Transcript of interview with Fiona Stanley
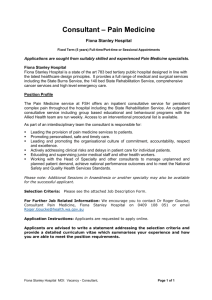
advertisement

Transcript of interview with Professor Fiona Stanley Voice-over: Welcome to the National Health and Medical Research Council podcast. Our podcasts aim to keep you in touch with major health and medical research issues, and the people who shape them. Introduction: Two of Fiona Stanley's most significant discoveries are that if a mother has a diet rich in folic acid it can prevent spina bifida in babies, and that cerebral palsy is not only the result of birth trauma, but may also be caused by other factors such as infections. Former Australian of the year, Professor Fiona Stanley is the founding director of the Telethon Institute for Child Health Research. As well as being a living national Treasure, Fiona is a professor in the school of paediatrics and child health at the University of Western Australia, and UNICEF’s Australian Ambassador for Early Childhood Development. In this conversation with Dr Mark Bradley, she explains how the Telethon Institute evolved into a highly regarded organisation which she calls a hotchpotch of science trying to make a difference. Interviewer: Fiona, thanks very much for joining us today on this National Health and Medical Research Council podcast, a bit of a pioneering podcast in the series, because this one's being done over Skype. But welcome. Prof. Stanley: Thank you very much. Interviewer: I thought we might begin by you giving us an overview of this wonderful institute, the Telethon Institute for Child Health Research. You've done some terrific work over the years. Prof. Stanley: Yes. Well, the interesting thing about the institute is that we really established it because I had come out of a - every 10 years I seem to have a frustration in my career. After the first 10 years of clinical work I realised that I wasn't going to make it as a clinician and that I really wanted to get into epidemiology and preventive medicine. So for 10 years I was in an NHMRC-funded unit in epidemiology and preventive medicine. After 10 years of that, I thought, 'Uh-huh, epidemiology alone can't unpack the complex causal pathways to child health problems. We need a multidisciplinary institute that is able to go from what's happening in genes and cells and molecules to the whole child and then to the child in its family and its community, so right through to the population sciences, and they all need to be together in one building and they all need to interact and work together in a lovely collaboration which will really start to understand cause and prevention,' and that was the dream of the institute. Of course, when you set up an institute in a remote place like Perth, a lot of what you do is opportunistic rather than strategic. So in the first 10 years or so, we were opportunistic, and we were luckily so. In other words, whilst the people that I managed to recruit in the institute were nearby, and therefore achieving - that we could actually get them in here - they were the right kinds of people. So we had the immunology research group at the Children's Hospital, who were basically mucosal immunologists, looking at what would happen to the developing respiratory tree; they've unpacked the asthma epidemic, which has just been fantastic, and have moved from about 80 per cent of their work being in animal models now to about 80 per cent of their work 1 being in the human model, including our big cohort studies that we do here in Western Australia. There was a group around - and that's the group around Pat Holt and Wayne Thomas. Then there's another group around childhood leukaemias and cancers, including solid tumours, around Ursula Kees. She was also in the immunology research unit. She's expanded dramatically and has built upon growing these tumours, both leukaemias and spotted tumours up as cell lines, which now go all over the world, and to look at both the genetic and immunological aspects of cancer. We've linked that into the population sciences, where we have a big group now working in childhood cancers, the genealogy of childhood cancers. So those two groups in basic science moved their mostly immunogenetic basic science research into the institute, and we've expanded that just recently by recruiting Jenny Blackwall from Cambridge. She is really a molecular parasitologist, looking at the sort of genetic aspects of infectious disease. And we also have Pru Hart now who heads up an inflammation laboratory particularly looking at skin. And then we recruited from Melbourne a top clinical researcher, Peter Sly, whose responsibility it was to work in mainly respiratory disease, but to build up clinical research in the institute. And then, of course, my group expanded dramatically from just a fairly narrow immunological maternal and child health group and focusing a lot on peri-natal epidemiology - things like low birth weight, birth defects, cerebral palsies, neurodevelopmental disorders. It's expanded enormously into psycho-social pathways, suicide prevention, mental health, Aboriginal child health, infectious disease, and a much expanded developmental disorders research endeavour. So the plan of the institute was to try and say well, okay, we've got these major different groups the basic scientists, you know, including geneticists and info-biomathematicians and so on, the clinical scientists and the population scientists, but what we want to do is have big important themes going across the entity. So asthma allergy is one theme, cancer is another theme, infectious disease is another theme, Aboriginal child health another theme, mental health and developmental disorders, and actually sort of child health and development normal pathways into child health and development, and the whole idea was to have basic clinical and population sciences represented in all those themes. That's not happened yet, 17 years down the track, but it has happened a lot more than you would think. So this idea of having true collaboration across disciplines has been fantastic, particularly in asthma allergy, particularly in the cancer, particularly in some of the infectious disease program, less so in things like Aboriginal health, mental health and developmental disorders. We don't have a basic science underpinning for those, and I think we'd have to make a major investment and recruit some top people to make that an effective collaboration. The other big thing that the institute does is not just sit around and publish and try and publish in the best journals and hope that it gets picked up. What we do is have a big translational capacity. So a lot of my time and the time of some of the people in all of the different groups, but particularly in the clinical and in the population sciences, is about influencing