URINE LUCK: GETTING THE MOST FROM URINALYSIS

Urine Luck: Getting the Most From Urinalysis
Anne Barger, DVM, MS, DACVP
Small Animal Track
2012 ISVMA Annual Conference Proceedings
Understanding the process of urine production is essential to getting the most information for the urinalysis. There are three necessary steps to urine excretion: 1. Glomerular filtration, 2.
Tubular reabsorption from the tubular lumen into the blood and 3. Tubular secretion is the secretion of substrates from blood into the tubular lumen.
Glomerular filtration is an important first step. Many substances such as urea freely pass through the glomerulus but other substances such as albumen are strictly filtered. Tubular reabsorption can be active or passive.
Passive transport is primarily from osmosis. Passive water reabsorption by osmosis is coupled to sodium reabsorption. Active transport requires energy in the form of ATP. In the proximal tubule 65% of sodium, water and chloride are reabsorbed. In the loop of Henle, water and urea are freely filtered and there is active transport of sodium and chloride. The distal tubule avidly reabsorbs sodium, potassium and chloride but is impermeable to water and urea. The collecting duct is impermeable to water in the absence of ADH. With ADH, the collecting duct becomes are major source of water reabsorption. Tubular secretion consists of active release of substances by the tubular epithelial cells into the lumen of the nephron. Tubular secretion controls the electrolyte balance. Large amounts of potassium and hydrogen can be secreted by the tubular epithelial cells.
The concentrating ability of urine is an important aspect to evaluate. Dilute urine is formed by continually reabsorbing solute from the urine. Dilution of urine still requires effort on the part of the renal tubule and indicates that the nephron is still functional. Urine is concentrated by reabsorbing water. ADH, functioning nephrons, adequate levels of sodium and urea are essential to this process.
Urinalysis
Collection of urine can influence interpretation and significance of material observed in the sediment. Each methodology has advantages and disadvantages. Free catch or voided sample is minimally invasive collection method and can give accurate information about concentrating ability however some unusual items may be observed in the urine sediment.
Pollen grains, plant material and bacterial organisms are commonly identified in samples collected by free catch so this is not the ideal sample for culture. Urinary catheterization is a bit more invasive but can still be traumatic to the patient. It is common to see squamous and transitional epithelial cells in a sample collected by urinary catheterization. Cystocentesis is the best sample for culture however it is also the most invasive method. Blood contamination occurs with this method but usually not enough to discolor the urine.
Examination of Urine
Urine should be examined as soon as possible. Many things can change quickly in urine, chemically and within the sediment so if it cannot be examined immediately or if it is being sent out to a laboratory, refrigeration is recommended.
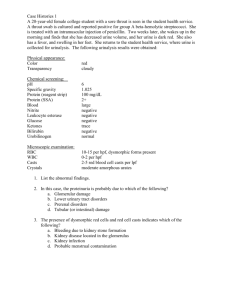
Every urinalysis should begin with gross examination of the urine. Color, clarity and aroma are all part of this examination. Normal urine color is yellow due to the presence of urochrome and urobilin. When urine is red, it is likely due to red blood cells or hemoglobin. Dark yellow to brown urine indicates the presence of bilirubin and reddish brown urine may be from
hemoglobin or myoglobin. Normal urine should be clear, clear enough to read text. Cloudy urine indicates an active sediment which means there are cells, crystals, mucus, bacteria, casts or even sperm in the urine. Even normal urine has an aroma. Pathologic processes which can give urine a nasty odor include ammonia, protein breakdown and ketonuria.
The next step to urine evaluation is determination of the concentration. The most widely used method is specific gravity. This method utilizes a refractometer and can easily be performed in most general practices. Urine specific gravity or USG is the ratio of the weight of a volume of urine to the weight of the same volume of water. It provides a general assessment of the functioning capacity of the tubules and collecting ducts. USG has a normal wide range or 1.001 to 1.065 in the dog and up to 1.080 in the cat. It is necessary to correlate the USG value with the hydration status of the patient. We categorize urine concentration by how much it has deviated from the specific gravity of the urine when it entered the glomerulus. Hyposthenuric urine has a USG of 1.001-1.007. This indicates that solute has been removed from the urine and nephron is able to dilute the urine. Isosthenuric urine has a range of 1.008-1.012. This indicates that the urine has not changed since it passed through the glomerulus. This could be normal for a well hydrated patient or may suggest renal failure. Urine can become isosthenuric when 66% of the nephrons are not functioning. Dehydrated patients should have concentrated urine. If an animal is >3% dehydrated ADH should cause the renal tubules to concentrate the urine.
