Improvement in neurological outcomes of asphyxiated - Skills
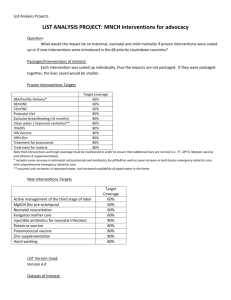
advertisement

MESOAMERICAN HEALTH INITIATIVE MASTER PLAN MATERNAL, NEONATAL AND REPRODUCTIVE HEALTH WORKING GROUP Submitted to: Public Health Institute Bill and Melinda Gates Foundation The final conformation of this document was carried out by Juan Díaz, Bernardo Hernández, Edgar Kestler, Sarah Lewis and Elvia de la Vara. The elaboration of the document received input and incorporated elements from discussion with the members of the core group of maternal, neonatal and reproductive health, integrated by Bernardo Hernández (chair, INSP-MEXICO), Edgar Kestler (co-chair, CIESAR, Guatemala), Ana Langer (Engender Health), Dilys Walker (INSP, Mexico), Emma Iriarte (GTZ-PRAIM Honduras), Isabela Danel (CDC-CAP), France Donnay (Gates Foundation) and Denis Alemán (PROFAMILIA, Nicaragua), and from the focal groups of all the countries of the region: Rosely Serrano and Evelyn Morales (Costa Rica), Natalia Largaespada (Belize), Douglas Jarquín (El Salvador), Ma. Del Carmen Hernández (Guatemala), Claudia Quiroz (Honduras), Geneva González and Yadira Carrera (Panama), Clelia Valverde (Nicaragua) and Rufino Luna (Mexico). We also appreciate the comments and contributions of Rebecca Aced-Molina (PHI, USA). October 2009 MASTER PLAN: MATERNAL, NEONATAL AND REPRODUCTIVE HEALTH GROUP TABLE OF CONTENTS Acronyms Executive summary 1. Theory of change 1.1. Problem 1.2. Target population 1.3. Vision 1.4. Levers 1.5. Outcomes 2. Literature-based evidence for effective practices 2.1. Summary of relevant effective practices 2.2. Outcomes, impacts and cost effectiveness of relevant effective practices 3. Possible solutions: selection of effective practices for regional implementation 3.1. Maternal health 3.2. Neonatal health 3.3. Reproductive health and family planning 3.4. Implementation and timing of effective practices 3.5. Rationale for effective practices 4. Integration 4.1. Integration within the maternal, neonatal and reproductive health pillar 4.2. Integration across the vaccine, nutrition, and vector pillars 5. Human and systems capacity building 5.1. Maternal health 5.2. Neonatal health 5.3. Reproductive health and family planning 5.4. Needs 5.5. Available resources 6. Feasibility 6.1. Barriers and challenges 6.2. Unintended consequences 6.3. Protecting other programs 7. Newly emerging issues 8. Policy landscape 9. Indicators for monitoring and evaluation 10. In-text references 11. Appendices 11.1. Selected demographic and health indicators for the Mesoamerican region, 2009 11.2. Examples of interventions selected by countries 11.3. Neonatal health interventions: extensive listings MASTER PLAN: MATERNAL, NEONATAL AND REPRODUCTIVE HEALTH GROUP ACRONYMS BCG Bacillus Calmette-Guérin BEmOC Basic Emergency Obstetric Care CEmOC Comprehensive Emergency Obstetric Care CHW Community Health Worker COMISCA Council of Central American Ministries of Health EmOC Emergency Obstetric Care FP Family Planning HBV Hepatitis B Virus KMC Kangaroo Mother Care LBW Low Birth Weight MHI Mesoamerican Health Initiative MMR Maternal Mortality Rate MNRH Maternal, Neonatal and Reproductive Health MTC/HIV Mother to child transmission/HIV NMR Neonatal Mortality Rate PMR Perinatal Mortality Rate PAHO Pan-American Health Organization RH Reproductive Health SRH Sexual and Reproductive Health SRR Sexual and Reproductive Rights STI Sexually Transmitted Infection TBA Traditional Birth Attendant TFR Total Fertility Rate WHO World Health Organization MASTER PLAN: MATERNAL, NEONATAL AND REPRODUCTIVE HEALTH GROUP EXECUTIVE SUMMARY The Mesoamerican Health Initiative (MHI) constitutes an effort to improve health conditions in this region (Central America and nine states of the southern part of Mexico), as a way to respond to the common health challenges and needs faced by the region. So far, the MHI has conformed four working groups: nutrition, immunizations, vector-borne diseases and maternal, neonatal and reproductive health. In this document, we present the Master Plan for maternal, neonatal and reproductive health (MNRH). This plan has been prepared with the participation of a group of international experts, as well as representatives of the countries of the region. Goals and objectives The most important goals in this area are to reduce maternal mortality by 75%, reduce neonatal mortality by 50%, and achieve universal access to reproductive health services including family planning by the year 2015, in line with the United Nations 2009 Millennium Development Goals (MDG) report. The main objectives are as follows: To increase access to childbirth care provided by qualified and competent personnel, especially in rural and marginalized urban areas. To increase access to basic emergency obstetric care, especially in rural and marginalized urban areas. To reduce the gap between the poorest and richest income quintiles in the proportion of women giving birth with skilled personnel, in all countries in the region. To reduce neonatal mortality by improving obstetric care and implementing actions to improve the quality of immediate care provided to the newborn, especially in communities removed from large metropolitan areas. To increase access to and improve the quality of services that offer permanent and reversible contraceptive methods for both men and women, and to implement actions to reduce common barriers to contraceptive access in the region, especially in rural areas and for adolescents and youth. Theory of change Although there have been improvements in basic maternal, neonatal and sexual and reproductive health indicators in the Mesoamerican region during the past 10 years, on average unacceptably high maternal mortality ratios and neonatal mortality rates persist. All national governments have designed policies and programs to reduce maternal and neonatal mortality and to improve reproductive health services with an emphasis on family planning. However, these programs have not been fully implemented and the limited available evaluations indicate that most programs have not achieved the desired impact. The lack of effective implementation of programs and interventions is due, fundamentally, to deficiencies within the systems of service and resource provision which fail to make interventions fully accessible to the whole population. This Plan’s main objective is to increase access to high quality services and promote the equitable utilization of those services in order to reduce maternal and neonatal mortality, thus contributing to the achievement of Goals 3, 4 and 5 of the MDGs. However, interventions should not focus solely on service provision; in addition to identifying and implementing evidence-based interventions, the Plan addresses ways to promote empowerment and greater community participation, strategies which have proven essential for the effective implementation of sustainable interventions. The Plan’s main targets are women of reproductive age (10-49 years old), and newborns, also addressing men’s participation and promoting community participation. Proposed actions will be directed mainly to the poorest populations, indigenous groups, adolescents and young adults, MASTER PLAN: MATERNAL, NEONATAL AND REPRODUCTIVE HEALTH GROUP and the rapidly growing marginalized urban populations. The plan recognizes the high importance of addressing adolescent health as a high priority.. Our vision is that by 2015 the region’s entire population will enjoy equitable access to high quality services and that all people will be able to exercise their sexual and reproductive rights, including the right to decide freely and responsibly the number, spacing and timing of their children; to have the information and means to do so, and the right to attain the highest standard of sexual and reproductive health. It also includes their right to make decisions concerning reproduction free of discrimination, coercion and violence, as expressed in human rights documents. For this plan we have identified the following main levers: Political will. Several key actors, like the Mesoamerican Public Health System (SMSP in Spanish), the Central American Council of Ministries of Health (COMISCA in Spanish) and the Pan-American Health Organization (PAHO) are supporting this initiative. Health policy. Most of the countries of the region have already developed progressive national policies and programs and put into action projects that incorporate the most current concepts of reproductive health care. Financial and technical support. All national governments have committed to supporting this initiative. Additionally, the Bill and Melinda Gates Foundation (BMGF) has provided funds for the planning stage, and the Carso Health Institute has already begun to support various SMSP activities. These two organizations and