Policy Guidelines – Peer - New Zealand Institute of | Rural Health
advertisement

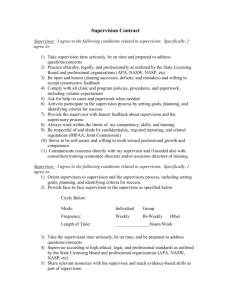
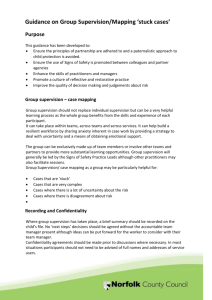
Policy and Guidelines Peer Group Supervision Issued: Authorised: Contents 1.0 Introduction 2.0 Purpose and Scope 3.0 General Policy Statement 4.0 Clinical Supervision 4.1 Principles 4.2 Frameworks 5.0 Peer 5.1 5.2 5.3 5.4 6.0 Participant Rights and Responsibilities 6.1 Rights of the Supervisee 6.2 Responsibilities of the Supervisee 7.0 Peer Group 7.1 Rights of the Peer Group 7.2 Responsibilities of the Peer Group 8.0 Peer Group Supervision Management 8.1 Contracts 8.2 Recording and Documentation of Clinical Supervision Sessions 8.3 Risk Management 8.4 Training Required 8.5 Implementation, Monitoring and Review Group Supervision Aims Process Suggested Structure Long distance peer group supervision Appendices Appendix Appendix Appendix Appendix Appendix I – Professional Supervision Peer Group Contract II – Peer Supervision Record III – Nursing Council Competencies IV – Peer Group Supervision Audit Tool V – Rural Health Clinical Supervision Risk Profiling Tool References/Bibliography 2 1.0 Introduction Clinical supervision supports evidence based, high quality and safe patient care, by encouraging practitioners to learn from experiences in the work place. It brings practicing health care staff together to reflect on practice and encourages the development of professional skills. This enhances the quality of patient care through the implementation of an evidenced based approach to maintaining standards of best practice. Much of the benefit of clinical supervision is reliant upon listening to, recognising and facilitating the supervisee(s) to become selfreflective and ultimately generate their own solutions in defining a positive outcome-based action plan. 2.0 Purpose and Scope The aim of this policy is to provide a formalised framework for the development, and implementation of clinical supervision, underpinned by international and local guidelines. This policy will apply to all clinical staff employed within..................................... Clinical supervision is advised for all grades of clinical staff. This includes the following groups: Employed staff who have direct contact with patients/clients nurses Health care assistants Public Health nurses, District nurses Midwives Well child nurses (Tamariki Ora nurses) Practice Nurses Nurse specialists Nurse Practitioners This policy outlines the process for clinical/professional supervision and the responsibilities of clinical staff and reinforces the importance and value of clinical staff having the opportunity to reflect on clinical interactions as a means of practicing effectively and safely, to improve practice and to identify learning and development needs. 3.0 General Policy Statement Clinical supervision will: Support and enhance practice for the benefit of patients Maintain and improve standards of care Promote evidence based best practice Provide a practice-focused professional relationship Promote reflective practice Be organised, planned and systematic Be conducted within agreed boundaries Be evaluated against the contract (Appendix 1), within agreed time scales.............................................will: Support all clinical staff with protected time to access clinical supervision. Provide training for clinical supervisors and supervisees. 3 Organisational Benefits There are a number of benefits in providing clinical supervision to staff which include: Supervision can be used as a workforce development strategy or as a human resource strategy by providing an approach which addresses factors which impact on the workers ability to function effectively. Supervision can help prevent and reduce the effects of stress and burnout by providing emotional support. Supervisees have reported that regular supervision relieves the negative effects of isolation and improves staff relationships. Reviewed literature reports good quality supervision is a key component of effective staff retention. (VHA, 2008). 4.0 Clinical Supervision 4.1 Principles 4.2 To To To To To To safeguard standards of practice; develop the individual personally and professionally; promote excellence in healthcare; be practice focused; empower staff and patients; facilitate professionally accountable practitioners. Frameworks The framework of clinical supervision for clinical staff in ...........................will be peer group supervision. However, in some circumstances, one-to-one supervision may be the framework of choice. The choice of framework will depend on both staff and service needs and will be at the discretion of line managers/professional leads. 