Sonography of Complex Gallbladder Disease - e
advertisement

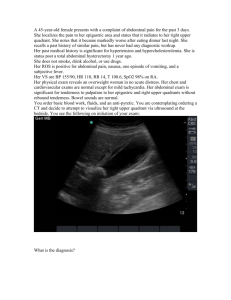
Sonography of Complex Gallbladder Disease Author: Sharlene A. Teefey, M.D. Objectives: Upon the completion of this CME article, the reader will be able to: 1. List the risk factors for gangrenous cholecystitis and describe the sonographic findings seen with this disorder. 2. Categorize the types of gallbladder perforation and the sonographic patterns of pericholecystic fluid. 3. Describe the etiology of acalculous cholecystitis and define the sonographic findings seen with this disorder. 4. Describe the etiology of emphysematous cholecystitis and define the sonographic findings seen with this disorder. Introduction: Recent studies have reported new trends in the patients who develop acute cholecystitis, including a greater incidence in patients who are elderly or diabetic. There has also been an increased incidence of acalculous and gangrenous cholecystitis. This article will review the pathogenesis and the clinical and sonographic features of gangrenous, acalculous, and emphysematous cholecystitis. Gangrenous cholecystitis Gangrenous cholecystitis occurs in approximately 20% of cases of acute cholecystitis. The incidence is equal in men and women. The majority of patients are elderly; however, cases have been reported in younger patients who are immunosuppressed, have a malignancy, or are on steroids. In the elderly population, atherosclerosis and diabetes mellitus are important predisposing factors. The mortality rate for gangrenous cholecystitis is 5% to 10%, and perforation occurs in approximately 10% of cases. While the definition of gangrenous cholecystitis is somewhat variable in the literature, it is considered present when there is histologic evidence of coagulative necrosis (surface ulceration or transmural necrosis) and acute and or chronic inflammation. Gallstones are present in most patients. The pathogenesis begins with impaction of a stone in the cystic duct, followed by the development of bile salt that is more concentrated than normal, which then incites a chemical inflammatory reaction. As mucus production continues, the gallbladder becomes distended, leading to ischemia (a lack of blood flow), necrosis (cell death), and perforation within one to seven days after the onset of symptoms. The signs and symptoms of gangrenous cholecystitis may mimic those of uncomplicated acute cholecystitis (nausea, vomiting, right upper quadrant pain and tenderness, fever, and leukocytosis or elevated white blood cell count), but can also be absent. In our series of 25 patients with gangrenous cholecystitis, at initial presentation, 50% were afebrile, 30% had a nontender abdomen, 20% had no abdominal pain, and 15% had a normal white blood cell count. Two of these signs and/or symptoms were absent in 30% of patients and three or more were absent in 10% (Teefey, unpublished data). Several sonographic findings have been described in patients with gangrenous cholecystitis, including absence of a sonographic Murphy sign, intraluminal membranes, wall irregularity and intramural perforation, gallbladder wall striations, and peri-cholecystic fluid collections. The absence of a sonographic Murphy sign is an important finding, which may occur in up to 67% of patients. The Murphy sign is absent due to necrosis of the visceral afferent nerve fibers supplying the gallbladder. Intraluminal membranes are probably due to a fibrinous exudate or sloughed, necrotic mucosa (figure 1). This finding may be simulated by thick tenacious mucus within the gallbladder lumen or by a multi-septate gallbladder. Irregularity of the gallbladder wall and intramural perforation is due to wall hemorrhage, microabscess formation, ulceration, and necrosis. Striated gallbladder wall thickening appears sonographically as multiple hypoechoic layers separated by echogenic zones (figure 2). We often observed this finding prior to perforation. In our series of 25 patients with gangrenous cholecystitis, gallbladder wall striations were observed in 10 cases, whereas intraluminal membranes and wall irregularity were observed in only 1 case each. Gallbladder wall striations appear to be a frequent, early sign of gangrenous cholecystitis. While striated