the Spanish government have shown a clear interest in supporting activities for at least five years. Technical support has been essential for the development of the Strategic Assessment and for defining the programs to be implemented in the countries. The continuation of this support will be very important for the establishment of sustainable Mesoamerican-based coordination mechanisms capable of supporting the scaling up of interventions. Existing regional technical capacity for research and training. Political support from the Group of Twenty (G-20). Identification of effective practices An extensive literature review was conducted to identify evidence-based effective practices, and to document their outcomes, impacts and cost effectiveness. The next step was the selection of the most promising ones which compose the proposals for resolving the problems identified in the Strategic Assessment. These interventions were discussed extensively within the working group and with the country representatives. The group has focused on interventions aimed principally at the community and primary care level, targeting mainly poor and indigenous population. The document discusses the implementation of each practice and the factors necessary to achieve sustainability of these practices after the MHI ends. The main interventions proposed in each area are: a) Maternal health: implementation of basic Emergency Obstetric Care (EmOC), and interventions aimed at improving care of obstetric emergencies related to infections, eclampsia, hemorrhage and abortion; and community awareness, education and training to improve these outcomes. b) Neonatal health: essential newborn care, care for the low birth weight newborn and emergency care for newborns with complications. c) Reproductive health and family planning: implement quality family planning services for adolescents, ensure access to counseling and services for at least six contraceptive methods, ensure access to vasectomy, and post-partum and post-abortion contraceptive counseling and services. MASTER PLAN: MATERNAL, NEONATAL AND REPRODUCTIVE HEALTH GROUP Implementation and timing of effective practices Although the implementation of a given intervention should take into account its specific characteristics, the following factors were identified as relevant for the implementation of effective practices. This Master Plan applies to the first five years of the MHI. Capacity building is a crucial aspect of most of the interventions proposed, and it should be considered as an initial step of the implementation of all interventions. Definition of implementation sites in each country, focusing interventions on the poorest areas, and giving emphasis to the community and primary health care level. Although the proposed interventions have demonstrated effectiveness in various settings, it is advisable to undertake operations research in some locations to define which interventions are best for the country and the components that should be scaled up. Interventions should build upon existing structures and organizations in each country. Governance mechanisms should be clearly defined to facilitate coordination of actions. Rationale for effective practices Some of the reasons why we expect the proposed interventions to have the most potential to solve the problems identified in the Strategic Assessment are: While constituting a regional strategy, the effective practices will constitute a public good that may generate economies of scale for all countries. A capacity building component is considered a crucial part of the implementation process of these interventions, but monitoring and supervision is equally important to incorporate into the intervention packages. The implementation of effective family planning interventions is crucial for MNRH because, as stated in the last High-Level Meeting on Maternal Health for MDG5, family planning is one of the most cost-effective development investments because ensuring access to modern contraception can prevent up to 40% of maternal deaths. Integration A number of interventions in MNRH impact other indicators within this focus area. Therefore the implementation of interventions, especially personnel training, should keep this integration in mind both within MNRH and to some degree with the other pillars of this initiative, in order to reap the most benefit across programs. Human and systems capacity building The Master Plan assesses human and systems capacity existing in the region, and identifies areas where capacity building is needed for successful implementation of the proposed interventions. In general, the health systems have great limitations in their infrastructure, though this varies considerably across countries. Moreover, training systems are generally quite weak, thus strengthening local training capacity is a high priority of this plan. Feasibility, barriers and challenges, and other issues related to the implementation of the interventions The proposed interventions are in accordance with those proposed and tested in other regions by international organizations, including the BMGF. There is a clear need for strengthening human resources for the implementation of interventions. The feasibility and sustainability of the proposed interventions rely heavily on the political commitment of governments of the region, both to invest in personnel training and to support the implementation of actions. Feasibility and sustainability will also depend on the ability of the programs to integrate interventions and strengthen health systems to respond to sexual and reproductive health needs and respect sexual and reproductive rights. MASTER PLAN: MATERNAL, NEONATAL AND REPRODUCTIVE HEALTH GROUP The key MNRH problem identified in the region is the unsuccessful implementation of programs, standards and projects. Besides the financial factor, aspects such as managerial deficiencies, lack of trained personnel, lack of effective commitment, poor quality of health personnel and managerial systems, and political and ideological opposition to family planning are the main barriers to effective implementation in Mesoamerica, and as such should be carefully addressed. The implementation of interventions proposed in this Master Plan may lead to unintended consequences. One is that the successful implementation of interventions, as well as promotion of community participation may increase the demand for health services. The proposed interventions have a low potential to negatively influence the performance of other programs. However, it is important to maintain communication between maternal, neonatal and family planning programs with other ongoing programs to minimize potential negative effects and promote synergies among programs. At the same time, some emerging issues may affect the implementation and sustainability of the proposed interventions: political instability, epidemics and other health threats (especially if they lead to migration), political opposition to family planning, natural disasters and economic and financial crisis. The Master Plan also discusses the policy landscape in consideration of the issues that may affect the implementation of interventions. Aspects addressed include the commitment of countries to improve health, and the support and participation of international organizations such as COMISCA and PAHO. Indicators for monitoring and evaluation In the final section of the Master Plan we propose specific indicators for the monitoring and evaluation of the proposed interventions, at the level of impact, outcomes and outputs. Evaluation is key for improving health systems and this plan aims to help improve evaluation systems in all of the countries. Therefore these indicators are an important initial input for the design of evaluation plans and represent an important first step in this initiative’s goal of improving MNRH in Mesoamerica. MASTER PLAN: MATERNAL, NEONATAL AND REPRODUCTIVE HEALTH GROUP 1. THEORY OF CHANGE Regional goals The most important goals in this area are to reduce maternal mortality by 75% by the year 2015, to reduce neonatal mortality and to achieve universal access to reproductive health services, including family planning, following the United Nations 2009 Millennium Development Goals report. Achieving these goals may require different activities, since countries have at present different situations. General demographic and health indicators are shown in appendix 1. This proposal includes the development of interventions to improve obstetric and neonatal emergencies care, as well as to increase access to family planning methods, strengthening health services and promoting community empowerment and participation in the Mesoamerican region (Central America and the States in Southern Mexico). Objectives To increase the access to childbirth care provided by qualified and competent personnel, especially in rural and marginalized urban areas. To increase the access to basic emergency obstetric care, especially in rural and marginalized urban areas. To reduce the gap in the proportion of women giving birth with skilled personnel between women in the poorest and richest income quintiles in all countries in the region. To reduce neonatal mortality by improving obstetric care and by implementing actions to improve the quality of immediate care provided to the newborn, especially in communities removed from large metropolitan areas. To increase access to and quality of services that offer permanent and reversible methods for both men and women, and to implement actions that promote the reduction of the barriers to contraceptive access common in rural areas and among indigenous women, adolescents and youth. 