CH 9 Outline
advertisement

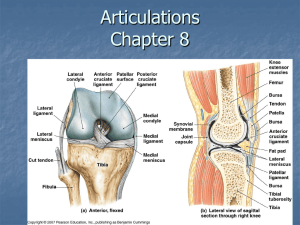
Chapter 9 Articulations Introduction Articulation—point of contact between bones Joints are mostly very movable, but others are immovable or allow only limited motion Movable joints allow complex, highly coordinated, and purposeful movements to be executed Classification of Joints Joints may be classified using a structural or functional scheme (Table 9-1) Structural classification—joints are named according to one of the following: • Type of connective tissue that joins bones together (fibrous or cartilaginous joints) • Presence of a fluid-filled joint capsule (synovial joint) Functional classification—joints are named according to degree of movement allowed: • Synarthroses—immovable joint • Amphiarthroses—slightly movable • Diarthroses—freely movable Fibrous joints (synarthroses)—bones of joints fit together closely, allowing little or no movement (Figure 9-1) Syndesmoses—joints in which ligaments connect two bones Sutures—found only in skull; toothlike projections from adjacent bones interlock with each other Gomphoses—between root of a tooth and the alveolar process of the mandible or maxilla Cartilaginous joints (amphiarthroses)—bones of joints are joined together by hyaline cartilage or fibrocartilage; allow very little motion (Figure 9-2) Synchondroses—hyaline cartilage present between articulating bones (ribs) Symphyses—joints in which a pad or disk of fibrocartilage connects two bones (symphysis pubis) Synovial joints (diarthroses)—freely movable joints (Figure 9-3) Structures of synovial joints • Joint capsule—sleevelike casing around ends of bones, binding them together • Synovial membrane—lines joint capsule and also secretes synovial fluid • Articular cartilage—hyaline cartilage covering articular surfaces of bones Classification of Joints Structures of synovial joints (cont.) • Joint cavity—small space between the articulating surfaces of the two bones of the joint • Menisci (articular disks)—pads of fibrocartilage located between articulating bones • Ligaments—strong cords of dense, white, fibrous tissue that hold bones of synovial joint more firmly together • Bursae—synovial membranes filled with synovial fluid; cushion joints and facilitate movement of tendons Types of synovial joints (Figure 9-4) • Uniaxial joints—synovial joints that permit movement around only one axis and in only one plane Hinge joints—articulating ends of bones form a hinge-shaped unity that allows only flexion and extension Pivot joints—a projection of one bone articulates with a ring or notch of another bone • Biaxial joints—synovial joints that permit movements around two perpendicular axes in two perpendicular planes Saddle joints—synovial joints in which the articulating ends of the bones resemble reciprocally shaped miniature saddles; only occurrence in body is in thumbs Condyloid (ellipsoidal) joints—synovial joints in which a condyle fits into an elliptical socket • Multiaxial joints—synovial joints that permit movements around three or more axes in three or more planes Ball and socket (spheroid) joints—most movable joints; ball-shaped head of one bone fits into a concave depression Gliding joints—relatively flat articulating surfaces that allow limited gliding movements along various axes Representative Synovial Joints Humeroscapular joint (Figure 9-5) Shoulder joint Most mobile joint because of the shallowness of the glenoid cavity Glenoid labrum—narrow rim of fibrocartilage around glenoid cavity that lends depth to the cavity Structures that strengthen the shoulder joint are ligaments, muscles, tendons, and bursae Representative Synovial Joints Elbow joint (Figure 9-6) Humeroradial joint—lateral articulation of capitulum of humerus with head of radius Humeroulnar joint—medial articulation of trochlea of humerus with trochlear notch of ulna Both components of elbow joint surrounded by single joint capsule and stabilized by collateral ligaments Classic hinge joint Medial and lateral epicondyles are externally palpable bony landmarks Olecranon bursa independent of elbow joint space—inflammation called olecranon bursitis • Trauma to nerve results in unpleasant sensations in those fingers and part of hand supplied by nerve; severe injury may cause “wrist drop” Proximal radioulnar joint—between head of radius and medial notch of ulna Stabilized by annular ligament Permits rotation of forearm Dislocation of radial head called “pulled elbow” Distal radioulnar joint—point of articulation between ulnar notch of radius and head of ulna Together with proximal radioulnar joint, permits pronation and supination of forearm Radiocarpal (wrist) joints (Figure 9-7) Only radius articulates directly with carpal bones distally (scaphoid and lunate) Joints are synovial Scaphoid bone is fractured frequently Portion of fractured scaphoid may become avascular Intercarpal joints (Figure 9-7) Between 8 carpal bones Stabilized by numerous ligaments Joint spaces usually communicate Movements generally gliding, with some abduction and flexion Carpometacarpal joints—total of three joints One joint for thumb—wide range of movements Two joints for fingers—movements largely gliding type Thumb carpometacarpal joint is