ENDOCRINOLOGY AND METABOLIC DISEASES
advertisement

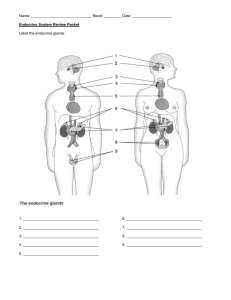
ENDOCRINOLOGY AND METABOLIC DISEASES MODUL II C HYPERLIPOPROTEINEMIAS AND PATHOGENESIS OF ATHEROSCLEROSIS 1. Physiology of lipoproteins a. Lipoprotein classes b. Lipoprotein composition c. Lipoprotein synthesis and function d. Reverse cholesterol transport e. Physiological values of basic lipid parameters 2. Hyperlipidemia a. Types of hyperlipidemia b. Pathophysiology mechanisms of HL c. Secondary HL 3. Therapy of HL a. Dietary therapy b. Hypolipidemic drugs (types of, indications, side effects) c. Therapy goals in primary and secondary HL 4. Atherosclerosis a. Pathogenesis of atherosclerosis (endotelial dysfunction, stable and unstable placque, composition of atheroma) b. Risk factors of atherosclerosis c. Clinical manifestation of atherosclerosis d. Theoretical possibilities of treatment of atherosclerotic diseases OBESITY A. Demonstration of a patient I. History of an obese patient a. Ethiopathogenetics factors of obesity endogenic (genetics, endocrine factors etc.) and exogenic factors (nutrition, physical activity, social environment, psychosocial aspects) b. Complications of obesity (metabolic complications, cardiovascular, endocrine, gastrointestinal, urogenital and musculosceletal diseases) II. Examination of an obese patient with respect to the above mentioned factors III. Basic approach to the therapy of obesity B. Seminar I. Definition of obesity II. Evaluation methods of body composition and fat distribution III. Clinical aspects of obesity IV. Ethiopathogenesis of obesity – new findings (candidate genes regulating the energy metabolism, dietary intake, metabolism of fat tissue) V. Treatment of obesity today Literature: Kopelman PG : Clinical Obesity , Blackwell Science, Oxford 1998; Internet: www.obesita.cz; www.nugenob.com NUTRITION STATUS OF A PATIENT, METHODS OF EVALUATION 1. 2. 3. 4. Personal and family history, nutrition history Clinical investigation (aspection and basic physical methods for malnutrition evaluation) Biochemical examination of blood and urine Anthropometric measurements, body height and weight, wait to hip ratio, BMI calculation, measurement of subcutaneous fat layer 5. Evaluation of nutritional consumption Nutrition toxicology 1. Toxic substances in the food, their evaluation and risk regulation. Biotransformation and interaction of toxic substances in the body, possibilities of therapy. Impact on the organism. Limits. Monitoring. 2. PCB, DBF and dioxines 3. Possibilities of exposition. TDI. 4. Toxic congeners PCB, PCBF, PCDD. International toxic equivalent (I-TEQ). 5. Risk for health. PCB as endocrine disruptor. 6. Phtalic acid esters (sources of exposition, limits, toxic effects, risk for health) 7. Dietary toxic substances for thyroid gland 8. Mycotoxines Vitamins – homework Fat soluble and water soluble vitamins – sources, needs, function, symptoms of hypo- and hypervitaminosis of each vitamin CLINICAL NUTRITION 1. Risks and consequences of malnutrition - general risks of malnutrition - consequences of malnutrition for critical patient, clinical foundations with specific nutritional deficiency, medication with impact on nutrition 2. Diagnostics of malnutrition - clinical methods of nutrition status of evaluation - physical examination and history - body height, weight, BMI, anthropometric data - nutritional score systems: SGA, MNA, PNI - laboratory methods - indirect calorimetry - bioimpedance - energy and metabolic balance 3. Nutritional support, parenteral and enteral nutrition - options for nutritional support - specific aspects of parenteral (PN) and enteral (EN) nutrition - physiology effects, advantages and disadvantages of EN - how to perform EN - difficulties, risk and complications of EN - physiology effects, advantages and disadvantages of PN, all-in-one system - how to perform PN - difficulties, risk and complications of PN - methodology of nutritional support, perioperative PN and EN 4. Nutritional support in special situations - critically ill patient - perioperative nutrition - gastroenterology - short bowel syndrome - oncology - gerontology - out-patient forms of nutrition support BODY FLUIDS AND ITS MOST IMPORTANT IONS A. Repetition – Na+, K+ 1. Normal values 2. Importants 3. Hormone regulations (aldosteron, ADH, ANF) 4. Pathophysiology: causes and mechanisms of sodium and potassium dysbalance B. Calcium 1. Normal values (total stores in the body) 2. Impacts a. neuromuscular excitability b. excitation – contraction in smooth muscle and myocardial cells c. messenger (in target cells of endocrine system) d. tight junction between cells e. coagulations 3. Metabolism of calcium – short time and long time regulation 4. Hormonal regulation a. PARATHORMON: parathyroid effect on bone (rapid and slow release of calcium from bones) effect on kidneys (calcium reabsorption, phosphate excretion, vit.D activation b. CALCITONIN c. VITAMIN D 5. Calcium metabolism disturbances (their causes and consequences) a. hyperparathyroidism: primary-, secondary-, tertiaryb. hypoparathyroidism