gallbladder wall thickening is associated with gangrenous cholecystitis, it has also been identified in patients with edema and or inflammation of the wall unrelated to gallbladder disease including those with hepatitis, portal hypertension, right heart failure, renal failure, ascites, hypoalbuminemia, pancreatitis, and obstruction of the lymphatic and or venous drainage of the gallbladder. Thus, although this finding is nonspecific, in the setting of acute cholecystitis, striations suggest gangrenous changes in the gallbladder wall. Gallbladder wall perforation usually occurs in the fundus because the cystic artery branches are end arteries so fresh blood reaches the fundus last. Three types of gallbladder wall perforation may occur: acute, subacute, and chronic. Acute, free peritoneal perforation is rare and results in bile peritonitis. Subacute perforation with peri-cholecystic abscess formation is the most common type. Chronic gallbladder wall perforation with cholecystoenteric fistula formation is unusual. Fistulous communication occurs most frequently with the duodenum and or hepatic flexure (figure 3). In our series of 25 patients with gangrenous cholecystitis, sonography revealed two patterns of peri-cholecystic fluid collections. Type I fluid collections were thin, anechoic crescent-shaped collections adjacent to the gallbladder wall. Type II fluid collections were large, round, and irregular in shape and complex (thick walls, internal debris, or septations). The gallbladder may or may not be identifiable as a separate structure. Type I fluid collections were not typically associated with gallbladder perforation whereas type II fluid collections were nearly always associated with gallbladder wall perforation and abscess formation. Acute Acalculous Cholecystitis Acute acalculous cholecystitis occurs in 10%-14% of cases of acute cholecystitis. It is more common in men than in women (3:1) and usually occurs in patients 50 to 65 years of age. The mortality rate averages 40% and the incidence of perforation is 15%. Predisposing risk factors include previous surgery or trauma, ICU admission, mechanical ventilation, one or more episodes of hypoventilation, prolonged fasting or total parenteral nutrition (TPN) usage, and narcotic use. The pathogenesis of acalculous cholecystitis is multifactorial and includes ischemia, gallbladder stasis, sepsis, and toxins. Ischemia occurs due to hypotension or hypovolemia, especially in postoperative or post-trauma patients or in patients with severe pancreatitis or burns. Atherosclerosis has also been implicated as a cause of ischemia in acute acalculous cholecystitis. In one study, the authors reviewed their seven-year experience with acute acalculous cholecystitis and found that 75% of cases occurred in older men who were healthy, except for atherosclerotic vascular disease. Gallbladder stasis, which occurs in the setting of prolonged fasting, parenteral nutrition, and narcotic use, is another predisposing factor. As bile salts become concentrated, chemical inflammation of the gallbladder wall ensues, leading to cholecystitis. Sepsis also is hypothesized as a cause for acute acalculous cholecystitis. Finally, bacterial endotoxins may activate factor XII dependent pathways, injuring blood vessels in the gallbladder wall. Signs and symptoms of acute acalculous cholecystitis may be similar to those in uncomplicated acute cholecystitis, but may be masked by narcotics, postoperative incisional pain, or a decreased level of consciousness. In one report, only 37% of patients were febrile, 70% had a leukocytosis, and 56% had right upper quadrant pain. In addition, symptoms may be non-localizing, and patients may present with an isolated fever or diffuse abdominal pain. Several reports have described sonographic findings associated with acute acalculous cholecystitis, including gallbladder wall thickening, lumen distension, peri-cholecystic fluid, a positive sonographic Murphy sign, lack of gallbladder contraction in response to cholecystokinin, and the presence of sludge. However, most of these findings are nonspecific and are not very sensitive in diagnosing acute acalculous cholecystitis. Gallbladder wall thickening may be normal in 15% to 30% of cases, especially early in