5.0 Peer Group Supervision In peer group supervision each member takes responsibility for supervising and being supervised. There is no permanent supervisor who is overall responsible for the group rather each member takes their turn in taking up the facilitator role and the supervisee role. Within the initial agreement all participants agree to participate equally in the roles and responsibilities of both supervisor and supervisee. All peer group supervision requires the members to have attended training through a workshop. Peer group supervision is based on a number of clinical staff who agree to work together. Groups should be a minimum of 3 to a maximum of 6 clinical staff; they should be from the same discipline, work in the same team/service area or share a commonality e.g. palliative care. 4 5.1 Aims Provide an opportunity for clinical staff to review and clarify clinical issues, within a safe and challenging environment Provide clinical staff with evidence of clinical supervision Promote reflective practice Identify a forum for staff and service developments Explore the management of clinical risk Provide a mechanism for identifying gaps in service and to develop action plans to address those gaps Fulfill the principles of clinical supervision Process of Peer Group Clinical Supervision Clinical supervision sessions provide a safe, supporting and challenging environment characterised by trust and confidentiality where set members work on issues and solve problems through a process of reflection and action. It also provides a particular structure to a group which, although simple, radically alters the normal flow of conversation. The supervisee presents the issue to the group in order to reflect upon and explore ways of addressing the issue. The group members act as supporters, listening, observing, commenting and questioning the supervisee with the aim of assisting in the exploration of the issue and in forming action points. The facilitator enables this interaction to be most useful to the supervisee through facilitation. 5.2 Suggested Structure for a Peer Supervision Group Session Facilitator Always appoint a facilitator for the session whose responsibility is to keep the group on task, keeping to the structure, agenda, and time keeping (the person facilitating alters each time to ensure everyone takes turns). Minutes Minutes are recorded and a minute recorder is allocated on the roster/facilitation plan (this alters each time to ensure everyone takes turns), or the facilitator can record the minutes. Main points of the session are documented and distributed to each of the supervisees using the record of clinical supervision form this will provide evidence of attendance at the individual’s annual appraisal and nursing council competencies. Check In Everyone checks in at the beginning, how they have been at work etc before starting on the agenda. Peer Supervision The first person on the roster/facilitation plan presents their dilemma or issue. Their peers ask reflective questions, give feedback or share knowledge if requested until the supervisee has been able to reflect on the issue explore options and come up with some actions. The facilitator ensures that the first person takes no more than 20 minutes in total. The next person on the roster then gets a chance to reflect on their issue and the same process is used as before. Check Out The group review the session, what was useful, any changes they want to suggest or anything else they need to do. The facilitator ensures the next person due to facilitate according to the facilitation plan/roster knows it’s their turn and 5 the time, date and venue for the next session is confirmed. Those who are due for supervision next time are asked to remember to bring an issue/dilemma etc next time. 5.4 Long distance Peer Group Supervision When group members live in rural or isolated areas peer group supervision can be conducted via Skype which is an internet program which can be downloaded free from: http//:www.skype.com/intl/en/ By using a conference call the group members can speak at little or no cost. It is advisable that prior to the commencement of Skype sessions that the members have had some contact via email to share some information. If one member cannot attend physical for a reason they could attend via Skype instead. 6.0 Participant Rights and Responsibilities 6.1 Rights of the Supervisee The supervisee can expect the following rights within the supervision process: To be treated with respect and as an equal partner in the supervision relationship To confidentiality, with the exception of revealing anything that endangers patient safety, breaks the law, trust policy or professional codes of conduct To protected time to access a minimum of six hourly clinical supervision sessions a year, equivalent to 6 hours To protected space, in private with no interruptions To talk openly without fear of reprisal or criticism, about any difficulties, issues or feelings of vulnerability 6.2 Responsibilities of the Supervisee The supervisee is expected to undertake the following responsibilities within the supervision process: To attend a minimum of one hours of clinical supervision, six times a year, equivalent to 6 hours and to provide evidence of this to their line manager at their annual appraisal. To prepare for clinical supervision by identifying ongoing clinical/professional issues To manage their own time and give booked sessions high priority To be punctual and attend the full session To arrange service cover to enable business continuity To be open to and be prepared to challenge with positive intent To give feedback to the supervisor regarding their facilitation techniques e.g. what is helpful, what is least helpful To use the protected time to reflect in depth on issues affecting clinical/professional practice and avoid non-productive conversation To set an agenda to meet clinical needs 6 7.0 Peer Group 7.1 Rights of the Peer Group The peer group can expect the following