description of residency rotation (elective)
advertisement

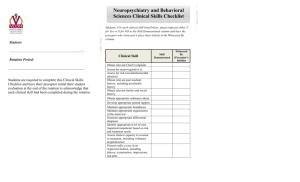
Psychiatry Rotation PHILADELPHIA VA MEDICAL CENTER Preceptor: Karimah Lynum, Pharm.D. PHONE NUMBERS Phone: 4038, 2598; (outside hospital: 215-823-4038); 6363 (Research) Pager: 215-894-1276 Pharmacy Administration Office: 5844 (outside hospital: 215-823-5844) Outpatient Pharmacy: 3534, 4408 (outside hospital: 215-823-6361) Inpatient, Mental Health: 6600 (7 West); 4107 (7 East) INSTITUTION Philadelphia VA Medical Center (PVAMC) provides health care for some 433,000 veterans living in America's fifth largest metropolitan area and surrounding seven counties. The PVAMC, the second largest VA medical center in Pennsylvania, is a VA acute referral center for the tri-state area and offers a wide range of advanced high tech treatments for the special needs of veterans. The facility is staffed by more than 1,500 employees and supports more than 150 acute beds and a 240-bed Nursing Home Care Unit.1 DESCRIPTION OF RESIDENCY ROTATION (ELECTIVE) The psychiatry rotation is designed to provide both an introduction and beginning level of concentration into the area of psychiatry. The resident will have the opportunity to provide pharmaceutical care in both the outpatient and inpatient setting for the mental health and behavioral health primary care services at PVAMC. The resident will participate in clinic services offered by the preceptor through the outpatient clinic, in addition to evaluating and observing patients with various mental disease states through clinical assessment and daily monitoring in the inpatient setting. The resident will interact daily with the preceptor and other healthcare practitioners in the outpatient/inpatient setting. KEY ROTATIONAL OBJECTIVES Upon completion of this rotation, the student will demonstrate the ability to: Monitor pharmacotherapy regimens for appropriate dosing adjustments, therapeutic duplications, drug-drug interactions, adverse events, polypharmacy, medications without indication etc. Independently gather patient data (medication history, physical findings, laboratory values, etc.) and assess therapy. Effectively communicate drug information requests with patients and healthcare providers Discuss the basic pathophysiology and pharmacotherapy of the following disease states/conditions discussed during the rotation, which include: Schizophrenia/Psychosis Depressive Disorders Bipolar Disorder Anxiety Disorders Sleep Disorders Substance Abuse Disorder Alzheimer's Disease and Dementia ORIENTATION The resident's orientation will include review of syllabus, including: rotation goals, objectives, evaluation process, assignments and responsibilities; introduction to the medical team and team members; orientation to the outpatient and inpatient clinic; introduction to key personnel (technicians, nurses, social workers, psychiatrists, psychologists, primary care team); and review of pertinent hospital and pharmacy policies and procedures. The preceptor will ensure the completion of CPRS Training prior to beginning rotational activities. Last Updated 1/26/12 1 EDUCATIONAL OBJECTIVES and COMPETENCIES R1.5 Provide concise, applicable, comprehensive, and timely responses to requests for drug information from patients and health care providers. R2.1 As appropriate, establish collaborative professional relationships with members of the health care team R2.2 Place practice priority on the delivery of patient-center care to patients. R2.3 As appropriate, establish collaborative professional pharmacist-patient relationships. R2.4 Collect and analyze patient information. R2.5 When necessary, make and follow up on patient referrals R2.6 Design evidence-based therapeutic regimens R2.7 Design evidence-based monitoring plans. R2.8 Recommend or communicate regimens and monitoring plans. R2.9 Implement regimens and monitoring plans. R2.10 Evaluate patients' progress and redesign regimens and monitoring plans. R2.12 Document direct patient care activities appropriately. R5.1 Provide effective medication and practice-related education, training, or counseling R6.1 Use information technology to make decisions and reduce error. E7.2 Communicate effectively E7.4 Manage time effectively to fulfill practice responsibilities. PRE-REQUISTE LEARNING The resident should obtain access to at least 3 different sources listed in the Available References section of syllabus. The resident should be familiar with basic patient interview techniques as well as basic pathophysiology and drug therapy of the above listed disease/disorder states. The resident should be familiar with normal laboratory values, especially those associated with metabolic syndrome, the "SOAP" format, and creatinine clearance determinations. CLERKSHIP ACTIVITIES AND ASSIGNMENTS OUTPATIENT ACTIVITIES: MHC PHARMACY MEDICATION MONITORING CLINIC o Interview patient referred by mental health for metabolic syndrome monitoring o Evaluate current stages of patient and necessity for monitoring o Develop plan/monitoring parameters, etc. o Document via CPRS progress note CLOZARIL® CLINIC (Weekly) MOOD DISORDER CLINIC (Consult Service) MHC PHARMACY-WALKIN (Daily) SPECIAL PROJECTS INPATIENT ACTIVITIES: Participate in interdisciplinary team meetings, Tuesday, Wednesday, and Thursday mornings. Participate in daily monitoring and clinical assessment of patients within the designated patient case load (3) with the following required activities: o Review medications and pertinent laboratory data o Address appropriate interventions with preceptor o Leave intervention notes for physicians with clinical recommendations that are co-signed by the preceptor o Follow-up on previous days' interventions o Reconcile Medication Administration Record upon admission, during stay, and at time of discharge. o Participate in