Blood lab answers
advertisement

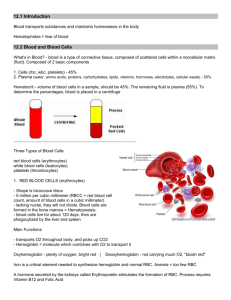
Anatomy and Physiology I Lab: Blood Blood is the fluid that circulates through the heart, arteries, capillaries and veins and that constitutes the chief means of transport within the body. Blood is a _liquid_connective __ tissue. A) Three General Functions of Blood: 1. _Transportation______ The blood transports: - _oxygen____________ from the lungs to the cells of the body - _CO2_________ from body cells to the lungs - _nutrients_____________ from GI tract to body cells - _hormones____________ from endocrine cells to other body cells - _heat_________ and _waste_________ products to lungs, kidneys and skin for elimination 2. _Regulation___________________ Circulating blood helps maintain homeostasis in all body fluids. The blood helps: - __regulate pH_____________ through buffers - adjust body __temperature_____________ - influence __H2O________ content of cells 3. _Protection_______________________ The blood: - protects against its _excessive loss__ after and injury via _clotting___ - protects against _disease____________ via – a. phagocytic white blood cells b. blood proteins (antibodies and interferons) B) Major Components of Blood 1. Components a) _blood plasma_______________ - a watery liquid matrix that contains dissolved substances b) formed elements = _cell and cell fragments_____ i) _red blood cells__________ (erythrocytes) (RBC) ii) _white blood cells________ (leukocytes) (WBC) iii) _platelets_________________ 2. Total Blood Volume of RBC, WBC and platelets and plasma Complete the labels below. a) _plasma_______________55% b) _cells_______________45% 99% RBCs less than 1% WBCs and platelets 3. Plasma – Composition a) _water____________ (91.5%) - liquid portion of blood - acts as a solvent and suspending medium - absorbs, transports, releases heat. b) _proteins____________ (7%) - those confined to blood stream = _plasma proteins_______ - help maintain proper blood osmotic pressure 3 main plasma proteins 1. _albumin_______ – transport hormones and fatty acids 2. _globulins_______– transport iron, lipids, vitamins immunoglobulins (antibodies) - help attack _viruses and bacteria____ 3. _fibrinogen_____ – role in blood clotting c) _other solutes________ (1.5-2%) - electrolytes, nutrients, hormones, gases, wastes 4. __Red Blood Cells_______________ (Erythrocytes) a) Structure RBCs : are biconcave _discs_________ which provides a _large surface area____ for diffusion of gas molecules in and out of RBC have a __strong flexible plasma membrane____________which allows RBC to squeeze through narrow capillaries without being damaged have no _nuclei_____ or _organelles________ therefore all internal space is available for _O2______ transport and they do not undergo cell division - contain protein called _hemoglobin_______________ that carries O2 gives blood its red colour b) What is the normal RBC count: male- 5.4 million/drop female- 4.8 million/drop c) Hemoglobin (Can carry _4___ oxygen molecules from lungs to tissue cells.) Consists of: i) a _globin_________ protein consisting of 4 polypeptide chains ii) 4 _heme groups____________ - one heme group is attached to each polypeptide chain - each heme group contains a _iron ion (Fe2+)___hat can combine reversibly with one oxygen molecule -1/3 of cells weight is hemoglobin d) Hematocrit = _% of total blood volume occupied by RBC_____ - female normal range = __38-46% (avg.42%)____________ = 42% of blood volume composed of RBCs - male normal range = _40-55% (47%avg.)__________ (higher since testosterone in males) i) A higher than normal hemocrit = _anemia____________ ii) A lower than normal hemocrit = __polyethemia_______ e) Blood doping: What is blood doping? -injecting previously stored RBC’s before an athletic event i. ii. Why do athletes do it? -more cells available to deliver oxygen to tissues iii. Is it dangerous and if so why? -yes- increases blood viscosity -forces heart to work harder C) Transport of O2 and CO2 by RBCs a) Briefly describe the transport of O2 and CO2 by RBCs. Each hemoglobin molecule picks up 4 O2 molecules from the lungs Each O2 is bound to the iron of the heme group As blood flows through the