reflex arc and to a lesser degree the C6 reflex arc. The test is performed by using of a tendon hammer to quickly depress the biceps brachii tendon as it passes through the cubital fossa. Specifically, the test activates the stretch receptors inside the biceps brachii muscle which communicates mainly with the C5 spinal nerve and partially with the C6 spinal nerve to induce a reflex outcome. The reflex results in flexion of the antebrachium. 5. The Brachioradialis reflex (supinator reflex) is testing the reflex motor arc associated with the brachioradialis muscle. The supinator reflex is tested by striking the lower end of the radius just above the wrist with a tendon hammer. This normally causes contraction of the brachioradialis and hence flexion of the elbow. 6. The Corneal reflex (the blink reflex): is an automated involuntary blinking of the eyelids elicited by stimulation (such as touching or a foreign body) of the eyeball's cornea. The evolutionary purpose of this reflex is to protect the eyes from foreign bodies.The reflex is mediated by: the nasociliary branch of the ophthalmic nerve (V1) of the 5th Cranial nerve (Trigeminal) sensing the stimulus on the cornea, and the 7th Cranial nerve (Facial nerve) initiating the motor response. The examination of the corneal reflex is a part of some neurological tests in particular the coma exam. 7. The Crossed extensor reflex: When the reflex occurs the flexors in the withdrawing limb contract and the extensors relax, while in the other limb the opposite occurs 8. The H-reflex is a reflectory reaction of muscles after electrical stimulation of sensory fibers in their innervating nerves (for example, those located behind the knee). CNS – Belgium - HHRoeselare – A. Houtman 17/02/2016 – Version 1 21 9. The patellar reflex or knee jerk is a monosynaptic reflex. Striking the patellar tendon with a tendon hammer just below the patella stretches the quadriceps tendon. This stimulates stretch sensory receptors (most importantly, muscle spindles) that trigger an afferent impulse in a sensory nerve fiber of the femoral nerve leading to the lumbar region of the spinal cord. There, the sensory neuron synapses directly with a motor neuron that conducts an efferent impulse to the quadriceps femoris muscle, triggering contraction. This contraction, coordinated with the relaxation of the antagonistic flexor hamstring muscle causes the leg to kick. It has been thought that this type of reflex helps maintain the upright posture. The patellar tendon reflex tests the function of the femoral nerve and spinal cord segements L2-L4. The Patellar reflex CNS – Belgium - HHRoeselare – A. Houtman 17/02/2016 – Version 1 22 10. The Babinski reflex or the Plantar reflex: The lateral side of the sole of the foot is rubbed with a blunt implement so as not to cause pain, discomfort or injury to the skin; the instrument is run from the heel along a curve to the metatarsal pads. There are three responses possible: Flexor: the toes curve inward and the foot everts; this is the response seen in healthy adults. Indifferent: there is no response. Extensor: the hallux (large toe) extends upward, and the other toes fan out; Babinski's sign. o o The extensor response can indicate damage of the spinal cord in the thoracal or lumbar region, or brain disease. Occasionally, a pathological plantar reflex is the first (and only) indication of a serious disease process, and a clearly abnormal plantar reflex often prompts detailed neurological investigations, including CT scanning of the brain or MRI of the spine, as well as lumbar puncture for the study of cerebrospinal fluid. Young babies (less than a few months of age) will also show an extensor response. A baby's smaller toes will fan out, and their big toe wills dorsiflex slowly. This happens because the corticospinal pathways (that run from the brain down the spinal cord) are not fully myelinated at this age, so the reflex is not inhibited by the cerebral cortex. 11. Pupillary reflex: The pattern of papillary response to light can help determine which of the cranial nerves is damaged. There are two types of response assessed for each eye: Direct pupillary reflex: whether each pupil constricts with light shone into the that eye Consensual pupillary reflex: whether each pupil constricts with light shone into the other eye CNS – Belgium - HHRoeselare – A. Houtman 17/02/2016 – Version 1 23 Test for nerve damage - Emergency room physicians often assess the pupillary reflex because it is useful for gauging brain stem function. Normally, pupils react (constrict) equally. Lack of the pupillary reflex or an abnormal pupillary reflex can be caused by optic nerve damage, oculomotor nerve damage, brain death and depressant drugs, such as barbiturates. The optic nerve is responsible for the afferent limb of the pupillary reflex, or in other words, senses the incoming light. The oculomotor nerve is responsible for the efferent limb of the pupillary reflex; in other words, it drives the muscles that constrict the pupil. - Normally, each pupil should constrict with light shone into either eye. On testing each reflex for each eye, several patterns are possible. 