unique and important functionally • Loose-fitting joint capsule • Saddle-shaped articular surface • Movements—extension, adduction, abduction, circumduction, and opposition • Opposition—ability to touch tip of thumb to tip of other fingers— movement of great functional significance Representative Synovial Joints Metacarpophalangeal joints (Figure 9-8) Rounded heads of metacarpals articulate with concave bases of proximal phalanges Capsule surrounding joints strengthened by collateral ligaments Primary movements are flexion and extension Interphalangeal joints Typical diarthrotic, hinge-type, synovial joints Occur between heads of phalanges and bases of more distal phalanges Two categories: • PIP joints—proximal interphalangeal joints (between proximal and middle phalanges) • DIP joints—distal interphalangeal joints (between middle and distal phalanges) Hip joint (Figure 9-9) Stable joint because of shape of head of femur and of acetabulum A joint capsule and ligaments contribute to joint’s stability Knee joint (Figures 9-10 and 9-11) Largest and one of most complex and most frequently injured joints Tibiofemoral joint is supported by a joint capsule, cartilage, and numerous ligaments and muscle tendons Permits flexion and extension and, with knee flexed, some internal and external rotation Ankle joint (Figure 9-12) Hinge type of synovial joint Articulation between lower ends of tibia and fibula and upper part of talus Joint is “mortise” or wedge-shaped • Lateral malleolus lower than medial Internal rotation injury results in common “sprained ankle” • Involves anterior talofibular ligament Other ankle ligaments may also be involved in sprain injuries—example is deltoid ligament External ankle rotation injuries generally involve bone fractures rather than ligament tears • First-degree ankle injury—lateral malleolus fractured • Second-degree ankle injury—both malleoli fractured • Third-degree ankle injury—fracture of both malleoli and articular surface of tibia Representative Synovial Joints Vertebral joints (Figures 9-13 and 9-14) Vertebrae are connected to one another by several joints to form a strong, flexible column Bodies of adjacent vertebrae are connected by intervertebral disks and ligaments Intervertebral disks are made up of two parts: • Annulus fibrosus—disk’s outer rim, made of fibrous tissue and fibrocartilage • Nucleus pulposus—disk’s central core, made of a pulpy, elastic substance Types and Range of Movement at Synovial Joints Measuring range of motion (Figure 9-14) Range of motion (ROM) assessment used to determine extent of joint injury ROM can be measured actively or passively; results of both methods generally about equal ROM measured by instrument called a goniometer Angular movements—change the size of the angle between articulating bones Flexion—decreases the angle between bones; bends or folds one part on another (Figures 9-15, A, 9-17, and 9-18) Extension and hyperextension (Figure 9-17) • Extension—increases the angle between bones, returns a part from its flexed position to its anatomical position • Hyperextension—stretching or extending part beyond its anatomical position (Figures 9-18, 9-20, and 9-22) Plantar flexion and dorsiflexion (Figure 9-24) • Plantar flexion—increases angle between top of foot and front of leg • Dorsiflexion—decreases angle between top of foot and front of leg Abduction and adduction (Figures 9-18 and 9-22) • Abduction—moves a part away from median plane of body • Adduction—moves a part toward median plane of body Circular movements Rotation and circumduction • Rotation—pivoting a bone on its own axis (Figure 9-15, D) • Circumduction—moves a part so that its distal end moves in a circle Supination and pronation (Figure 9-19, B) • Supination—turns the hand palm side–up • Pronation—turns the hand palm side–down Types and Range of Movement at Synovial Joints Gliding movements—simplest of all movements; articular surface of one bone moves over articular surface of another without any angular or circular movement Special movements Inversion and eversion (Figure 9-24, B) • Inversion—turning sole of foot inward • Eversion—turning sole of foot outward Protraction and retraction (Figure 9-16, B) • Protraction—moves a part forward • Retraction—moves a part backward Elevation and depression • Elevation—moves a part up • Depression—lowers a part Cycle of Life: Articulations Bone development and the sequence of ossification between birth and skeletal maturity affect joints Fontanels between cranial bones disappear Epiphysial plates ossify at maturity Older adults ROM decreases Changes in gait occur Skeletal diseases manifest as joint problems Abnormal bone growth (lipping)—influences joint motion Disease conditions can be associated with specific developmental periods The Big Picture: Articulations Mobility of the upper extremity is extensive because of the following: Arrangement of bones in shoulder girdle, arms, forearm, wrist, and hand Location and method of attachment of muscles to bones Proper functioning of joints Mobility and extensive ROM is needed to position the upper extremity and hand to permit grasping and manipulation of objects, thus enabling effective interaction with objects in external environment