the course of the disease (figure 4). Furthermore, gallbladder wall thickening may be due to several other etiologies, including hypoalbuminemia, ascites, right heart failure, renal failure, and liver disease. Gallbladder distension may not be present when prior inflammation and fibrosis limit the gallbladder’s ability to distend. If the etiology of acute acalculous cholecystitis is ischemia, distension of the gallbladder may also be absent. Alternatively, gallbladder distension may be present in the setting of prolonged fasting, parenteral nutrition, diabetes mellitus, prior vagotomy, or distal common bile duct obstruction. Pericholecystic fluid is not sensitive in diagnosing acute acalculous cholecystitis and may be absent in the early stages of inflammation. The presence of peri-cholecystic fluid also is nonspecific and may occur in patients with peptic ulcer disease, pancreatitis, ascites, or peritonitis. A positive sonographic Murphy sign, while very specific for acute cholecystitis, is frequently absent in the presence of gangrenous changes or may be masked by narcotic use and postoperative pain. The presence of gallbladder sludge is nonspecific and may be observed in prolonged fasting states and parenteral nutrition use. Finally, the inability of the gallbladder to contract in response to cholecystokinin has been reported in postoperative patients with no evidence of gallbladder disease. Emphysematous cholecystitis Emphysematous cholecystitis occurs in approximately 1% of cases of acute cholecystitis. It is more common in men than in women (3:1) and usually occurs in patients 50 to 70 years of age. Diabetes mellitus is present in up to 40% of cases, and cholelithiasis is present in up to 50%. The mortality rate is approximately 15%. Gangrenous changes occur in approximately 75% of cases, with progression to perforation in 20%. Emphysematous cholecystitis is due to ischemia from cystic artery or arteriolar narrowing. Secondary infection occurs from gas-forming organisms, including Clostridium welchii, E. coli, staphylococcus, or anaerobic streptococcus. Signs and symptoms of emphysematous cholecystitis may mimic those of uncomplicated acute cholecystitis or may be unusually severe, with right upper quadrant pain and sepsis. However, in two studies, 30%-50% of patients were afebrile, only 50% had an elevated white blood cell count, and abdominal tenderness was frequently absent. Several sonographic features have been described in patients with emphysematous cholecystitis, including intramural and intraluminal gas. Intramural gas will cause the gallbladder wall to be hyperechoic with posterior reverberation producing comet tail or ring down artifact (figure 5). However, these sonographic findings may be caused by other pathologic conditions. Adenomyomatosis may cause comet tail artifacts in the gallbladder wall that simulate the appearance of intramural gas. A porcelain gallbladder may also produce an echogenic wall, but there is no distal reverberation, which aids in differentiating this condition from emphysematous cholecystitis. Intraluminal gas may produce tiny echoic foci with posterior reverberation that rise toward the nondependent wall. Floating cholesterol crystals may simulate the appearance of intraluminal gas, however, intraluminal gas rises to the nondependent portion of the gallbladder, whereas cholesterol crystals settle in the dependent portion of the gallbladder. In addition, intraluminal gas may be due to multiple other etiologies including biliary-enteric anastomoses or fistulae or an incompetent sphincter of Oddi. Clinical history is important in distinguishing these entities from emphysematous cholecystitis. In summary, gangrenous cholecystitis, acalculous cholecystitis, and emphysematous cholecystitis are entities that are increasing in incidence, have a high morbidity and mortality rate, and may have an atypical and often subtle clinical presentation. Sonographic findings, when observed, must be interpreted within the context of the patient’s overall clinical status, given the low specificity and sensitivity of many of the findings. Figures: 1 Gangrenous gallbladder with intraluminal membranes from sloughed mucosa 2 Striated gallbladder wall thickening from pancreatitis 3 Gangrenous gallbladder with perforation into the liver 4 Acalculous cholecystitis with normal wall thickness and sludge 5 Emphysematous cholecystitis with intramural and intraluminal air References or Suggested Reading: 1. Reiss R, Nudelman I, Gutman C et al. Changing trends in surgery for acute cholecystitis. World J Surg 14:567-571,1990. 