Liver
advertisement
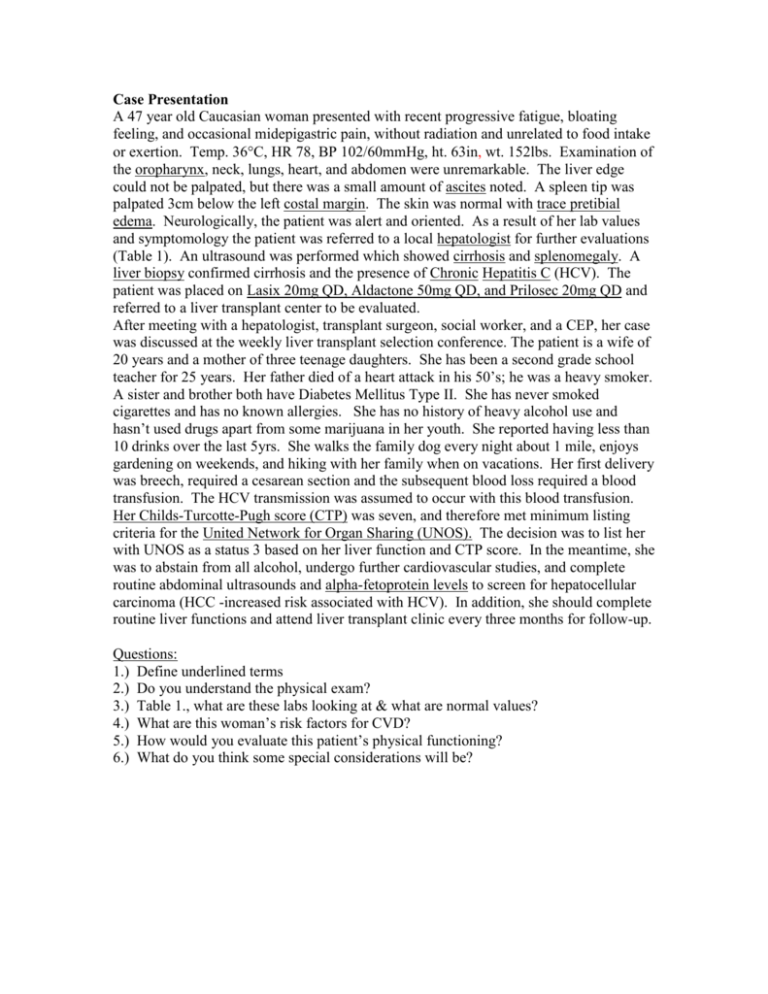
Case Presentation A 47 year old Caucasian woman presented with recent progressive fatigue, bloating feeling, and occasional midepigastric pain, without radiation and unrelated to food intake or exertion. Temp. 36C, HR 78, BP 102/60mmHg, ht. 63in, wt. 152lbs. Examination of the oropharynx, neck, lungs, heart, and abdomen were unremarkable. The liver edge could not be palpated, but there was a small amount of ascites noted. A spleen tip was palpated 3cm below the left costal margin. The skin was normal with trace pretibial edema. Neurologically, the patient was alert and oriented. As a result of her lab values and symptomology the patient was referred to a local hepatologist for further evaluations (Table 1). An ultrasound was performed which showed cirrhosis and splenomegaly. A liver biopsy confirmed cirrhosis and the presence of Chronic Hepatitis C (HCV). The patient was placed on Lasix 20mg QD, Aldactone 50mg QD, and Prilosec 20mg QD and referred to a liver transplant center to be evaluated. After meeting with a hepatologist, transplant surgeon, social worker, and a CEP, her case was discussed at the weekly liver transplant selection conference. The patient is a wife of 20 years and a mother of three teenage daughters. She has been a second grade school teacher for 25 years. Her father died of a heart attack in his 50’s; he was a heavy smoker. A sister and brother both have Diabetes Mellitus Type II. She has never smoked cigarettes and has no known allergies. She has no history of heavy alcohol use and hasn’t used drugs apart from some marijuana in her youth. She reported having less than 10 drinks over the last 5yrs. She walks the family dog every night about 1 mile, enjoys gardening on weekends, and hiking with her family when on vacations. Her first delivery was breech, required a cesarean section and the subsequent blood loss required a blood transfusion. The HCV transmission was assumed to occur with this blood transfusion. Her Childs-Turcotte-Pugh score (CTP) was seven, and therefore met minimum listing criteria for the United Network for Organ Sharing (UNOS). The decision was to list her with UNOS as a status 3 based on her liver function and CTP score. In the meantime, she was to abstain from all alcohol, undergo further cardiovascular studies, and complete routine abdominal ultrasounds and alpha-fetoprotein levels to screen for hepatocellular carcinoma (HCC -increased risk associated with HCV). In addition, she should complete routine liver functions and attend liver transplant clinic every three months for follow-up. Questions: 1.) Define underlined terms 2.) Do you understand the physical exam? 3.) Table 1., what are these labs looking at & what are normal values? 4.) What are this woman’s risk factors for CVD? 5.) How would you evaluate this patient’s physical functioning? 