Collaborative Pathway – MSK First Learning Session (3.5 hours
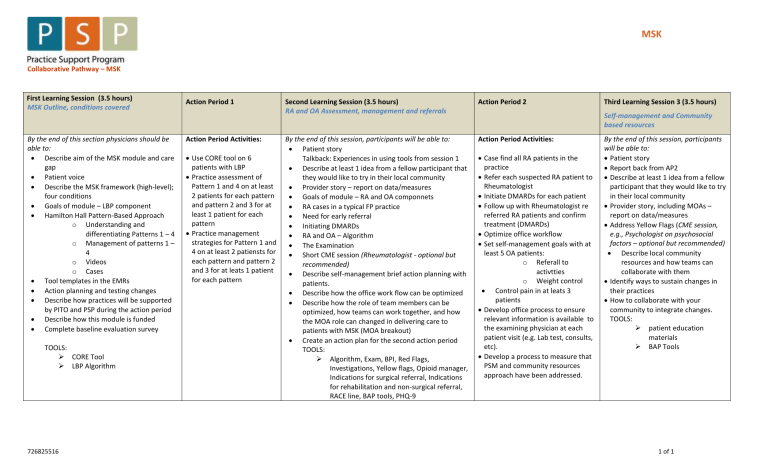
MSK
Collaborative Pathway – MSK
First Learning Session (3.5 hours)
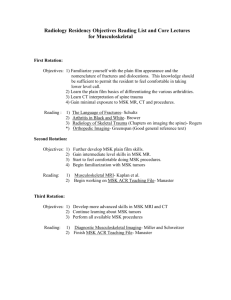
MSK Outline, conditions covered
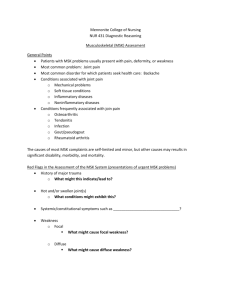
By the end of this section physicians should be able to:
Describe aim of the MSK module and care gap
Patient voice
Describe the MSK framework (high-level); four conditions
Goals of module – LBP component
Hamilton Hall Pattern-Based Approach o Understanding and differentiating Patterns 1 – 4 o Management of patterns 1 –
4 o Videos o Cases
Tool templates in the EMRs
Action planning and testing changes
Describe how practices will be supported by PITO and PSP during the action period
Describe how this module is funded
Complete baseline evaluation survey
TOOLS:
CORE Tool
LBP Algorithm
Action Period 1 Second Learning Session (3.5 hours)
RA and OA Assessment, management and referrals
Action Period 2
Action Period Activities:
Use CORE tool on 6 patients with LBP
Practice assessment of
Pattern 1 and 4 on at least
2 patients for each pattern and pattern 2 and 3 for at least 1 patient for each pattern
Practice management strategies for Pattern 1 and
4 on at least 2 patiensts for each pattern and pattern 2 and 3 for at leats 1 patient for each pattern
By the end of this session, participants will be able to:
Patient story
Talkback: Experiences in using tools from session 1
Describe at least 1 idea from a fellow participant that they would like to try in their local community
Provider story – report on data/measures
Goals of module – RA and OA componnets
RA cases in a typical FP practice
Need for early referral
Initiating DMARDs
RA and OA – Algorithm
The Examination
Short CME session (Rheumatologist - optional but
recommended)
Describe self-management brief action planning with patients.
Describe how the office work flow can be optimized
Describe how the role of team members can be optimized, how teams can work together, and how the MOA role can changed in delivering care to patients with MSK (MOA breakout)
Create an action plan for the second action period
TOOLS:
Algorithm, Exam, BPI, Red Flags,
Investigations, Yellow flags, Opioid manager,
Indications for surgical referral, Indications for rehabilitation and non-surgical referral,
RACE line, BAP tools, PHQ-9
Action Period Activities:
Case find all RA patients in the practice
Refer each suspected RA patient to
Rheumatologist
Initiate DMARDs for each patient
Follow up with Rheumatologist re referred RA patients and confirm treatment (DMARDs)
Optimize office workflow
Set self-management goals with at least 5 OA patients: o Referall to activtties o Weight control
Control pain in at leats 3 patients
Develop office process to ensure relevant information is available to the examining physician at each patient visit (e.g. Lab test, consults, etc).
Develop a process to measure that
PSM and community resources approach have been addressed.
Third Learning Session 3 (3.5 hours)
Self-management and Community based resources
By the end of this session, participants will be able to:
Patient story
Report back from AP2
Describe at least 1 idea from a fellow participant that they would like to try in their local community
Provider story, including MOAs – report on data/measures
Address Yellow Flags (CME session, e.g., Psychologist on psychosocial factors – optional but recommended)
Describe local community resources and how teams can collaborate with them
Identify ways to sustain changes in their practices
How to collaborate with your community to integrate changes.
TOOLS:
patient education materials
BAP Tools
726825516 1 of 1