capillaries the iron-oxygen reaction reverses. Hemoglobin releases O2 which diffuses into the interstitial fluid and then into the cells. Blood flows through tissue capillaries picking up CO2 which combines with AAs in the globin part of the hemoglobin. As blood flows through the lungs CO2 is released from the hemoglobin and then exhaled. b) What does the hemoglobin transport that helps to regulate blood pressure? -transports nitric oxide and super nitric oxide helping to regulate BP c) Nitric oxide causing _vasoconstriction_________-is released in the lungs d) Super nitric oxide causing _vasodilation________-is picked up in the lungs D) White Blood Cells (Leukocytes) White blood cells have a _nucleus____and does not contain _hemoglobin____. Granular or agranular classification based on presence of cytoplasmic granules made visible by staining Complete the chart below to name and describe the 5 types of leukocytes. Type of Leukocyte Function neutrophil -phagocytosis – destruction of bacteria -60-70% of circulating WBCs -fastest WBC getting to tissue -granular destruction due to bacteria -diameter is 10-12 microns basophil -less than 1% of circulation WBCs -granular -diameter is 10-12 microns -involved in allergic reactions – intensifies the overall inflammatory response (liberates histamine) -heighten inflammatory response eosinophil -2-4% of circulation WBCs -granular -diameter is 10-12 microns -combat the effects of histamine in allergic reactions - phagocytosis -slows down inflammation caused by basophils monocyte -3-8% of circulating WBCs -agranular -largest WBC in circulation – diameter is 12-20 microns -phagocytosis -takes longer to get there, but come in larger numbers and destroy more microbes -clean up dead tissues following an infection B cells- destroy bacteria and inactivate their toxins- develop into plasma cells, which produce antibodies lymphocyte -20-25% of circulation WBCs -increase in # during viral infections -agranular -small cells 6-9 microns in diameter -large cells 10-14 microns in diameter T cells- attack invading viruses, cancer cells, and transplanted tissue cells(doesn’t recognize the cells) Natural killer cells- attack a wide variety of infectious microbes and certain spontaneously arising tumor cells Emigration and Phagocytosis in WBCs a) How does WBC get between cells? -WBC roll along endothelium, stick to it & squeeze between cells b) How do selectins help with emigration -help WBCs stick to endothelium, displayed near site of injury c) What role do neutrophils (integrins that are found on neutrophils) play in emigration? -assist in movement through wall d) Neutrophils and macrophages(derived from monocytes) _phagocytize__bacteria. E) Platelets – Hemostasis – a sequence of responses that stops bleeding a) Structure -disc shaped cell _fragments_____ with no _nucleus__________ b) Function i) _help stop blood loss from damaged blood vessels by forming a platelet plug ii)_granules of platelets contain substances that promote blood clotting c) What is vascular spasm? -damage to blood vessel stimulates pain receptors -reflex contraction of smooth muscle of small blood vessels d) What are the steps in order for platelet plug formation briefly explain each step: (page 647) 1.__platelet adhesion___________- platelets stick to exposed collagen( damaged blood vessels) underlying damaged endothelial cells in vessels wall 2.__platelet release reaction______- adhesion causes platelets to become active – extend projections to make contact and interact with each other – liberate contents in vesicles activating nearby platelets which in turn function as vasoconstrictors, causing contraction of vascular smooth muscle, which decreases blood flow through the injured vessel 3.