6.) What do you think some special considerations will be? You guys are doing great, but unfortunately the patient is not… Over the next two years the patient gradually decompensated in physical functioning and liver dysfunction. She began working half days at school, but eventually had to go on full disability due to fatigue, worsening edema and ascites, and the beginning symptoms of encephalopathy. Her exercise regiment had been reduced to one or two bouts of 10 min. walks/day when she felt she had enough energy. Six months after leaving work and almost three years after her initial liver transplant (ltx) evaluation the patient underwent an orthotopic liver transplant (ltx). Two days after an uncomplicated ltx, a physical therapist had the patient performing ROM exercises in the ICU. On post-op day 4, the patient had progressed to unassisted ambulation and physical therapy referred the exercise therapy to a CEP. Questions: 1.) Define underlined terms 2.) What would you do with this patient? Keep plugging away… The patient was discharged on post-op day 6 with the following post tx pharmacological therapies: prednisone taper (200mg QD to 5mg QD over the next six weeks), tacrolimus 2mg BID, mycophenolate mofetil 1000mg BID, acyclovir 800mg QID, trimethoprim/sulfamethoxazole 80mg/400mg TIW, omeprazole 20mg BID, and magnesium 300mg TID. She was told to obtain biweekly blood draws at her local lab, with results to be faxed to the liver transplant office so her liver functions could be assessed regularly. She was also instructed to attend liver transplant clinic weekly for the first month. The CEP also gave her a written exercise prescription and exercise logs for adherence and motivation. Questions: 1.) Define underlined terms 2.) Now, what would you kind of exercise prescription would you send this patient home with and what is your next plan of action for this patient? Time marches on… Three months post transplant, the patient was seen at the liver transplant clinic for routine follow-up. Her liver function tests were elevated again. A liver biopsy was performed to differentiate between HCV recurrence and organ rejection. The histology report confirmed acute rejection and her immunosuppressive medications were recycled. The patient met with the CEP and reported increased duration and intensity of exercise and “feeling stronger every day”. Questions: 1.) Define underlined terms 2.) What would you discuss at this patient at this visit? Very sad, but true… At six months post transplant, she had been released to begin working part-time and also to resume driving. After working for one week, she received a call from the liver transplant center informing her that her LFT’s were elevated again. Another biopsy was performed which revealed HCV recurrence. Interferon and ribavirin therapy was initiated. Over the next few weeks, exercise phone follow-up calls were not returned to the CEP and there was also no response via postal mail. Ten months post transplant, the patient attended clinic to have a physician complete disability leave papers for work. The patient was placed on an antidepressant. The patient told the CEP that she has no energy to exercise and feels that she must conserve her energy just for routine errands and childcare and that she’ll contact the CEP when she feels strong enough to resume her exercise program. Questions: 1.) Define underlined terms 2.) Now what will you do? . Table 1. Laboratory Values – Pre transplant Creatinine 0.6 mg/ Alk Phos BUN 20.2 mg/dL AST Hgb 11.1 g/dL ALT Hct 33.1 % Bili, t WBC 6.9 thous/mcl PT Sodium 138.0 mmol/L Potassium 2.9 mmol/L Normal range values vary between laboratories 148.0 U/L 69.0 U/L 77.0 U/L 1.2 mg/dL 14.0 sec