discharge medication counseling and order processing. o Note Patient Case Load Requirements: Designate at least 4 initial patient cases to follow by the 2nd day of the rotation start on inpatient. Last Updated 1/26/12 2 The resident and preceptor will discuss the cases to ensure a variety and multiple educational opportunities are present, as determined by the preceptor and resident. The resident is to maintain at least 3 patient cases at any one time. GENERAL ACTIVITIES: Attend and participate in Outpatient and Clinical Staff Pharmacy Meetings Present announcements/topics to Mental Health Clinic during staff meetings Provide drug information to Mental Health Clinic/Behavioral Health Primary Care Team Respond to Drug Information requests within 3 days Meet with preceptor for topic discussions/journal reviews Attend staff meetings for MHICM team GENERAL ASSIGNMENTS: Prepare for topic discussions assigned by preceptor by reviewing current literature Evaluate current medical literature and present one journal club per month to pharmacy department staff and students Present one patient case presentation per week to preceptor Present pharmacy in-service to nursing staff and/or pharmacy staff Drug Class Reviews REQUIRED READINGS: STAR*D trial CATIE antipsychotic trial Ciranni MA, Kearney TE, Olson KR. Comparing Acute Toxicity of First- and SecondGeneration Antipsychotic Drugs: A 10-Year, Retrospective Cohort Study. J Clin Psychiatry 70:1, January 2009 Boyer EW and Shannon M. The Serotonin Syndrome. New Engl J Med 2005;352:1112-20 Blanchet PJ. Antipsychotic Drug-Induced Movement Disorders. Can J Neurol Sci 2003; 30: suppl 1:S101-7. Cutler, AJ, Kalali AH, Weiden PJ, et al. Four-Week, Double-Blind, Placebo- and ZiprasidoneControlled Trial of Iloperidone in Patients With Acute Exacerbations of Schizophrenia. Journal of Clinical Psychopharmacology; Volume 28:2, Supplement 1, April 2008 Dipiro Pharmacotherapy and Mental Health chapters “Drug Therapy: Alzheimer’s Disease” N England J Med Vol 351(1), July 2004. Pages 56-67. Lieberman JA, Stroup TS, McEvoy JP, Swartz MS, et al. Effectiveness of Antipsychotic Drugs in Patients with Chronic Schizophrenia. N Engl J Med 353;12, September 22, 2005 AVAILABLE REFERENCES: Clinical Psychopharmacology made Ridiculously Simple, 4th Ed. J. Preston and J. Johnson DSM-IV TR Essential Psychopharmacology, 2nd Ed. Stephen Stahl Child and Adolescent Clinical Psychopharmacology Made Simple, J. Preston, J O’Neal, and M. Talaga ASHP Therapeutic Position Statement of the Use of Second-Generation Antipsychotic Medications in the Treatment of Adults with Psychotic Disorders. August 4, 2004. Diverse Roles of Anticonvulsants in Bipolar Disorders. Annals of Clin Psyc Vol 15(2) June 2003, pp95-108. Consensus Development Conference on Antipsychotic Drugs and Obesity and Diabetes (2004). Thase ME, Howland RH, Friedman ES. Treating Antidepressant Nonresponders With Augmentation Strategies: An Overview. J Clin Psychiatry 1998;59[suppl 5]: 5-12. Last Updated 1/26/12 3 Inouye SK. Delirium in Older Persons. N Engl J Med 2006;354:1157-65. Fick DM, et al. Updating the Beers Criteria for Potentially Inappropriate Medication Use in Older Adults. Arch Inter Med 2003;163:2716-2724. ASHP Therapeutic Position Statement on the Use of Second-Generation Antipsychotic Medications in the Treatment of Adults with Psychotic Disorders (Jason Noel2007). EVALUATION Based upon the following: Attendance, attitude, and professionalism Motivation to achieve independent competence Demonstration of disease state knowledge and application to clinical practice Participation in topic discussions Nursing/Pharmacy In-service Final Examination (At the discretion of the preceptor) Formal Journal Club Case Presentation (4) Drug Review (4) A midpoint evaluation will assess progress and provide suggestions for improvement. TARDIES AND ABSENCES ALL tardies or absences MUST be called in directly to the preceptor. Tardies and absences will be handled accordingly: For each tardy resident will be required to makeup the time For each unexcused absence, the resident will be required to makeup the time with an additional project at the discretion of the preceptor. JOURNAL CLUB GUIDELINES Article selection The topic should be psychiatry related The topic should be one that the resident has not discussed previously Selection of article must be from a peer-reviewed medical journal Article should have been published within the past 6 months Article and handout will be provided to the preceptor 2 days prior to presentation Format Presentation should be 20 minutes long and 2-3 minutes for questions/discussion Introduction Title, authors, journal and date A brief introduction to subject Review of article Methods should include study design; inclusion/exclusion criteria Results Author’s conclusion Your conclusions Discuss strengths and weaknesses of the study Discuss application to clinical practice Last Updated 1/26/12 4 CASE PRESENTATION GUIDELINES CASE SELECTION The topic should be one that the resident has not discussed previously. Presentation should be no longer 15-20 minutes including time for questions FORMAT Introduction Vital statistics on admission Chief complaint, history of present illness Past Medical History, allergies Medications prior to admission Social/family history Pertinent physical exam, vitals, labs Problem list Abbreviated summary of hospital course (labs, tests and drug changes) Review of topic Background Focus mainly on drug therapy Conclusions Please relate topic to patient at the end Be prepared to comment on any discrepancies with the care of the patient Handout Maximum of 4 pages Provide a list of references (at least 2 have to be primary literature) Presentation should be an outline, not a transcript Refer to medications by generic names only Last Updated 1/26/12 5