12. Scratch reflex is a reflex transmitted by very sensitive nerve endings near the surface of the skin via the spinal cord, and is a reflex frequently inherited by mammals. The nerve signal includes positioning to pinpoint the location of the itch, and the effect of the reflex is either an affective sensation or even an involuntary action to make a scratching movement that usually relieves the itch. The scratch reflex is a reflex to help an organism protect and rid its body of parasites and other irritants. CNS – Belgium - HHRoeselare – A. Houtman 17/02/2016 – Version 1 24 In case of intense itch, scratching to relieve it can cause pain, and such pain signals are believed to suppress the itch signals due to a lateral inhibition effect, as the dorsal column system transmits critical sensations much faster than the cruder spinothalamic tract that deals with less accurate types of sensations, such as itch, also at a slower pace. 13. The Tendon reflex (or T-reflex) is an feedback mechanism that controls increasing muscle tension by causing muscle relaxation before tension force becomes so great it may damage the muscle 14. The Vestibulo-Ocular Reflex (VOR) is a reflex eye movement that stabilizes images on the retina during head movement by producing an eye movement in the direction opposite to head movement, thus preserving the image on the center of the visual field. For example, when the head moves to the right, the eyes move to the left, and vice versa. 15. The Caloric reflex test is a test of the vestibulo-ocular reflex. It is used by physicians to assess brain stem function and may be part of an evaluation to determine brain death. It involves putting cold or hot water into the external auditory canal. If the water is cold (4o C) the eyes turn toward the ipsilateral ear, with horizontal nystagmus (quick horizontal eye movements) to the contra lateral ear. If the water is warm (44oC) the eyes turn toward the contra lateral ear, with horizontal nystagmus to the ipsilateral ear. Absent reactive eye movement suggests brain death. Cold water = nystagmus to the opposite side Warm water = nystagmus to the same side CNS – Belgium - HHRoeselare – A. Houtman 17/02/2016 – Version 1 25 CNS – Belgium - HHRoeselare – A. Houtman 17/02/2016 – Version 1 26 5. Parasympathetic - and Sympathetic Nervous System A. The Parasympathetic Nervous System and the Sympathetic Nervous System (SNS) as a part of the Autonomic Nervous System. Sympathetic Nervous System is the portion of the autonomic nervous system concerned with non-volitional preparation of the organism for emergency situations; it is frequently referred to as the "fight or flight" system, as it has a stimulatory effect on organs and physiological systems. In contrast the parasympathetic nervous system has been described as the "rest and digest" system because it has a relaxing effect on many organs. The Sympathetic Nervous System is controlled by bunches of nerves called ganglions. One large ganglion, called the stellate ganglion, helps control nerves in the upper body. In the lower body, nerves are controlled by several ganglions that make up the sympathetic chain. The Parasympathetic Nervous System is sometimes called the rest and digests system; the parasympathetic system conserves energy as it slows the heart rate, increases intestinal and gland activity, and relaxes sphincter muscles in the gastrointestinal tract. The Parasympathetic Nervous System is a portion of the visceral (autonomic) branch of the PNS (peripheral nervous system). The regions of the body associated with this division are the cranial and sacral regions of the spinal cord. Specifically, cranial nerves III, VII, IX, X (vagus n.) and in the sacral region (spinal nerves exiting from the sacrum) the spinal nerves S2 to S4. CNS – Belgium - HHRoeselare – A. Houtman 17/02/2016 – Version 1 27 1. Parasympathetic Nervous System Dilates blood vessels leading to the GI tract, increasing blood flow. This is important following the consumption of food, due to the greater metabolic demands placed on the body by the gut. The parasympathetic nervous system can also constrict the bronchiolar diameter when the need for oxygen has diminished. CNS – Belgium - HHRoeselare – A. Houtman 17/02/2016 – Version 1 28 During accommodation, the parasympathetic nervous system causes constriction of the pupil and lens. The parasympathetic nervous system stimulates salivary gland secretion, and accelerates peristalsis, so, in keeping with the rest and digests functions; appropriate PNS activity mediates digestion of food and indirectly, the absorption of nutrients. Is also involved in erection of genitals, via the pelvic splanchnic nerves 2-4. 