__platelet aggregation_________- vesicle contents makes other platelets (new recruits) in the area sticky – cause platelets to adhere to originally activated platelets causing a gathering of platelets (aggregation), the accumulation and attachment of large numbers of platelets form a mass called a platelet plug (platelet plug becomes tight when reinforced by fibrin threads formed during clotting) – edges of damaged vessel are pulled together Blood clotting – through a sequence of events enzyme thrombin converts fibrinogen to fibrin that forms the threads of the clot e) What is the role of Vitamin K in Clotting? -required for the synthesis of clotting factors f) Intravascular clotting: i. What is a thrombosis? -clot (thrombus) forming in an unbroken blood vessel ii. What is an embolus? -clot, air bubble or fat from broken bone in the blood – pulmonary embolus is found in lungs iii. What can help to reduce inappropriate clot formation? -low dose aspirin reduces inappropriate clot formation iv. What are some diseases caused by these inappropriate clots? -strokes, TIA (transient ischemic attacks), and myocardial infarctions F) ABO Blood Groups a) Define: i) Antigen = a molecule typically found in the surface of a cell whose shape triggers the prod’n of Abs that will bind to the molecule ii) Antibody = a protein molecule produced by the immune system that recognizes a particular foreign antigen and binds to it b) The ABO blood groups are based on two glycolipid antigens called _A__ and _B___found on RBCs. c) - People whose RBC have only antigen A have type __A____blood. - People whose RBC have only antigen B have type __B____ blood. - People whose RBC have both antigen A and antigen B have type _AB_____ blood. - People whose RBC have neither antigen A nor antigen B have type _O_______ blood. d) Blood plasma usually contains antibodies (agglutinins) to the above antigens. i) Anti-A Antibody reacts with __antigen A__________ ii) Anti-B Antibody reacts with __antigen B__________ e) A person’s blood only has antibodies for the antigens that their RBCs lack. ie. Type A blood = antigen A on RBC = anti – B Ab in plasma f) Complete the table below Antigen on RBC A Blood Type B B Antibody in plasma Anti – B Compatible Donor/s A, O A AB A and B O Neither A nor B Anti - A Neither Anti A nor anti-B Both anti-A and anti-B B, O A, B, AB, O O g) Which blood type is the universal recipient? Explain. -AB is universal recipient -can receive blood of any of 4 ABO types since plasma has no antiA Abs or anti-B Abs h) Which blood type is the universal donor? Explain. -O is the universal donor -can donate blood to any of the 4 ABO types since RBC have neither A nor B antigens i) What would happen if a person with type B blood received a transfusion of type A blood? Explain. - donated RBC would hemolyze (burst) = release haemoglobin = = kidney damage - Recipient’s type B blood has B antigens on RBC and anti-A Ab in plasma - Donor’s type A blood has A antigens on RBC and anti-B Ab in plasma 1. recipient’s anti-A Abs in plasma bind to A antigens on donor RBC = hemolysis of donor RBC = kidney damage 2. donor’s anti-B Abs in plasma bind to antigen B on recipient’s RBC = hemolysis of recipient RBC (but anti-B Ab are usually so diluted in recipient plasma that significant hemolysis does not occur) G) Rh Blood Group a) b) c) d) e) People whose RBC have Rh antigens are designated _Rh+_____ People whose RBC _lack Rh antigens______ are designated RhNormally the blood plasma does not contain anti-Rh antibodies. Antibodies only develop in what blood type Rh- or Rh+ circle correct answer. How do they develop? And give examples! -antibodies develop only in Rh- blood type and only with exposure to the antigen -transfusion of positive blood -during a pregnancy with a positive blood type fetus f) When a transfusion reaction occurs upon 2nd exposure to the antigen what condition occurs? -Rh- person receives Rh+ blood = recipient’s immune system makes anti-Rh+ Abs that remain in the blood -If a 2nd transfusion of Rh+ blood is given the anti-Rh+ Abs will bind to the donated RBC = hemolysis of donated Rh+ RBC g) Describe the role of Rh incompatibility in hemolytic disease of the newborn (HDN). Rh- mother Rh+ fetus - at birth a small amount of Rh+ fetal blood enters maternal bloodstream - mother’s immune system creates anti-Rh+ Abs which remain in blood - 2nd Rh+ fetus i. maternal anti-Rh+ Ab cross placenta ii. anti-Rh+ Ab bind to fetal Rh+ RBC = hemolysis Prevention: - Rh- mothers receive an injection of anti-Rh+ Ab after delivery - anti-Rh+ Abs bind to any Rh+ RBC in maternal bloodstream - mother’s immune system does not make any anti-Rh+ Abs