rights within the supervision process: To be treated as equal partners in the clinical supervision relationship To break confidentiality relating to anything that endangers patient safety, breaks the law, trust policy or professional codes of conduct To challenge any behaviour or values that the supervisee displays which raises concerns regarding their practice, development or use of clinical supervision To refuse requests which make inappropriate demands on them within their supervision group. To set personal and professional boundaries on issues to be discussed To choose whether or not to work with a group 7.2 Responsibilities of the Peer group The peer group members are expected to undertake the following responsibilities within the supervision process: To be registered with a relevant body e.g. Nursing Council and at least one member to have 18 months or more clinical experience. To prepare for the supervision session, ensuring the venue is appropriate with no interruptions. To prioritise agreed appointments, and ensure time boundaries, the supervision contract and agreed confidentiality is met. To ensure that management or educational assessment is not part of the supervision To encourage the supervisee to seek specialist advice or help where necessary To challenge any behaviour that the supervisee displays which raises concerns about their practice, development or use of supervision 8.0 Peer Group Supervision Management 8.1 Contracts Prior to commencing any supervision session the peer group members must agree and sign a contract (Appendix 1). The clinical supervision contract should contain the following: The aim of the clinical supervision session is to enable the supervisee to reflect in depth on issues affecting practice in order to develop personally and professionally towards achieving, sustaining and developing high quality best practice The frequency, timing and location of the clinical supervision sessions. The contract should be personalised and have agreed, planned sessions, subject to review Records must be distributed to each individual to provide evidence at appraisal and for nursing council competencies Agreed timing of reviews and evaluation of the effectiveness of clinical supervision. Preparation for sessions and the responsibility for bringing agenda items Details of the development and learning points to be actioned Lines of communication Agreement on the occasions when confidentiality may need to be broken 7 8.2 Frequency of contract review Details of new members or changes in membership Recording and Documentation of Clinical Supervision Sessions The following is recommended: Each clinical supervision session should be recorded on the supervision record sheet (Appendix 2) Documentation of the session should be discussed with, agreed by and signed by all the peer group members. Any differences of opinion should be clearly noted. All actions to be undertaken by the supervisee or other group members must also be documented. Copies of the documentation will be held by the supervisee and in a central group folder. Access to the clinical supervision record by anyone other than the supervisee would be in exceptional circumstances (i.e. as part of a disciplinary, legal process or audit). The supervisee(s) would in all circumstances be informed that their records were to be accessed. All registered and non-registered staff are required to record attendance at supervision, and in particular learning and development resulting from it, as part of their professional portfolio. 8.3 Risk Management Clinical supervision is a key mechanism supporting clinical governance by enabling practitioners to examine their practice, their skills, knowledge, attitudes and values in a safe environment. Effective participation in clinical supervision is seen as individuals demonstrating accountability and taking responsibility for the continuous improvement of their practice. Having a structured approach to aid deeper reflection on clinical practice; lead to improvements in practice and patient care, and contribute to clinical risk management. The risk assessment tool in appendix 4 can be used to assess the supervisee’s vulnerability and need for the support provided by peer group supervision. 8.3 Training Requirements ...............................have a responsibility to provide and resource training needs and facilitate staff attendance. All staff receiving peer group supervision will be required to have a basic understanding of: The principles of clinical supervision The supervision contracting process The roles and responsibilities of the supervisee and the peer group members Techniques of reflective practice The process of the supervisory relationship Ethical and legal issues Supervision models and frameworks Facilitation skills Group supervision 8 8.5 Implementation, Monitoring and Review .......................... is responsible for ensuring that this document is reviewed and, if necessary, revised in the light of legislative guidance or organisational change. Review shall be at intervals of no greater than 3 years. Any revisions to this document shall be agreed through ...........................................approval processes A copy of this policy will be placed with all other policies on ...................... intranet, internet and Provider Services internet site. All