1.1 Problem Despite significant improvements in basic maternal, neonatal, and sexual and reproductive health indicators in the Mesoamerican region during the past 10 years, on average unacceptably high maternal mortality ratios and neonatal mortality rates persist. If reductions in maternal and neonatal mortality continue at the same pace observed in recent years, it is likely that most countries in the region will fail to meet the Millennium Development Goals, especially goals 4 and 5. All national governments in the region have recognized the great importance of improving the quality of reproductive health care and have designed policies and programs to reduce maternal and neonatal mortality, and to improve reproductive health services with an emphasis on family planning. However, these programs have not been fully implemented and the limited evaluations that do exist indicate that in many cases, programs have not achieved the desired impact. The lack of effective implementation of programs and interventions is due, fundamentally, to deficiencies within the systems of service and resource provision which fail to make interventions fully accessible to the whole population. The main reasons for unsuccessful implementation are MASTER PLAN: MATERNAL, NEONATAL AND REPRODUCTIVE HEALTH GROUP the endemic lack of funding for health prevalent in all countries in the region and the lack of competent and skilled personnel, especially in those areas removed from large urban metropolitan areas. Although all countries have implemented training programs for health personnel, these programs have limited resources, are of questionable quality, and demand for training far exceeds systems capacity. This is further aggravated by the high staff turnover common in all Mesoamerican countries. Furthermore, the global economic crisis continues to threaten efforts to achieve the Millennium Development Goals. Pressures on donor countries to cut aid budgets may limit resources available to developing countries, which in turn will face further difficulties in tackling the crisis and providing for the needs of their populations. This Plan’s main objective is to increase access to high quality services and promote the equitable utilization of those services in order to reduce maternal and neonatal mortality, thus contributing to the achievement of Goals 3, 4 and 5 of the Millennium Development Goals. However, interventions should not focus solely on service provision; in addition to identifying and implementing evidence-based interventions, the Plan addresses ways to promote empowerment and greater community participation, strategies which have proven essential for the effective implementation of sustainable interventions. 1.2 Target population The Plan’s objectives are the improvement of health care services for pregnant women and newborns and increased access to high quality family planning services that result in increased use of effective contraceptives and a decrease in unwanted and high-risk pregnancies. Thus the Plan’s main targets are women of reproductive age (10-49 years old) and newborns. Furthermore, the Plan will include actions aimed at increasing men’s participation and promoting community participation at large. Proposed actions will be directed mainly to the poorest populations, indigenous women and communities, and adolescents and young adults. A reinforcement of health information systems, including geographic information systems, may help to identify the location of target groups with lower access to obstetric, neonatal or family planning services. The main target groups — poor and indigenous populations — are mainly concentrated in rural localities, so these areas necessarily compose the Plan’s most important focal point. Nevertheless, since the region’s countries are all undergoing more or less rapid processes of urbanization, we must also consider actions geared toward the rapidly growing marginalized urban populations, as they also concentrate vulnerable groups of people. This is important when considering interventions aimed at improving emergency obstetric care, primarily focused on the referral hospital setting. 1.3 Vision The main objectives are to significantly reduce the maternal mortality ratio and the neonatal mortality rate, and to increase the prevalence of effective contraceptive use as a means to reduce unmet need and unwanted pregnancies — an important factor responsible for the higher than expected maternal mortality ratios in the region. The conditions necessary to achieve these goals are: a) improve access to high quality reproductive health services including family planning, prenatal care, labor and delivery, and postpartum and newborn care; 1 b) promote the use of these services among the entire population, ensuring access by the poor and marginalized 1 Improving quality and access to obstetric care are crucial processes, and each one deserves full attention on its own. However, we recognize in this plan that an increase in access without improving quality of obstetric care may not give the expected results. MASTER PLAN: MATERNAL, NEONATAL AND REPRODUCTIVE HEALTH GROUP including indigenous communities and people living in rural and marginalized urban areas; and c) promote community education programs as a means to empower the community through acquiring healthy behaviors, becoming actively involved in health care, and exercising social control over health services. Greater emphasis on bridging the gap between “knowing” and “doing” is also a necessary precondition. The region has already reached the point at which it becomes necessary to concentrate the efforts of “thinkers” or planners, governments and donors to stimulate and provide the “doers” with the conditions required to implement and evaluate sustainable interventions; and as a consequence shift from service delivery models of wealth transference to empowerment models of wealth creation. The evidence shows that community empowerment and participation via education is imperative in order to make significant and sustainable changes. We hope that by 2015 the region’s entire population will enjoy equitable access to high quality services and that all people will be able to exercise their sexual and reproductive rights, including the right to decide freely and responsibly the number, spacing and timing of their children and to have the information and means to do so, and the right to attain the highest standard of sexual and reproductive health. It also includes their right to make decisions concerning reproduction free of discrimination, coercion and violence, as expressed in human rights documents.. Consequently, significant improvements in maternal and neonatal morbidity and mortality indexes will reflect these developments. 