2. Roslyn J, Busuttil RW. Perforation of the gallbladder: A frequently mismanaged condition. Am J Surg 137:307-312,1979. 3. Madrazo BL, Francis I, Hricak H, et al. Sonographic findings in perforation of the gallbladder. AJR 139:491-496, 1982. 4. Teefey SA, Baron RL, Radke HM et al. Gangrenous cholecystitis: New observations on sonography. J Ultrasound Med 10:603-606, 1991. 5. Simeone JF, Brink JA, Mueller PR et al. The sonographic diagnosis of acute gangrenous cholecystitis: Importance of the Murphy sign. AJR 152:289-290, 1989. 6. Isch JH, Finneran JC, Nahrwold DL. Perforation of the gallbladder. Am J Gastroenterol 55:451-458, 1971. 7. Strohl EL, Diffenbaugh WG, Baker JH et al. Gangrene and perforation of the gallbladder. Int Abstracts Surg 114:1-7, 1962. 8. Jeffrey RB, Laing FC, Wong W et al. Gangrenous cholecystitis: Diagnosis by ultrasound. Radiology 148:219-221, 1983. 9. Cohan RH, Mahoney BS, Bowie JD et al. Striated intraluminal gallbladder lucencies on US studies: Predictors of acute cholecystitis. Radiology 164:31-35, 1987. 10. Teefey SA, Baron RL, Bigler SA. Sonography of the gallbladder: Significance of striated (layered) thickening of the gallbladder wall. AJR 156:945-947, 1991. 11. Fletcher AG, Ravdin IS. Perforation of the gallbladder. Am J Surg 81:178-185, 1951. 12. Kalliafas S, Ziegler DW, Flancbaum L, et al. Acute acalculous cholecystitis: Incidence, risk factors, diagnosis, and outcome. Am Surg. 64(5): 471-475,1998. 13. Glenn F, Becker CG: Acute acalculous cholecystitis. Ann Surg, 195:31-136, 1982. 14. Johnson LB: The importance of early diagnosis of acute acalculous choleystitis. Surg, Gyn & Obstet, 164:197-203, 1987. 15. Fox MS, Wilk PJ, Weissman HS, et al: Acute acalculous cholecystitis. Surg, Gyn & Obstet, 159:13-16, 1984. 16. Long TN, Heimbach, DM, Carrico CJ: Acalculous cholecystitis in critically ill patients. Am J Surg,136:31-34, 1978. 17. Savoca PE, Longo WE, Zucker KA, et al: The increasing prevalence of acalculous cholecystitis in outpatients: Results of a 7-year study. Ann Surg, 211:433-437, 1990. 18. Shapiro MJ, Luchtefeld WB, Kurzweil S, et al. Acute acalculous cholecystitis in the critically ill. Am Surg 60(5):335-338,1994. 19. Frazee RC, Nagorney DM, Mucha P: Acute acalulous cholecystitis. Mayo Clin Proc, 64:163-167, 1989. 20. Boland GW, Slater G, Lu DS, et al. Prevalence and significance of gallbladder abnormalities seen on sonography in intensive care unit patients. AJR,174:973-977, 2000. 21. Boland GW, Lee MJ, Leung J, et al. Percutaneous cholecystostomy in critically ill patients: early response and final outcome in 82 patients. AJR 163:339-342, 1994. 22. Shuman WP, Rogers JV, Rudd TG, et al: Low sensitivity of sonography and cholescintigraphy in acalculous cholecystitis. Am J Radiol 142:531-534, 1984. 23. Blankenberg F, Wirth R, Jeffrey RB, et al: Computed tomography as an adjunct to ultrasound in the diagnosis of acute acalculous cholecystitis. Gastrointest Radiol 16:149-153, 1991. 24. Cohen SM, Kurtz AB: Biliary sonography. Radiol Clin North Am 29:1171-1198, 1991. 25. Raduns K, McGahan JP, Beal S: Cholecystokinin sonography: Lack of utility in diagnosis of acute acalculous cholecystitis. Radiology 175:463-466, 1990. 26. Nyberg DA, Laing FC. Ultrasonographic findings in peptic ulcer disease and pancreatitis which simulate primary gallbladder disease. J Ultrasound Med, 2:303, 1983. 27. Mentzer RM, Golden GT, Chandler JF, et al: A comparative appraisal of emphysematous cholecystitis. Am J Surg 129:10-15, 1975. 28. Lorenz RW, Steffen HM: Emphysematous cholecystitis: Diagnostic problems and differential diagnosis of gallbladder gas accumulations. Hepato-gastroenterol 37:103106, 1990. 29. Brandon JC, Glick SN, Teplick SK, et al: Emphysematous cholecystitis: Pitfalls in its plain film diagnosis. Gastrointest Radiol 13:33-36, 1988. 30. Gill KS, Chapman AH, Weston MJ. The changing face of emphysematous cholecystitis. Br J Rad 70:986-991, 1997. 