Precepting Webinar Q and A
advertisement
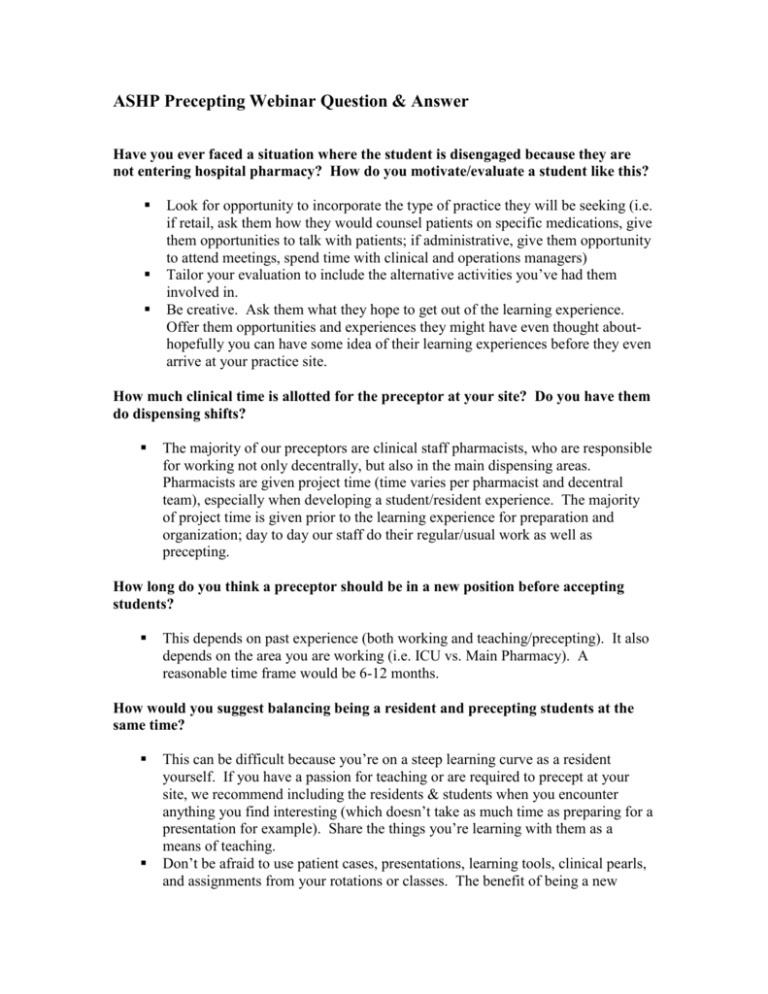
ASHP Precepting Webinar Question & Answer Have you ever faced a situation where the student is disengaged because they are not entering hospital pharmacy? How do you motivate/evaluate a student like this? Look for opportunity to incorporate the type of practice they will be seeking (i.e. if retail, ask them how they would counsel patients on specific medications, give them opportunities to talk with patients; if administrative, give them opportunity to attend meetings, spend time with clinical and operations managers) Tailor your evaluation to include the alternative activities you’ve had them involved in. Be creative. Ask them what they hope to get out of the learning experience. Offer them opportunities and experiences they might have even thought abouthopefully you can have some idea of their learning experiences before they even arrive at your practice site. How much clinical time is allotted for the preceptor at your site? Do you have them do dispensing shifts? The majority of our preceptors are clinical staff pharmacists, who are responsible for working not only decentrally, but also in the main dispensing areas. Pharmacists are given project time (time varies per pharmacist and decentral team), especially when developing a student/resident experience. The majority of project time is given prior to the learning experience for preparation and organization; day to day our staff do their regular/usual work as well as precepting. How long do you think a preceptor should be in a new position before accepting students? This depends on past experience (both working and teaching/precepting). It also depends on the area you are working (i.e. ICU vs. Main Pharmacy). A reasonable time frame would be 6-12 months. How would you suggest balancing being a resident and precepting students at the same time? This can be difficult because you’re on a steep learning curve as a resident yourself. If you have a passion for teaching or are required to precept at your site, we recommend including the residents & students when you encounter anything you find interesting (which doesn’t take as much time as preparing for a presentation for example). Share the things you’re learning with them as a means of teaching. Don’t be afraid to use patient cases, presentations, learning tools, clinical pearls, and assignments from your rotations or classes. The benefit of being a new practitioner is that resources from your learning experiences should be current and need little to no work to update. Residents often have more to offer than they sometimes realize. I will have students who are interested in residencies meet with the residents to discuss the residency application process. As a preceptor, it’s important to put residents in teaching situations where they’re going to be comfortable and build some confidence in teaching and/or giving advice. Depending on the resident, it may be appropriate to wait until the last ½ or 1/3 of the residency to dedicate to teaching. Approximately how much time per day do you recommend spending with your student? Depends on the day. Some days zero hours (because they are with another staff member or because of scheduling) and sometimes 1-2 hours. The key is to try and be consistent; whether it’s 2 hours/week or 5 hours/week. Establishing a communication mechanism is vital (email, website, phone,etc…) It also depends on the level of interaction. They may be working side-by-side with a preceptor all day with easy access for questions as they come up, but may only total to a few hours of interaction. It is reasonable to aim for 1 – 2 hours per day of direct interaction with cases, teaching points, etc. But this needs to be flexible and would be site specific. How would you recommend handling a student who relies heavily on their drug information resources in their PDA and cannot think on their feet? This is tough, because it’s certainly reasonable to look up questions in a reference; but you could simply ask them to share with you their thoughts before checking the reference; ask them pointed questions about their thought process, try to get them to critically think through the important points and assess the situation before reaching for a reference. We recommend helping them understand that being a pharmacist is not all about knowing just drug facts. It is reasonable to look things up, especially when you are new to an area and are fielding many unfamiliar questions. With experience, a student begins to see the same types of issues surface and can begin to anticipate certain drug therapy problems, for instance. That’s where the ‘thinking on your feet’ becomes much easier. The trick for a preceptor is to make them aware of common vs. unexpected questions and to nurture that anticipation skill that will help them develop a thought process more quickly. Certainly no easy feat. It also depends on what they are looking up. Specific drug doses seem more reasonable than which drugs should be used; also it is better to encourage them to double-check rather than guess and be wrong. In general, how long do you recommend before a resident should be ready to coprecept students? Depends on the resident and where they are in their residency year. As a resident I was expected to co-precept from the beginning. But I often felt that the students may have found it more beneficial if I was more well established and familiar with the residency/site. Perhaps 3-6 months is reasonable before having the resident co-precept. Residents may be able to participate with parts of the student’s learning experience earlier on. For instance, I attended the students’ case presentations and journal clubs right away and also led 1 – 2 topic discussions with them. Allowing 3 – 6 months to get settled in is best before evaluating and more formally precepting students.