1.4 Levers Political will. The Mesoamerican Public Health System (SMSP in Spanish), which has been incorporated into the Mesoamerican Development Project, has the explicit support of all countries in the region. In addition, the Central American Council of Ministries of Health (COMISCA in Spanish) is supporting activities in collaboration with the Pan-American Health Organization (PAHO) and other regional institutions. This international collaboration, including the creation of the Mesoamerican Institute of Public Health (IMSP in Spanish), is the cornerstone that will facilitate and sustain the implementation of the Plan. Health policy. The countries of the region have for the most part already developed progressive national policies and programs and put into action projects that incorporate the most current concepts of reproductive health care. This includes the concept that reproductive health is a right of the people and that the organized community must actively participate in programs from the planning stages onward. Financial and technical support. All national governments have committed to supporting this initiative. Additionally, the Bill and Melinda Gates Foundation has provided funds for the planning stage, and the Carso Health Institute has already begun to support various IMSP activities. These two organizations and the Spanish government have shown a clear interest in supporting activities for at least five years. Grant funds are not sufficient to ensure the implementation of all initiatives (thus making sustainability a key issue), but these funds are an essential resource for intervention design and implementation. Technical support has been essential for the development of the Situation Analysis and for defining the programs to be implemented in the countries. We are hopeful that this support will continue during the first five years of implementation and evaluation until the establishment of sustainable Mesoamerican-based coordination mechanisms capable of supporting the scaling up of interventions. Existing regional technical capacity for research and training. Several countries in the region have research and training centers that can play an essential role in implementing initiatives. Additionally, the IMSP may take on a very important role in coordinating activities in the region thereby increasing the cost-effectiveness of actions. MASTER PLAN: MATERNAL, NEONATAL AND REPRODUCTIVE HEALTH GROUP Political support from the Group of Twenty (G-20). According to the Millennium Development Goals Report (United Nations, 2009) the leaders of the G-20 have agreed to make available large additional amounts of international liquidity to countries in crisis in order to fight protectionism and reform the international financial system. They have also reasserted existing commitments to provide more aid and debt relief to the poorest countries to safeguard development in low-income countries. 1.5 Outcomes All countries in the region have committed to achieving the Millennium Development Goals. Our proposal can significantly advance progress in meeting three of those goals. With support from PAHO and other international agencies, all of the countries have developed strategies and programs to improve the quality of prenatal, childbirth and postpartum care with the goal of reducing maternal morbidity and mortality (Goal 5) and to collaborate in achieving Goal 4 through reducing neonatal mortality. PAHO’s Regional Initiative for Maternal Mortality Reduction has been used by some countries to design strategies for reducing maternal mortality. Commitments have also been made to meet the goal of achieving universal access to reproductive health services as part of Goal 5, especially universal access to family planning and labor and delivery care by qualified and competent personnel. Increased community participation in reproductive health has been acknowledged as an essential success factor for improving reproductive health services. Several countries are already implementing initiatives in this regard, some of which are part of the PAHO Healthy Communities initiative. These initiatives can have a positive impact on health while also contributing to the achievement of Goal 3 (promoting gender equality and empowerment of women). All of the countries have put into practice programs and interventions to achieve these regional objectives, but so far implementation efforts have been either inadequate to achieve the results required to meet established goals or have not been evaluated to assess effectiveness. 1.5.1 Regional goals The most important regional goal is to reduce maternal mortality by 75% by the year 2015. According to the United Nations 2009 Millennium Development Goals report, the commitment also includes universal access to reproductive health services including family planning, by 2015. The region has experienced some progress in reducing maternal mortality but results are inadequate; in particular the coverage of births attended by skilled service delivery personnel and access to basic emergency obstetric care are lacking, especially in rural and marginalized urban areas. Figures for this indicator also have an important variability between countries, ranging from 31.4% (Guatemala) to 98.7% (Costa Rica). To get nearer to the universal coverage objective, greater efforts must be made to increase access to childbirth care provided by qualified and competent personnel and reduce the abysmal gap in access between the poorest and richest segments of the population. The percentage of women giving birth with a skilled provider is 50 or more percentage points lower among the poorest women (quintile 1) than the richest (quintile 5) in all countries of the region. Improvements in delivery and postpartum care also necessarily affect neonatal mortality. The second major objective of the Plan is to reduce neonatal mortality and improvements in obstetric care should decrease neonatal mortality rates. However, only improving obstetric care is not enough to reduce neonatal mortality; actions to improve the quality of immediate care provided to the newborn are also crucial, especially in communities removed from large metropolitan areas. Reducing unwanted pregnancies is an important regional goal that would also affect the reduction of maternal morbidity and mortality, especially through the reduction of unsafe abortions. Although contraceptive prevalence has increased in all countries, significant unmet demand MASTER PLAN: MATERNAL, NEONATAL AND REPRODUCTIVE HEALTH GROUP persists, particularly because access to contraceptive service delivery points that offer at least six methods remains highly insufficient. Additionally, significant proportions of the population identify themselves as users of natural or traditional contraceptive methods but do not seek any type of health services-based counseling or consultation. The objective then is to increase access to and quality of services that offer permanent and reversible methods for both men and women, and to implement actions that promote the reduction of the barriers to contraceptive access, common among indigenous women, adolescents and youth. An increase in the prevalence of the use of highly effective contraceptives alongside a reduced use of less effective natural and traditional methods is expected. To reach this objective it will be important to create a regional system for purchasing contraceptive supplies and methods to ensure quality and lower costs. A purchasing system including a distribution route and administrative procedures is a necessary pre-condition for ensuring regional self-sustainability. If this type of agreement were reached by regional bodies such as the Presidential Summit or COMISCA, the following actions would take place: i) finance and health ministers will earmark the budget for this system, ii) the system will be made a part of national budget cycles, and iii) the necessary amount of contraceptive methods will be purchased every year. 1.5.2 Country-specific objectives Increase access to and use of modern contraceptive methods among indigenous populations, the poorest wealth quintiles, and otherwise vulnerable populations in the region. It is important that countries like Guatemala and Honduras continue efforts to deliver a guaranteed set of benefits (including family planning) to rural and indigenous populations via decentralized services which make use of third party providers. El Salvador should continue its rural community services delivery model which uses basic health systems teams that include actions in the areas of education, promotion and delivery of family planning services. One of the main actions to achieve this goal is to train family planning service providers who understand the cultures of different indigenous and ethnic communities and are capable of working in the local language. Ensuring the availability of contraceptive methods is key. The increasing decline in international collaboration to obtain contraceptive methods has forced countries to implement programs to ensure method availability. With initial support from USAID, some countries have managed to sustain these efforts, but others are facing great difficulties in maintaining contraceptive availability. The main challenge to ensuring contraceptive supply is not only securing funding for the acquisition of methods and supplies, but also developing capacities such that the distribution of supplies is efficient and methods are available in all family planning service sites. Thus, one type of intervention would strengthen and consolidate the work that national contraceptive supply committees are already carrying out in individual countries. By 2015 it is expected that all countries in the region will have legally secured a protected budget to ensure acquisition and will have implemented efficient distribution systems. Expand family planning services, with at least six modern methods available in countries’ health network units or facilities. Although family