Determination of urine chemistry is a very easy in-house test that can be performed using urine dipsticks. pH, glucose, ketones, protein, bilirubin, and blood can all be identified. Urine dipsticks can be an insensitive method for evaluation of protein, so other testing such as protein:creatinine or microprotein analysis should be performed. There are some limitations to the urine dipstick. Certain medications can cause false positives on the urine dipstick, particularly Cephalexin and Enrofloxacin can give a false positive reaction. The nitroprusside test used to identify ketones reacts with acetone and acetoacetone but is insensitive to
hydroxybutyric acid which is the most common ketone in dogs and cats. There is an ELISA test method available to detect small amounts of protein in the urine which is more sensitive than the urine dipstick.
Urine sediment
After the urine chemistry and specific gravity are performed it ’s time for the examination of the urine sediment. The urine should be centrifuged for 5 minutes. The supernatant is poured off and the sediment is resuspended in a few drops of the remaining supernatant. A drop of sediment is placed on a glass slide and is covered with a cover slip. The sediment is scanned at 10x (lpf) and then at high power or 40x. No oil is necessary for examination of urine sediment. If interesting cells or structures are examined in the sediment, the sample can be preserved by painting the edges of the cover slip with nail polish. Structures identified in the sediment include cells, crystals, casts, microorganisms and other structures. Several different cell types can be observed including epithelial cells (squamous, transitional and renal tubular), red blood cells and white blood cells. Squamous epithelial cells exfoliate from the distal urethra and vagina. The presence of these cells is not considered pathologic unless the morphology of the cells is unusual. Transitional epithelial cells can exfoliate from the proximal urethra, urinary bladder, ureters and renal pelvis. These cells may be observed in high numbers, even in clusters from catheterized samples. These cells do not necessarily indicate disease unless they appear morphologically abnormal. The presence of renal tubular epithelial cells in the urine indicates renal pathology. These cells are often accompanied by casts. Red and white blood cells are quantitated per high power field. >3-5 cells/hpf is considered abnormal and may indicate hemorrhage or inflammation. RBCs can be round or Crenated depending on the
specific gravity. If the specific gravity is too low, the RBCs may even lyse. WBCs can lyse in alkaline urine. The presence of increased numbers of WBCs indicates an inflammatory process within the urogenital track.
Casts occur when there is damage to the nephron, primarily the renal tubule. If the tubule is damaged, it secretes a protein, called Tamm-Horsfall protein. This protein fills the tubule and encompasses any material that happens to be in the tubule at that time. If there is inflammation or hemorrhage in the tubule white blood cell casts or red blood cell casts, respectively, may be observed in the sediment. If there is cellular debris within the tubule, granular casts will be observed. Casts are intermittently shed and therefore do not indicate severity of disease but the presence of waxy casts indicates chronicity. There are many different types of casts in addition to those already mentioned. Hyaline casts are pure protein and may be observed with glomerular disease and epithelial casts consist of renal tubular epithelial cells.
The most common microorganisms observed in urine sediment are bacteria. Bacteria observed in a free catch sample must be interpreted with caution unless there are many white blood cells present. Urine is considered sterile until the miduretha so a catheterized sample or cystocentesis is preferred for collecting a sample for culture. Fungal organisms are usually considered a contaminant however Blastomyces dermatitidi s and Cryptococcus neoformans have been diagnosed in urine.
Formation of urine crystals is affected by a number of variables including, pH, temperature and medications given. Refrigeration can actually induce crystal formation. Presence of particular crystals can indicate very specific diseases. For instance, ammonium biurate crystals often indicate decreased hepatocellular function in most animals but may be normal for Dalmations.
Tyrosine crystals can also indicate liver disease. Calcium oxylate dihydrate crystals may be normal in small animals but calcium oxylate monohydrate crystals are associated with ethylene glycol toxicity. Calcium carbonate crystals are considered normal in the horse and the rabbit.
Certain medications are known to induce crystal formation such as sulfonamides, allopurinol and ampicillin.
It is not uncommon to identify other structures in urine sediment. Fat droplets are very common and can be challenging to differentiate from red blood cells. Plant material or pollen grains can mimic microorganisms or parasite eggs so it is important to identify these structures as contaminants.
In conclusion, the urine is packed with useful information that is essential for diagnosis. It is an inexpensive, convenient test that can easily be run as an “in-house” test.