2. Sympathetic Nervous System Diverts blood flow away from the gastro-intestinal (GI) tract and skin via vasoconstriction. Blood flow to skeletal muscles, the lung is not only maintained, but enhanced (by as much as 1200%, in the case of skeletal muscles). Dilates bronchioles of the lung, which allows for greater alveolar oxygen exchange. Increases heart rate and the contractility of cardiac cells (myocytes), thereby providing a mechanism for the enhanced blood flow to skeletal muscles. Dilates pupils and relaxes the lens, allowing more light to enter the eye. CNS – Belgium - HHRoeselare – A. Houtman 17/02/2016 – Version 1 29 6. NEUROTRANSMITTERS A. Definition Neurotransmitters are chemicals that allow the movement of information from one neuron across the gap between it and the adjacent neuron. The release of neurotransmitters from one area of a neuron and the recognition of the chemicals by a receptor site on the adjacent neuron causes an electrical reaction that facilitates the release of the neurotransmitter and its movement across the gap. The three major categories of substances that act as neurotransmitters: 1. Amino acids (primarily glutamic acid, GABA [= Gamma-aminobutyric acid], aspartic acid & glycine), 2. Peptides (vasopressin, somatostatin, neurotensin, etc.) and 3. Monoamines (norepinephrine, dopamine & serotonin) plus acetylcholine. The major "workhorse" neurotransmitters of the brain are glutamic acid (=glutamate) and GABA. The monoamines & acetylcholine perform specialized modulating functions, often confined to specific structures. The peptides perform specialized functions in the hypothalamus or act as cofactors elsewhere in the brain. CNS – Belgium - HHRoeselare – A. Houtman 17/02/2016 – Version 1 30 There are many neurotransmitters in the central nervous system, the peripheral nervous system has only two: acetylcholine and norepinephrine. Some examples of neurotransmitter action: Acetylcholine: Acetylcholine is particularly important in the stimulation of muscle tissue. After stimulation, acetylcholine degrades to acetate and choline, which are absorbed back into the first neuron to form another acetylcholine molecule. The poison curare blocks transmission of acetylcholine. Some nerve gases inhibit the breakdown of acetylcholine, producing a continuous stimulation of the receptor cells, and spasms of muscles such as the heart. Epinephrine (adrenaline) and norepinephrine: These compounds are secreted principally from the adrenal gland. Secretion causes an increased heart rate and the enhanced production of glucose as a ready energy source (the "fight or flight" response). Dopamine: Dopamine facilitates critical brain functions and, when unusual quantities are present, abnormal dopamine neurotransmission may play a role in Parkinson's disease, certain addictions, and schizophrenia. Serotonin: Synthesized from the amino acid tryptophan, serotonin is assumed to play a biochemical role in mood and mood disorders, including anxiety, depression, and bipolar disorder. Aspartate: An amino acid that stimulates neurons in the central nervous system, particularly those that transfer information to the area of the brain called the cerebrum. Oxytocin: A short protein (peptide) that is released within the brain, ovary, and testes. The compound stimulates the release of milk by mammary glands, contractions during birth, and maternal behavior. Somatostatin: A peptide, which is inhibitory to the secretion of growth hormone from the pituitary gland, of insulin, and of a variety of gastrointestinal hormones involved with nutrient absorption. Insulin: A peptide secreted by the pancreas that stimulates other cells to absorb glucose. The actions of some drugs mimic those of naturally occurring neurotransmitters. The pain-regulating endorphins, for example, are similar in structure to heroin and codeine, which fill endorphin receptors to accomplish their effects. The wakefulness that follows caffeine consumption is the result of its blocking the effects of adenosine, a neurotransmitter that inhibits brain activity. CNS – Belgium - HHRoeselare – A. Houtman 17/02/2016 – Version 1 31 Acetylcholine - voluntary movement of the muscles Norepinephrine - wakefulness or arousal Dopamine - voluntary movement and emotional arousal Serotonin - memory, emotions, wakefulness, sleep and temperature regulation GABA (gamma aminobutyric acid) - motor behaviour Glycine - spinal reflexes and motor behaviour Neuromodulators - sensory transmission-especially pain CNS – Belgium - HHRoeselare – A. Houtman 17/02/2016 – Version 1 32 CNS – Belgium - HHRoeselare – A. Houtman 17/02/2016 – Version 1 33 CNS – Belgium - HHRoeselare – A. Houtman 17/02/2016 – Version 1 34 CNS – Belgium - HHRoeselare – A. Houtman 17/02/2016 – Version 1 35 CNS – Belgium - HHRoeselare – A. Houtman 17/02/2016 – Version 1