planning services are generally available in all countries and their respective health care networks, in reality challenges remain with respect to ensuring the permanent availability of at least the following methods: an oral method, an injectable method, a barrier method, IUD, VSC (or in its absence the ability to refer to a center that does offer it) and guidance on the proper use of fertility awareness based methods, especially the Standard Days Method (SDM) used with and without Cycle beads. The related intervention would consist of ensuring that all health system units offer this minimum range of services, as well as require clinical and counseling capacity development planning and implement a logistics cycle subsystem to reduce the problem of shortages or stock outs commonly occurring in the region. MASTER PLAN: MATERNAL, NEONATAL AND REPRODUCTIVE HEALTH GROUP Scale up post-partum and post-abortion family planning programs. The provision of guidance and contraceptive services in the post-partum and post-abortion periods is a proven effective strategy to decrease the rate of unwanted pregnancies and to increase birth intervals. The plans of several countries in the region include the implementation of this strategy and capacity for personnel training already exists. Operational research to test strategies for implementing emergency obstetric care in all health centers. An examination of the most appropriate strategies to ensure that there are competent personnel and resources for the provision of emergency obstetric care in all (secondary level) health centers providing labor and delivery care is imperative, as is an efficient transport system to transfer serious cases to tertiary level hospitals. Provide universal access to treatment for obstetric emergencies in health centers in rural areas. Acute and unexpected complications during labor, delivery, and puerperium are responsible for most maternal deaths, principally hemorrhage, eclampsia, infections, and complications of abortion. The complications responsible for maternal deaths are quite serious in and of themselves, but in most cases death can be avoided by taking relatively simple therapeutic measures in a timely manner or by transferring the patients to better equipped facilities. Furthermore, a large proportion of complications are preventable: taking precautions to prevent infections, putting into practice active management of the third stage of labor, and avoiding lacerations. The most basic intervention comprises training the health professionals attending deliveries, treating the most common complications, and detecting complications that must be referred urgently to a better equipped hospital. Training should be theoretical as well as practical and newly trained providers must be supervised periodically, especially during the first months after training. It is also crucial to implement a system for transferring complicated cases without delays. Improve the quality of basic care, detection of danger signs, and treatment of neonatal emergencies in primary health centers. All physicians, nurses, and auxiliary nurses working in health centers where deliveries are attended should be trained to give basic care to newborns, including appropriate cord clamping, prevention of infections, warming, and treatment of asphyxia. In addition, all personnel should be trained to detect danger signs or complications such as intense jaundice, hypothermia, intense paleness, or severe indrawing of breath. Any newborn experiencing these symptoms should be rapidly transferred to a center with more resources including at least one pediatrician, ideally a neonatologist. Training of personnel cannot be done as a one-time course, but it is necessary to have a theoretical and practical training using models and a period of supervised practice. MASTER PLAN: MATERNAL, NEONATAL AND REPRODUCTIVE HEALTH GROUP 2. LITERATURE-BASED EVIDENCE FOR EFFECTIVE PRACTICES 2.1 Summary of relevant effective practices As part of the process of developing this Master Plan, we conducted a literature review to identify effective practices in the areas of maternal, neonatal and reproductive health (MNRH). In the following tables we present the main effective practices or packages identified in this review, including the type of activities involved, the geographical context in which they have been applied, their target populations, scale of implementation and countries where they have been implemented. This review includes the main practices identified, from which some of them have been selected as a core for this master plan, to be detailed in Section 3. Effective practices are first presented for maternal health, then neonatal health, followed by reproductive health and family planning (RHFP). The categories of effective practices (EP) identified to reduce the main causes of maternal mortality and morbidity at the community and primary care levels were basic Emergency Obstetric Care (EmOC), active management of the third stage of labor (AMSTL), and various practices to prevent and manage eclampsia, postpartum hemorrhage and infection, and complications arising from abortion (Table 2.1.1). We also identified several practices which address issues through community education and involvement. All practices depend on referral to secondary and tertiary care when necessary. Similarly, packages of EPs focused on eliminating or reducing the main causes of neonatal morbidity and mortality, particularly asphyxia, hypothermia and infection (Table 2.1.2). Appendix 3 presents a comprehensive and detailed listing of EPs, which for reasons of space have been grouped into the following packages: essential newborn care, care of the low birth weight (LBW) newborn and care of the newborn with complications. These packages consist of a number of facility-based or clinical interventions and community based actions which, like the maternal EPs depend on coordination with high-level facilities. Finally, effective RHFP interventions for our target population are presented in Table 2.1.3. These consist of implementing quality family planning services for adolescents, ensuring access to counseling and services for at least six different contraceptive methods in health centers, ensuring access to vasectomy and implementing postpartum and post-abortion contraceptive counseling and services. As with maternal and neonatal health EPs, these intervention packages can be designed for community and clinical settings. MASTER PLAN: MATERNAL, NEONATAL AND REPRODUCTIVE HEALTH GROUP . 2.1.1 Maternal health Name of EP or Package of EPs Basic Emergency Obstetric Care (EmOC) Active management of the third stage of labor to prevent postpartum hemorrhage Type of Activity(ies) (e.g., training, service delivery, outreach materials, media campaigns) 1. Train personnel to treat emergencies and to refer more complex problems to secondary and tertiary facilities. Ensure that trained personnel are retained in rural areas and that all new members of health teams are trained. 2. Attend normal vaginal delivery, manual removal of placenta, manual aspiration of placental remains, Tx of severe preeclampsia and eclampsia, administration of oxytocin and antibiotics. 3. All health center and hospital personnel should be trained.in EmOC. This includes doctors (usually interns or general practitioners) nurses, midwives and auxiliary nurses. Improving the skills of personnel attending deliveries has shown to reduce maternal mortality ratios (MMR) in various countries. 4. Training and supervision is crucial because the current quality of services delivered is very low in almost all countries, mainly in rural areas. Training of all personnel attending vaginal deliveries, including doctors, nurses, auxiliary nurses, and midwives.Training TBA’s would be challenging. Geographical Context (e.g., urban, rural) Target Population(s) (e.g., indigenous, poor, other vulnerable) -General -Rural areas are of special concern due to difficulties in access General population with emphasis on primary level services for poor, indigenous and rural populations. -General -Rural areas are of special concern due to difficulties in access Emphasis on public hospitals and clinics that treat the poor. Scale of Implementation (e.g., community, national, regional levels) -National -Methods included in the package may be different in different areas (e.g., urban, rural) -Community (training for emergencies and timely referral) -Hospital -Health center -Community MASTER PLAN: MATERNAL, NEONATAL AND REPRODUCTIVE HEALTH GROUP Country(ies) where Implemented Sources Some experiences in developing countries. 1-7 Almost all countries have had some experience, albeit limited. 