peer group members will be required to read the policy and sign to state that the policy has been read and understood. This policy is subject to annual audit of compliance 9 Appendix I Clinical Supervision Peer Group Contract As supervisor and supervisee’s we all agree to the following: Aim The aim of our sessions together are to enable the peer group members named below to reflect in depth on issues affecting their practice in order to develop both personally and professionally towards achieving, sustaining and developing a high quality of practice. Meeting The group will meet once a month at an agreed date and time. The meetings to be held at lunch time 12 to 1pm, 1pm to 2pm. The peer group members and supervisor will ensure protected time and space to reflect in depth by sticking to agreed appointments and time boundaries, being punctual, ensuring privacy and no interruptions. Record of Meeting Records of dates and times of supervision sessions or any notes of the meeting will be kept by both in the peer group folder and by the supervisee’s and any copies or use of these records will only be when explicitly agreed by all parties, for example when used within a supervisee’s portfolio. Agenda The supervisee’s will be responsible by preparing for the session and bringing to the supervision areas of practice they wish to reflect on. Responsibility Supervisee The supervisee’s will take responsibility for making effective use of the time, for outcomes and any actions needed as a result of the supervision. Also ensuring each member has the opportunity to participate equally in the supervision session. The supervisee is willing to be challenged and supported to learn and make change. As a group the supervisees will keep confidential all information discussed within the group sessions. Peer Group Members We agree to keep all personal information revealed within the supervision session confidentially except for the following exceptions: Unsafe, unethical, or illegal practice is revealed and the supervisee is unwilling to go through the appropriate organisational procedures to deal with the situation The supervisee consistently fails to turn up for supervision sessions or fails to use the time constructively. In the event of an exception occurring the peer group members will: Attempt to persuade and support the supervisee involved to deal with the issues appropriately. Check that this has been done If it had not been dealt with as a last resort the supervisor will reveal the relevant information to the appropriate person/organisation. The peer group members will offer support, catalytic help, supportive challenge and information or advice to enable the supervisee’s to reflect in depth on issues affecting their clinical practice. The peer group members will use their own 10 clinical judgment to support challenge and develop their own abilities in working with the supervisee’s without breaking confidentiality. The supervision session format, time, venue, effectiveness etc will be reviewed after 6 months and at further agreed intervals. Peer Group Members Name Signature Date 11 Appendix II Peer Supervision Record Date: Facilitator: Supervisee: Other Group Members: Cases and Issues 1 2 3 Case History or Identified Problem: Main Issues Identified: 1. 2. 3. 4. 5. What’s been tried so far: 12 On reflection what decisions/actions to be taken: This is a true record of the supervisees practice. Signed ……………………………………….. Signed ................................................................. Peer Group Members Date………………………………. Peer Group Members Signed................................................ Signed.................................................... ……………………………………….. Supervisee Date………………………………… 13 Appendix III New Zealand Nursing Council Competencies In order to link the nursing practice identified in the peer group supervision with the nursing council competencies the following can be used to highlight which area is being demonstrated. Nursing Council Competencies include: Professional Responsibility E.g. Comply with legislation, 1a, nursing practice, 1b delegation, 1c clients rights, 1d ethical principles, 1e, seek guidance on professional, ethical, cultural issues Safe Environment e.g. (2a,identify and manage risk, 2b, Implement nursing responses/policies for risk management, 2c recognise and respond to changes in client health status including critical events, initiate immediate response). Professional Development e.g. (3a, Participate in evaluation of own practice, 3b, use evidence based practice, 3c, proactive in seeking professional development). Quality e.g. (4a, Use quality improvement principles within own practice, 4b, Identify and participate in quality improvement activities, 4c, implement changes in practice if necessary). Health Promotion e.g. (6a, proactive in health promotion, illness prevention, community development, 6b, uses goals objectives, cultural safety and evidence based practice as key elements in planning/presentation of health promotion activity, 6c use Tikanga Maori concepts relevant to health promotion) Health Education e.g. (7a, Ensure education for the client is, consistent, timely, culturally safe and appropriate for their needs, 7b, use appropriate resources, formal and informal appropriate for the client group). Communication e.g. (8a uses variety of communication skills to establish rapport and trust with client, 8b, Demonstrate skills in problem solving/and or conflict resolution, 8c, advocate for the client when requested by the client). Collaboration and Co-ordination e.g. (9a Contributes and participates with others in the health care team to meet NZ health strategies objectives, 9b, Collaborates, consults and provides accurate information to the client and other health professionals, 9c, Co-ordinates, maintains and documents timely information to maximise health outcomes for client. 