c. vitamin D: hyper- and hypovitaminosis hypocalcemia hypercalcemia bone metabolic disease Literature: Calcium metabolism: http://blue.vm.temple.edu/~pathphys/general/tablecontents.html http://www.merck.com/pubs/mmanual/section2/chapter12/12d.htm The Thyroid and Parathyroid Glands: http://arbl.cvmbs.colostate.edu/hbooks/pathphys/endocrine/thyroid/index.html http://endocrinesearch.com/ Control of Ca and Phosphate: http://www.members.aol.com/Bio50/LecNotes/lecnot34.html Metabolic Bone Diseases http://edcenter.med.cornell.edu/CUMC_PathNotes/Skeletal/Bone_04.html BASIC PATOPHYSIOLOGY OF ENDOCRINE SYSTEM I. Endocrine glands II. Definition of hormones A. Traditional: Informative molecule produced and liberated by specific endocrine gland in to the blood stream and to distant target organs. There the hormone introduces physiologic respond (the hormone changes the speed and extension of the existing reaction or initiates a new reaction. B. Modified definition – depends on different compartments of action 1. endocrine 2. paracrine 3. autocrine 4. neuroendocrine 5. immune C. Comparison with nervous and immune system III. Role of endocrine glands A. Synthesis of hormones B. Storages of hormones C. Secretion of hormones IV. Transport of hormones – the levels of circulatory hormones depend on: A. The rate of secretion Stimulators of secretion 1. Chemical stimules e.g. glucose stimulates secretion of insulin in pancreas 2. Neural stimules e.g. acetylcholine stimulates secretion of epinephrin and norepinephrin in adrenal medulla 3. Hormonal stimules e.g. ACTH stimulates secretion of glucocorticoids in adrenal coretex B. The rate of metabolism Halftime in blood Peptides to 2-30 min. OXY, MSH Proteins 60 min. TSH Steroides 20 – 120 min. cortisol C. Hormone-binding-proteins – esp. steroids and catecholamines Hormone (active)+ blood proteins ↔ hormone-binding-protein (inactive) 1. Increased solubility 2. Increased halftime in blood D. Role of transport and degradation in pathology E. Recognition of hormones by target cells through specific receptors 1. Structure of receptors – proteins 2. Binding of hormones with high affinity 3. Concentration of hormone in target cells 4. Binding of a hormone causes a chain of reactions leading to a biology response 5. The interval between hormone binding and biology response is variable Type of hormone Binding-response interval neurotransmiters miliseconds peptides seconds-minutes proteins minutes-hours steroids hours-days 6. Number of receptors varies 7. Receptors are localised a. in the cell membrane on the surface b. in the nucleus of the target cells V. Methods of measurement A. Hormonal levels 1. bioassay 2. chemical analysis 3. radioimmunoassay B. Specific receptors C. Clearance VI. Endocrinopathy A. Hyposecretion – treated with hormone substitution B. Hypersecretion – treated: 1. surgical removal of the gland and hormone substitution 2. Radioactive destruction of the gland and hormone substitution 3. Hormonal antagonists C. Insensitivity or resistance of target organ – the most difficult treatment D. Ectopic tumors – no negative feedback mechanism HYPERTHYROIDISM AND HYPOTHYROIDISM 1. Brief recapitulation of synthesis and metabolism of thyroid hormones and their regulation 2. Brief recapitulation of thyroid hormones function 3. Syndromology of thyroid gland diseases and basics of diagnostics a. local syndrome b. dysfunction c. immunopathology PHARMACOLOGY Insulin - physiology, basal and stimulated secretion indications of insulin therapy tactics of insulin therapy (conventional, intensified) classification of insulin Peroral antidiabetic drugs - sulfonylureas – mechanism of action, main representatives, side effects - biguanides – mechanism of action, main representatives, side effects - inhibitors of intestinal glycosidase – mechanism of action, main representatives, side effects - thiazolidinediones (glitazones) – mechanism of action, main representatives, side effects - rapid insuline secretion stimulators – mechanism of action, main representatives, side effects Hormonal replacement therapy - effect on climacteric syndrome and long term risks - osteoprotective and cardioprotective effects of HRT - therapeutic regimens, active substances - indication, contraindication, side effects - selective estrogene receptors modulators (SERM) Antihormones - antiestrogenes – tamoxifen – mechanism of action, indication - mifepriston, aromatase inhibitors - antiandrogenes – types of, mechanism of action, indication Pharmacotherapy of osteoporosis - antiresorption drugs, HRT, bisphosphonates, calcitonin, SERM - mechanism of action, principles and risk of therapy Corticosteroids - types of, mechanism of action - substitution therapy - intensive short therapy, pulse therapy - long term and chronic therapy - indications and therapy strategy - side effect and contraindications Drugs used for treatment of obesity - drugs decreasing energy intake vs. drugs increasing energy expenditure - sibutramin, orlistat - mechanism of action - principles and risk of therapy