8-15 Best practices (interventions) to reduce maternal mortality from acute postpartum vaginal hemorrhage Best practices (interventions) to reduce maternal mortality from eclampsia Best practices (interventions) to reduce maternal mortality from postpartum infection Best practices (interventions) to reduce maternal mortality from septic abortion Community awareness, education and training Ensure the availability of safe blood supply and medications such as Oxytocin and other uterine retractors. Training of all personnel attending vaginal deliveries, including doctors, nurses and midwives, in management and referral. Training of all personnel attending deliveries as well as those providing prenatal care since prevention is so important. Availability of drugs (magnesium sulfate and others). Training of all labor and delivery personnel. Prevention of intrahospital infection. Training of health care providers for management of complications from abortion. Community education for referral of cases. Educating families and community members about danger signs (e.g., preeclampsia) and when/where to refer. Birth preparedness. Training community midwives and traditional birth assistants in the above interventions (e.g., AMTSL, prenatal counseling). -General -Rural areas are of special concern due to difficulties in access Emphasis on public hospitals and clinics that treat the poor. -Isolated studies -Hospital -Health center -Community component poorly evaluated Almost all countries have had some limited experience, 8-10, 16-18 -General -Rural areas are of special concern due to difficulties in access Of the few existing studies, the focus has been on hospitals that treat the poor. Small-scale implementation without systematic expansion. Some experiences in all countries. 8-9, 19-26 -General -Rural areas are of special concern (birth center\s) -Women giving birth at home -Rural populations -Community -Health centers Some isolated experiences in all countries. 8-10, 26-31 Some improvement attempts in metropolitan areas. Focus on the poor, who are affected the most by unsafe abortion. Some isolated experiences in all countries. 32-33 Rural -Women giving birth at home -Rural populations -Community -Household -Household/ hospital continuum of care MASTER PLAN: MATERNAL, NEONATAL AND REPRODUCTIVE HEALTH GROUP General 8, 34-36 1. UNICEF, Guidelines for monitoring the availability and use of obstetric services. New Cork. UNICEF; 1997. 2. Koblinsky M, editor. Reducing maternal mortality: learning from Bolivia, China, Egypt, Honduras, Indonesia, Jamaica, and Zimbabwe. Health, nutrition and population series, Washington (DC): World Bank, 2003. 3. Pathmanathan I, Liljestrand J, Martins J, Rajapaksa L, Lissner C, de Silva A, et al. Investing in maternal health: learning from Malaysia and Sri-Lanka. Health, nutrition and population series. Washington (DC): World Bank; 2003. 4. Ronsmans C, Etard J-F, Walraven G, Hoj L, Dumont A, de Bernis L, Maternal mortality and access to obstetric services in West Africa. Trop Med Int Health 2003;8:940-8. 5. Miller S, Cordero M, Coleman A, Figueroa J, Brito-Anderson R, Dabagh R, et al. Quality of care in institutional deliveries: the paradox of the Dominican Republic. Int J Gynecol Obstet 2003;82:89-103. 6. Ronsmans C, Vanneste A, Chakraborty J, van Ginneken J, Decline in maternal mortality in Matlab, Bangladesh: a cautionary tale. Lancet 1997;350:1810-4. 7. Campbell OM, Graham WJ. Strategies for reducing maternal mortality: getting on with what works. The Lancet Maternal Survival Series steering group. Lancet 2006;368:1284-99. 8. Graham WJ, Cairns J, Bhattacharya S, Bullough CHW, Quayyum Z, Rogo K. Maternal and Perinatal Conditions. 2006. Disease Control Priorities in Developing Countries (2nd Edition) Eds. Jamison DT et al, 499-530. New York: Oxford University Press. 9. Adam T, Lim SS, Mehta S, et al. Cost effectiveness analysis of strategies for maternal and neonatal health in developing countries. BMJ 2005;331:1107. 10. Kestler E., Valencia L., Del Valle V., and Silva A. Scaling Up Post-Abortion Care in Guatemala: Initial Successes at National Level. Reproductive Health Matters 2006;14(27):1-10. 11. Prendiville WJ, Elbourne D, McDonal S. Active versus expectant management in the third stage of labour (Cochrane Review). In: The Cochrane Library, Issue 4, 2002. Oxford: Uptade Software Ltd. 12. Gülmezoglu AM, Villar J, Ngoc NN, Piaggio G, Carroli G, Adetoro L, Abdel-Aleem H, Cheng L, Hofmeyr GJ, Lumbiganon P, Unger C, Prendiville W, Pinol A, Elbourne D, El-Refaey H, Schulz KF, for the WHO Collaborative Group To Evaluate Misoprostol in the Management of the Third Stage of Labour. WHO multicentre double-blind randomized controlled trial to evaluate the use of misoprostol in the management of the third stage of labour. Lancet, 2001;358:689-695. 13. Managing complications in pregnancy and childbirth: A guide for midwives and doctors. World Health Organization, Geneva, 2000 (WHO/RHR/00.7). 14. Biblioteca de Salud Reproductiva N° 10. Información sobre las mejores prácticas en salud reproductiva. Organización Mundial de la Salud 2007. ISSN 1745-9923. Publicado por UPDATE Software. Summertown Pavilon, Middle Way, Oxford OX27LG, United Kingdom. 15. Instituto Biológico Argentino, Buenos Aires, Argentina. 16. Mousa, HA, Alfirevic, Z. Treatment for primary postpartum haemorrhage (Cochrane Review). Cohchrane Database Syst Rev 2003;CD003249. 17. Lu, MC, Fridman, M, Korst, LM, et al. Variation in the incidence of postpartum hemorrhage across hospitals in California. Maternal Child Health J 2005; 9:297. 18. Munn, MB. Owen, J. Vicent R. et al Comparison of two oxytocin regimens to prevent uterine atony at cesarean delivery: a randomized controlled trial. Obstet Gynecol 2001;98:386. 19. Douglas, KA., Redman, CW. Eclampsia in the United Kingdom. BMJ 1994;309:1395 20. Tuffnell, Dj., Jankowicz, D., Lindow, SW, et al. Outcomes of severe pre-eclampsia/eclampsia in Yorkshire 1999/2003. BJOG 2005;112:875 21. Zwart, JJ., Richters, A, Ory, F, et al. Eclampsia in the Netherlands. Obstet Gynecol 2008;112:820. 22. Geographic variation in the incidence of hypertension in pregnancy. World Health Organization International Collaborative Study of Hypertensive Disorders of Pregnancy. Am J Obstet Gynecol 1988;158:80. MASTER PLAN: MATERNAL, NEONATAL AND REPRODUCTIVE HEALTH GROUP 23. Which anticonvulsant for women with eclampsia? Evidence from the Collaborative Eclampsia Trial. Lancet 1995;345:1455. 24. American College of Obetetricians and Gynecologist. Diagnosis and management of preeclampsia and eclampsia. ACOG practice Bulletin #33. American College of Obstetricians and Gynecologists, 2002. 25. Sibai, BM. Magnesium sulfate prophylaxis in preeclampsia: Lessons learned from recent trials. Am J Obstet Gynecol 2004; 190:1520. 26. Darstadt DL, Bhutta ZA, Cousens S, Adam T, Walker N, de Bernis L, for the Lancet Neonatal Survival Team. Evidence-based, cost-effective interventions: how many newborn babies can we save? Lancet 2005;365:977-88. 27. Adair, FL. The American Comité of Maternal Welfare, Inc: Chairman’s Ardes. Am J Obstet Gynecol 1935;30:868. 28. Filker, R., Monif, G. The significance of temperature during the first 24 hours postpartum. Obstet Gynecol 1979;53:358. 29. diZerega , G, Yonekura, L, Roy, S, et al. A comparison of clindamycin-getamicin and penicillingentamicin in the treatment of post cesarean section endomyometritis. Am J Obstet Gynecol 1979;134:238 30. Gibbs, RS, Blanco, JD, Castaneda, YS, St Clair, PJ. A double-blind randomized comparison of clindamycin-gentmicin versus cefamandole for treatment of post-cesarean section endomyometritis. Am J Obstet Gynecol 1982;144:261 31. Frenc, LM, Samill, FM Antibiotics regimens for endometritis after delivery. Cochrane Database Syst Rev 2004; CD001067. 32. Forma, F. Gulmezoglu, AM. Surgical procedures to evacuate incomplete abortion. Cochrane Database Syst Rev 2001;CD001993 33. Grimes, DA. Unsafe abortion: the silent scourge. Br Med Bull 2003;67:99. 34. Household-to-Hospital Continuum of Maternal and Newborn Care, ACCESS, October 2005. 35. Home and Community-Based Health Care for Mothers and Newborns, ACCESS, September 2006. 