14 Sphere Met Not Met Not applicable Evidence Professional Responsibility Legislative and ethical requirement Safe environment Professional development Quality Professional nursing practice Nursing Process Health promotion Health Education Professional relationships Communication Collaboration and Co-ordination Identified Education and professional development: Appendix IV Peer Group Supervision Audit Tool Please circle the answer which is most appropriate for you. I have attended the peer group supervision sessions in the last 6 months 15 100% 75% 50% 25% 0% The timing of the peer group supervision session suits me 100% 75% 50% 25% 0% 50% 25% 0% The venue suits me 100% 75% I find it easy to reflect on issues with my peers within the group 100% 75% 50% 25% 0% 25% 0% The sessions are run in a structured way 100% 75% 50% The peer group supervision sessions have positively contributed to my professional development and nursing practice 100% 75% 50% 25% 0% I feel more validated and supported in my role since starting peer group supervision 100% 75% 50% 25% 0% Please take the time to briefly comment (positive and negative) on the peer group supervision you are receiving with any ideas you may have for ways to improve it. 16 Appendix V Rural Health Clinical Supervision Risk Profiling Tool Dimension Level of experience or competence generally Low Risk = 1 Senior Practitioner – Highly experienced practitioner with ongoing continuing education Regional Centre (Greater access to a pool of peer and senior professionals, infrastructure etc) Moderate Risk = 2 Established or competent practitioner in general clinical areas High Risk= 3 New Graduate at entry level competency in general clinical areas Rural Location (More limited access to a pool of peer and senior professionals, infrastructure etc) Professional Isolation High opportunity for formal and informal discipline-specific supervision. E.g. larger department Discipline Clinical Supervision culture Higher levels of CS education, training, perceptions and expectations. e.g. Social work and Psychology Formal agreement, Training and funding support for CS. Strong processes, clear roles, flexible modes of delivery Little to no involvement in areas of practice which Moderate opportunity for formal and informal discipline-specific supervision. E.g. Multidisciplinary team (only) or Virtual dept Moderate levels of CS education, training, perceptions and expectations. Very Remote or Remote Location (poor access to a pool of peer and senior professionals, infrastructure etc) Low opportunity for formal and informal discipline-specific supervision. E.g. Sole Practitioner Geographic remoteness Level of organisational support Exposure to areas of work with inherent clinical, professional or Adhoc, Training and funding support for CS. Less defined processes, unclear roles, less flexible modes of delivery Work in areas of moderate risk (e.g. Lower levels of CS education, training, perceptions and expectations. No formal agreement Poor access to trained supervisors Poor access to IT, communications and other infrastructure High level of involvement in areas of practice which Score personal risk present high clinical or personal risk (physical or psychological) Level of experience/competence within a specialty Senior Professional with both training and experience within specialty Overall Risk: 7-11 = Low Risk 12-16= Moderate Risk 17-21 = High risk NSW Institute of Rural Clinical Services and Teaching. (2008 Home visits) or moderate level of involvement in areas of practice which present high clinical or personal risk (physical or psychological) Competent practitioner, with specialist training and/or experience present high clinical or personal risk (physical or psychological) E.g. Mental Health, Novel Practitioner within specialty, may be experienced generalist with recent shift into more complex role Total 2 References/Bibliography Bond, M., & Holland, S. (1998). Skills of clinical supervision for nurses: a practical guide for supervisees, clinical supervisors, and managers. Buckingham, Philadelphia : Open University Press. Department of Health. (UK) (1993) A Vision for the Future: The Nursing, Midwifery and Health Visiting Contribution to Health and Health Care. London: The Stationery Office NSW Institute of Rural Clinical Services and Teaching. (2008). A Report: Clinical Supervision for Allied Health Professionals in Rural NSW: Accessed from www.ircst.health.nsw.gov.au on 06/12/2010 NZNO. (2005). NZNO Position Statement for: Professional and Clinical Supervision: Accessed from www.nzno.org.nz on 06/12/2010 Victorian Healthcare Association. (2008). Clinical Supervision and Leadership in Community Health Literature Review. Accessed from http://www.vha.org.au/uploads/Clinical%20Supervision_Background%20_Final_. pdf on 07/12/2010