policy or clinical practice or population health practice, which has been incredibly successful, but also the basic sciences had a very big success rate in terms of commercialisation. So we've now got several companies - and many, many patents - that the institute has produced. So I guess it's a wonderful hotch-potch of, you know, science trying to make a difference, focusing mostly on children and young people, but expanding a lot now beyond health even to take on board education, child abuse and neglect, and juvenile justice issues as well. So it's a pretty exciting place to be in. 2 Interviewer: You mentioned that you'd had some commercialisation outcomes, which is always good to hear from a research institute like yours, which has such breadth of activity. You were talking before about the leukaemia and cancer research. I know that one of those spinout companies, called Phylogica, came out of your institute, and it's now listed, I believe, on the Australian Stock Exchange? Prof. Stanley: That's right, yes. Interviewer: Has that been the most significant commercial outcome from the institute, or do you have a steady stream of activity? Prof. Stanley: We've had a pretty good stream of activity, but it's been the one we've gone farthest with, as it were, and following out of Phylogica's success, we've now got a drug discovery lab in the institute, which has basically got mostly Phylogica people in it. But there's been a really good - we've had a very good relationship with big pharma, some of which has just been, 'Here's the money. We're interested in anything you produce.' That's a very good relation that Pat Holt has had with GlaxoSmithKline. We've had a lot of funding from the big pharmaceutical companies that make vaccines - we've had about, oh, probably 80 vaccine trials since the 1990s, where we've done everything from the evaluation of new vaccines to looking at whether the vaccines can be given together, to look at novel ways of delivery of vaccine. We're doing trials on HPV as well as bird flu - you know, it's huge. Peter Richmond heads up a lot of that, but we always try to add some scientific questions to our vaccine trials. Wayne Thomas has had some very successful allergy patents - in fact, the first royalty cheque, of a very small amount, was Wayne's, which came into the institute some years ago, and that was with ALK and the patent has since been sold on. So that's really for the treatment of people with allergy, because we have so many allergens that have been purified and can be used, not just house dust mite, but others. And the other area has been in - Peter Sly and his team have developed novel ways of assessing infant lung function, because you can't say to a six-month-old, 'Take a nice big breath and then breathe out.' So he's got this very special mechanism of measuring lung function. And Paul Watt, who actually started Phylogica, the anti-inflammatory protein that - the molecule that we've got, he also developed a very nifty little spinhaler to enhance delivery of treatments for both asthma and pneumonia for kids, young kids, to make it sort of easy for them to take their medication. But Phylogica has been our most successful commercialisation, because it's really gone into a company and something the institute has had a very much greater role in, and Bruce McHarrie, who is our chief financial officer, as well as Paul, the director of Phylogica, have to take a lot of the credit for that and we're very proud that it's done it, because we do want to have - we want all of our - we want to have our institute successful in all areas of endeavour. Many people think because we're such advocates for Aboriginal health and for social justice and for child development, people forget that we also have this commercial success, which I'm very proud of. Interviewer: No, it's been terrific. I think there's a lot of institutes that could learn from your model. A final question - if you had to give advice, which I'm sure you do regularly to a young either high school student or researcher, an undergraduate student, and they're sort of toying with the idea of whether they should go into medical research or into scientific research, what would your key piece of advice be to try to ensure they do follow that path? 3 Prof. Stanley: I think that basically they probably can see how much fun I have and what an incredibly exciting career health and medical research can be. I think one of the things that's really very satisfying about it is to a certain extent you control your own agenda, and therefore you have the power to influence what you want to do better than almost any other career I can think of - you're the ones who are initiating the research, you're the ones who are writing the grants. Okay, it might be tough. You're never going to be a millionaire unless you go along the commercialisation route and hit it big time. But you're going to have this immense satisfaction of working with groups of people who are similarly committed, exciting people. You think of some of the characters in health and medical research. I mean, they're absolutely gorgeous, and lots of fun. And I get a sense that these people love working in this institute. There's a sense of great camaraderie and we have a lot of fun together. I think that people can actually see it has the potential to make a lot of difference to many of the problems in society which are actually not getting better. I think that there's almost, you know, five major big issues in the area of children and young people, which research is just important that we do - in mental health and in pathways into chronic disease and exposures in pregnancy and how they might, all the epigenetic stuff we were talking about. There are so many exciting problems for people to get stuck into. And what's more exciting now than it was in my day when I was making these decisions is the technology and the capacity that we have now to look at brain function, to look at what's happening in various systems in the body - structural biology, in the gene. It is just so much more - if I was going to start again, I'd do something like neuroembryology - I mean, some of the stuff we're going to be able to unpack is going to be so exciting in the future. I would just say to you if you want the most exciting career ever you could choose, this is for you. Interviewer: Fiona, that's a terrific advertisement. Again, thank you very much for your musings - they've been mighty. And I wish you all the best. Prof. Stanley: Thank you. Voice-over: This podcast was brought to you by the National Health and Medical Research Council, working to build a healthy Australia. You’ll find more information about this and other health and medical research issues on our website, at www.nhmrc.gov.au. 4