36. Koblinsky, Marge. Essential Obstetric Care and Subsets. Basic and Emergency Obstetric Care: What's the Difference. MotherCare Policy Brief #1. Arlington, VA: John Snow, Inc., 1999. MASTER PLAN: MATERNAL, NEONATAL AND REPRODUCTIVE HEALTH GROUP 2.1.2 Neonatal health Name of EP or Package of EPs Type of Activity(ies) (e.g., training, service delivery, outreach materials, media campaigns) Guidelines for home births and for the continuum of care between home and hospital to prevent and manage birth asphyxia, infections, and hypothermia. Essential activities under: -Immediate newborn care -Helping newborn breathe -Helping LBW newborn -Helping sick newborn -Stabilizing on way to referral site Recommended essential skills for birth asphyxia, infections, and hypothermia at peripheral facilities. Management of birth asphyxia via community midwife and community health worker (CHW) training. -Essential steps for newborn care antenatal, delivery and postpartum. -Linking the community to facilities and creating an enabling environment. Training of community midwives, village health workers and traditional birth attendants in various resuscitation methods for babies born at home. Tetanus immunization campaign using female vaccinators combined with community and partner support. Door-to-door campaign with female vaccinators and support from fathers, husbands, community leaders and influential community members. Formative research results were used to inform strategies for behavior change communication and social mobilization to help generate demand among at-risk women. Home-based model in which CHWs monitor, identify, treat and refer newborns with sepsis. One intervention provides neonatal care in the home and includes intensive training and supervision with key surveillance, home visit, diagnosis, referral, and sepsis Tx activities performed by CHWs and TBAs. Another trained female community health volunteers to counsel mothers on Target Population(s) (e.g., indigenous, poor, other vulnerable) Scale of Implementation (e.g., community, national, regional levels) Home birth, with family, TBA/CHW or skilled attendant General Geographical Context (e.g., urban, rural) Country(ies) where Implemented Sources -Household -Community -Household/ hospital continuum of care General guidelines 1,2 All -Household within the community -Type I and II level facilities -District hospital General guidelines 1, 3-5 Rural areas. Poor population. Community -Indonesia -Mali 6, 7 2 randomly selected districts At-risk women Community Pakistan 8, 9 Rural (India) Communities where births take place in the home. -Household -Community -India -Nepal General MASTER PLAN: MATERNAL, NEONATAL AND REPRODUCTIVE HEALTH GROUP 10, 11 Traditional birth attendants (TBAs) trained and issued safe delivery kits to reduce perinatal mortality from all causes including sepsis. newborn danger signs, use pictorial algorithms to identify probable serious bacterial infections, provide Tx, and refer to peripheral health workers for Tx. TBAs trained and issued delivery kits; Lady Health Workers linked TBAs with established services and documented processes and outcomes; and obstetrical teams provided outreach clinics for antenatal care. Seven sub-districts (3 intervention, 4 control) of a rural district Population with poor access to health services. -Community -Household/ health center continuum of care Pakistan 12 Community-based and primary care management of neonatal infections. Community-based management of infections: Tx of infections with antibiotics in the home and first level facilities. All types of communities/ homes, but several studies in rural areas. Families with newborns affected by sepsis, meningitis, or pneumonia in low-resource settings. -Household -Community -1st level facility -Bangladesh -India -Guatemala -Nepal -Pakistan 13–15 CHWs trained in communitybased universal skin-to-skin care to reduce neonatal mortality from causes including infections and hypothermia. Promotion of community-based universal skin-to-skin care which reaches all newborns regardless of their birth weight. One study combined a set of ideal practices, with the intervention carried out by CHWs after seven days of training followed by supportive supervision. A randomized control trial promoted universal community KMC as part of essential newborn care taught to pregnant and postpartum mothers by community nutrition workers. Rural areas with high neonatal mortality. -Community stakeholders -Newborns -Pregnant and postpartum mothers -Households with potentially harmful practices Community -India -Bangladesh 16–18 Apply facility-based Kangaroo Mother Care for LBW/ preterm babies to reduce neonatal mortality from complications including infections and hypothermia. What is the evidence that facility-based skin-to-skin care (SSC) (+ breastfeeding) works for LBW newborns? Six studies evaluated the effects of SSC in five areas—mortality, temperature, breastfeeding, weight gain, and infections. n/a n/a Facility n/a MASTER PLAN: MATERNAL, NEONATAL AND REPRODUCTIVE HEALTH GROUP 16 Treatment of neonatal infections in developing countries with oral antibiotics. A review of the evidence for treatment of neonatal infections in developing countries with oral antibiotics, and an evaluation properties of oral agents that could be considered. Simple, culturally relevant messages were developed to reinforce healthy birth preparedness and clean delivery, hygienic umbilical cord care, skin-to-skin care, breastfeeding and keeping the baby warm. CHWs and community volunteers incorporated behavior change messages into traditional folk songs and worked with stakeholders through a home visits and community meetings. The intervention consisted of a package of home-based newborn care (HBNC) activities carried out by project-paid CHWs. One of the activities was to identify pregnant women and make antenatal visits to counsel on healthy behaviors during pregnancy and birth preparedness. Door-to-door campaign with support from fathers, husbands, community leaders and influential community members. Developing country settings with limited health systems capacity. Resource-poor populations. -Facility -Community Developing countries 19 Uttar Pradesh state, where 25% of India’s 1 million annual neonate deaths occur. -Communities where more than 80% of infant deliveries take place in the home and away from the formal health care system. -Pregnant women -Families -Key community members Community India 20 Rural Communities where births take place in the home. -Household -Community India 10, 15 2 randomly selected districts -Fathers -Husbands Community Pakistan Referral system Within a package of essential activities, stabilizing the newborn on way to referral site. General Home birth, with family, TBA/CHW or skilled attendant -Household -Community -Household/ hospital continuum of care Training of mothers, families and CHWs to identify early neonatal warning signs and community referral and/or management The intervention consisted of a package of home-based newborn care (HBNC) activities carried out by project-paid CHWs. One of the activities was to teach families to recognize and seek care for newborn danger signs. Another program trained FCHVs to counsel families on essential newborn care and newborn danger signs. Rural Communities where births take place in the home. -Household -Community Community-based behavior change management through a campaign in which CHWs incorporate messages about healthy and safe delivery practices including hypothermia prevention techniques. Birth preparation Male involvement MASTER PLAN: MATERNAL, NEONATAL AND REPRODUCTIVE HEALTH GROUP 8, 9 1, 2 -India -Nepal 10, 11, 15, 20 1) Household-to-Hospital Continuum of Maternal and Newborn Care, ACCESS, October 2005. 2) Home and Community-Based Health Care for Mothers and Newborns, ACCESS, September 2006. 3) Bringing Care Closer to Mothers and Newborns: Using the GAP to Develop HH Continuum of Care, ACCESS, February 2006. 4) Koblinsky, Marge. Essential Obstetric Care and Subsets. Basic and Emergency Obstetric Care:What's the Difference. MotherCare Policy Brief #1. Arlington, VA: John Snow, Inc., 1999. 5) Beck D., Ganges F, Goldman S, Long P. Care of the Newborn Reference Manual. Saving Newborn Lives/Save the Children Federation. 2004. 6) Reducing Birth Asphyxia through the Bidan di Desa Program in Indonesia, Final Report to Save the Children 2006, PATH. 7) Pilot study of a community-based intervention to reduce neonatal death due to birth asphyxia in the health district of Ouelessebougou, Mali, Proposal to Save the Children, 2007, CREDOS. 8) Rasmussen B, Ali N. Mobilizing demand for maternal and neonatal tetanus immunization: reaching women in Pakistan, S Crump ed. Shaping policy for maternal and newborn health: a compendium of case studies. JHPIEGO Corporation, 2003: 23-28. 9) Krift L, et al. Final program evaluation, Pakistan program. Save the Children Saving Newborn Lives Program, 2005. 10) Bang A, Bang R, Reddy H. Home-based neonatal care: summary and applications of the field trial in rural Gadchiroli, India (1993 to 2003). J Perinatol 2005; 25: S108-S122. 11) Sharma J. Community based management of neonatal infections in Nepal: establishing a model in one district. Morang innovative neonatal intervention program (MINI) final report. Submitted to Save the Children US. John Snow International, 2006. 12) Abdul Hakeem Jokhio, Heather R. Winter, and Kar Keung Cheng. Intervention involving traditional birth attendants and perinatal and maternal mortality in Pakistan. N Engl J Med 2005;352(20):2091-9. 