31. Franquet T, Bescos JM, Barberena J, et al: Accoustic artifacts and reverberation shadows in gallbladder sonograms: their cause and clinical implications. Gastrointest Radiol 15:223-228, 1990. 32. Bloom RA, Libson E, Lebensart PD, et al: The ultrasound spectrum of emphysematous cholecystitis. J Clin Ultrasound 17:251-256, 1989. 33. Parulekar SG: Sonographic findings in acute emphysematous cholecystitis. Radiology 145:117-119, 1982. 34. Nemcek AA, Gore RM, Vogelzang RL, et al: The effervescent gallbladder: A sonographic sign of emphysematous cholecystitis. Am J Radiol 150:575-577, 1988. 35. Lafortune M, Gariepy G, Dumont A, et al: The v-shaped artifact of the gallbladder wall. Am J Radiol 147:505-508, 1986. 36. Raghavendra BN, Subramanyam BR, Balthazar EJ, et al: Sonography of adenomyomatosis of the gallbladder: Radiologic-pathologic correlation, Radiology 146:747-752, 1983. 37. Kane RA, Jacobs R, Katz J, et al: Porcelain gallbladder: Ultrasound and CT appearance. Radiology 152:137-141, 1984. About the Author: Sharlene A. Teefey, M.D. is currently an Associate Professor of Radiology at the Mallinckrodt Institute of Radiology at Washington University School of Medicine in St. Louis Missouri. She is a member of numerous societies and organizations including the American College of Radiology, the Society of Radiologists in Ultrasound, and the American Institute of Ultrasound in Medicine. She is a reviewer of manuscripts for Radiology, the American Journal of Roentgenology, and Radiographics. She has more than 45 publications in peer review medical journals and has been a speaker at numerous institutions and conferences across the country. Examination: 1. Which of the following statements is (are) true regarding gangrenous cholecystitis? A. It occurs in approximately 40% of cases of acute cholecystitis. B. The majority of patients are very young; however, cases have been reported in elderly patients who are immunosuppressed or are on steroids. C. The mortality rate for gangrenous cholecystitis is 5% to 10%, and perforation occurs in approximately 10% of cases. D. Gallstones are absent in most patients. E. B & C above are true. 2. The pathogenesis of gangrenous cholecystitis begins with impaction of a stone in the A. sphincter of Oddi. B. cystic duct. C. hepatic duct D. pyloric sphincter E. tubal sphincter 3. The signs and symptoms of gangrenous cholecystitis may mimic those of uncomplicated acute cholecystitis, which includes A. nausea, vomiting, and fever B. left upper quadrant pain and tenderness C. a decreased white blood cell count D. all of the above E. only A & B above 4. Several sonographic findings have been described in patients with gangrenous cholecystitis, including A. absence of a sonographic Murphy sign. B. intraluminal membranes and wall irregularity. C. gallbladder wall striations and peri-cholecystic fluid collections. D. all of the above. E. only B & C above. 5. Which of the following statements is (are) true regarding sonography of gangrenous cholecystitis? A The presence of a sonographic Murphy sign is an important finding, which occurs in over 85% of patients. B. Intraluminal membranes are probably due to a fibrinous exudate or sloughed, necrotic mucosa. C. Irregularity of the gallbladder wall and intramural perforation is due to necrosis of the visceral afferent nerve fibers supplying the gallbladder. D. E. Striated gallbladder wall thickening appears sonographically as multiple hyperechoic layers separated by echodense zones. all of the above are true. 6. While striated gallbladder wall thickening is associated with gangrenous cholecystitis, it has also been identified in patients with edema and or inflammation of the wall unrelated to gallbladder disease including those with A. hepatitis and pancreatitis B. left heart failure and hyperalbuminemia C. renal failure and obstruction of the lymphatic and or venous drainage of the gallbladder D. A & C above E. B & C above 7. Three types of gallbladder wall perforation may occur: acute, subacute, and chronic. A. Acute, free peritoneal perforation is the most common but rarely results in bile peritonitis. B. Subacute perforation with peri-cholecystic abscess formation is the most rare type. C. Chronic gallbladder wall perforation with cholecystoenteric fistula formation is unusual. D. all of the above E. only A & C above 8. In the author’s series of 25 patients with gangrenous cholecystitis, sonography revealed two patterns of peri-cholecystic fluid collections. A. Type I fluid collections were thin, anechoic crescent-shaped collections adjacent to the gallbladder wall. B. Type II fluid collections were large, round, and irregular in shape and complex with thick walls, internal debris, or septations. C. Type I fluid collections were not typically associated with gallbladder perforation D. Type II fluid collections were nearly always associated with gallbladder wall perforation and abscess formation. E. All of the above. 9. Acute acalculous cholecystitis A. occurs in 10%-14% of cases of acute cholecystitis. B. is more common in women than in men (3:1) C. usually occurs in patients 20 to 35 years of age. D. A & B above. E. B & C above. 10. Predisposing risk factors for acute acalculous cholecystitis include A. previous surgery or trauma B. admission to the ICU C. mechanical ventilation D. prolonged fasting or total parenteral nutrition (TPN) usage E. all of the above. 11. The pathogenesis of acalculous cholecystitis is multifactorial and includes A. ischemia and gallbladder stasis B. peptic ulcer disease C. sepsis and toxins. D. A & B above. E. A & C above. 12. Which of the following statements is (are) true? A. Gallbladder stasis occurs in the setting of hypertension. B. Gallbladder stasis occurs in the setting of prolonged fasting. C. Gallbladder stasis occurs in the setting of narcotic use. D. all of the above. E. only B & C above 13. The sonographic findings associated with acute acalculous cholecystitis include A. gallbladder wall thinning B. peri-cholecystic fluid and the presence of sludge C. gallbladder contraction in response to cholecystokinin D. all of the above. E. only B & C above. 14. Which of the following statements is (are) true? A. Gallbladder distension may not be present when prior inflammation and fibrosis limit the gallbladder’s ability to distend. B. Peri-cholecystic fluid is very sensitive in diagnosing acute acalculous cholecystitis and is nearly always present in the early stages of inflammation. C. The presence of peri-cholecystic fluid is also very specific and is not really seen with other disorders. D. All of the above. E. Only A & B above. 15. Gallbladder distension may be present in the setting of A. prolonged fasting or total parenteral nutrition. B. diabetes mellitus or prior vagotomy. C. proximal common bile duct obstruction. D. A & B above. E. B & C above. 16. Emphysematous cholecystitis A. occurs in approximately 10% of cases of acute cholecystitis. B. is more common in women than in men (3:1) C. usually occurs in patients 50 to 70 years of age. D. all of the above. E. only A & B above. 17. Emphysematous cholecystitis is due to ischemia from A. B C. D. E. cystic artery or arteriolar narrowing. cystic artery or arteriolar dilation. splenic artery or arteriolar narrowing. splenic artery or arteriolar dilation. gastric artery or arteriolar narrowing. 18. Several sonographic features have been described in patients with emphysematous cholecystitis. Which of the following statements is (are) true? A. Intramural gas will cause the gallbladder wall to be hypoechoic with anterior reverberation producing comet tail artifact. B. Adenomyomatosis may cause comet tail artifacts in the gallbladder wall that simulate the appearance of intramural gas. C. A porcelain gallbladder may produce an echogenic wall and this is confirmed by the presence of distal reverberation D. all of the above. E. only B & C above. 19. Sonographically, floating cholesterol crystals may simulate the appearance of intraluminal gas, however, A. intraluminal gas settles in the dependent portion of the gallbladder B. cholesterol crystals rise to the nondependent portion of the gallbladder C. intraluminal gas rises to the nondependent portion of the gallbladder D. cholesterol crystals remain evenly dispersed within the gallbladder. E. none of the above 20. Intraluminal gas in the gallbladder may be due to A. emphysematous cholecystitis. B. biliary-enteric anastomoses or fistulae C. an incompetent sphincter of Oddi. D. all of the above. E. only A & C above.