13) Bhutta ZA, Zaidi AK, Thaver D, Humayun Q, Ali S, Darmstadt GL. Management of newborn infections in primary care settings: a review of the evidence and implications for policy? Pediatr Infect Dis J. 2009 Jan;28(1 Suppl):S22-30. 14) Darmstadt GL, Batra M, Zaidi AK. Parenteral antibiotics for the treatment of serious neonatal bacterial infections in developing country settings. Pediatr Infect Dis J. 2009 Jan;28(1 Suppl):S37-42. 15) Community-based management of newborn infections MotherNewborNews Volume 3 No. 1 - 2 July 2007 – December 2008. 16) Community-Based Care for Low Birth Weight Newborns: The Role of Community Skin-to-Skin Care Meeting Report. May 27, 2008 Washington, DC. 17) Darmstadt, GL, et al. Introduction of community-based skin-to-skin care in rural Uttar Pradesh, India. J Perinatol. 2006 Oct;26(10):597-604. Epub 2006 Aug 17. 18) Sloan, L. Nancy et al. Community-based Kangaroo Mother Care to prevent neonatal and infant mortality: a randomized controlled trial. Pediatrics, Volume 121, Number 5, May 2008. 19) Darmstadt GL, Batra M, Zaidi AK. Oral Antibiotics in the Management of Serious Neonatal Bacterial Infections in Developing Country Communities. Pediatr Infect Dis J. 2009 Jan;28(1 Suppl):S31-6. 20) Kumar V, et al. Effect of community-based behaviour change management on neonatal mortality in Shivgarh, Uttar Pradesh, India: a cluster-randomised controlled trial. Lancet. 2008 Sep 27; 372(9644): 115162. MASTER PLAN: MATERNAL, NEONATAL AND REPRODUCTIVE HEALTH GROUP 2.1.3 Reproductive health and family planning Name of EP or Package of EPs Type of Activity(ies) (e.g., training, service delivery, outreach materials, media campaigns) Geographical Context (e.g., urban, rural) Target Population(s) (e.g., indigenous, poor, other vulnerable) Scale of Implementation (e.g., community, national, regional levels) Exclusive services for adolescents are better accepted and used more frequently Implement quality family planning services for adolescents Training providers in sexuality and family planning counseling is essential Wide range of contraceptive options is critical -General -Initially urban Entire adolescent population Services should be oriented to adolescents’ sexual and reproductive rights and needs and should be easy accessible and user friendly. Ensure access to counseling and services for at least six contraceptive methods in health posts Health systems should offer free choice of several methods. Each method added to the available options increases prevalence 12% Training personnel for counseling and delivering at least six methods and referral to surgical methods. Ensure availability of methods (contraceptive security). General General population with emphasis on primary level services for the poor population, adolescent and youths Services for adolescents are recognized as very important but programs have not been expanded. Several models have been tested. National. Methods included in the package may be different in different areas (e.g., urban, rural). Referral to surgical methods should be ensured MASTER PLAN: MATERNAL, NEONATAL AND REPRODUCTIVE HEALTH GROUP Country(ies) where Implemented Sources Many partially evaluated experiences in several countries. Most evaluations refer to how to implement and access. 1-8 No impact results available except from USA, UK, Europe, LAC. All countries have partially implemented programs to offer FP to the entire population. Access to services is very limited in the region 9-12 Ensure access to vasectomy in hospitals and health centers Implement postpartum and postabortion contraceptive counseling and services in all hospitals attending deliveries and abortions Vasectomy has shown to be very effective and well accepted. It is by far the most cost effective method because it is inexpensive, highly effective and long lasting. Contraceptive counseling and services in the post-partum and post-abortion period have shown to be effective in several studies in developing countries, increasing acceptance of effective contraceptive methods. Offered mainly in urban hospitals and health centers Should be implemented in all hospitals and health centers attending deliveries and abortion complications. Several studies, some expanded (Guatemala and Honduras) No national coverage. General. Acceptance has shown to be higher in urban educated men. No reliable data on indigenous population. Entire population with an emphasis on adolescents and youth. Officially approved and included in most FP programs. Access is limited and promotion of use of the method is low in LAC. Acceptance seems to be higher in the postpartum period. Several countries have implemented programs. Population Council has promoted projects in several countries in LAC, Europe and Africa. Guatemala has a structured program covering two thirds of the hospitals, with continual monitoring by a research team. MASTER PLAN: MATERNAL, NEONATAL AND REPRODUCTIVE HEALTH GROUP Partially implemented in most western countries. 13-14 Several countries in all regions including Guatemala have implemented post-partum and postabortion contraceptive services. 15-16 1. Contraception (Issues in adolescent health and development). WHO Discussion Papers on Adolescence. World Health Organization, 2004. 2. Sabonge K; Wulf D; Remez L; Prada E; Drescher J. Early childbearing in Honduras: a continuing challenge. Issues Brief (Alan Guttmacher Inst). 2006 Sep; (4):1-23. 3. Figueroa W, Lopez F, Remez L, Prada E, Drescher J. Early childbearing in Guatemala: a continuing challenge. Issues Brief (Alan Guttmacher Inst). 2006 Sep; (5):1-20. 4. Blandón L, Carballo Palma L, Wulf D, Remez L, Prada E, Drescher J. Early childbearing in Nicaragua: a continuing challenge. Issues Brief (Alan Guttmacher Inst). 2006 Sep; (3):1-24. 5. Kirby D (2001). Emerging Answers – Research findings on programs to reduce teen pregnancy. Washington, DC: The National Campaign to Prevent Teen Pregnancy. 2001. 6. Kirby D (2001). Understanding What Works and What Doesn’t in Reducing Adolescent Sexual RiskTaking. Fam Plann Perspect, 33(6):276–281. 2001. 7. Kilbourne-Brook M (1998) Adolescent Reproductive Health: Making a Difference. Outlook, 16(3):1–8. 8. Family Health International Network (2000). Adolescent Reproductive Health, 20(3):1–36. 9. Sullivan TM, Bertrand JT, Rice J, Shelton JD. Skewed contraceptive method mix: why it happens, why it matters. J Biosoc Sci. 2006 Jul;38(4):501-21. 10. Kayembe PK, Fatuma AB, Mapatano MA, Mambu T. Prevalence and determinants of the use of modern contraceptive methods in Kinshasa, Democratic Republic of Congo. Contraception 2006 Nov;74(5):400-6. 11. Lapham RJ and Mauldin WP. Contraceptive prevalence: the influence of organized family planning programs. Studies in Family Planning, 1985 May-Jun;16(3):117-37. 12. Jain AK. Fertility reduction and the quality of family planning services. Studies in Family Planning, 1989 Jan-Feb;20(1):1-16. 13. Frontiers in Reproductive Health (FRONTIERS), Population Council, Washington, DC. Available at: http://www.popcouncil.org/frontiers/ 14. De Rodriguez B, Vernon R, Solorzano J. Expanding Access to Vasectomy Services in the Ministry of Health of Guatemala. Final Report. Population Council/FRONTIERS, November 2005. 15. Kestler E, Valencia L, Del Valle V, Silva A. Scaling up post-abortion care in Guatemala: initial successes at national level. Reproductive Health Matters 2006;14(27):138–147. 16. Postabortion Care. Population http://www.popcouncil.org/rh/pac.html. 2.2 Council, Washington, DC. Available at: Outcomes, impacts, and cost effectiveness of relevant effective practices After conducting the literature review presented in the previous section, we identified the main outcomes (short or intermediate term) and long term impacts of each effective practice identified. We also identified information on the cost effectiveness of those practices; the most pertinent information is presented in the following tables. High coverage of the most cost-effective interventions depending on a country’s level of resources is the preferred approach (Adam et al 2005). However, cost-effectiveness data for interventions specifically carried out in Central America or the Latin American and Caribbean region is severely lacking. Thus when cost-effectiveness evidence was unavailable for the proposed EPs we refer to the WHO-CHOICE estimates for Mesoamerican countries. The first group known as AMRO-D (defined as having high child and adult mortality) includes Guatemala and Nicaragua. The rest of the Mesoamerican countries form part of the second group classified as AMRO-B (low child and adult mortality). WHO-CHOICE has carried out the exercise of estimating the cost-effectiveness of hundreds of maternal and neonatal packages for all regions including AMRO-B and AMRO-D, which should prove a useful tool for Mesoamerican countries when setting priorities and choosing intervention packages. The Disease Control Priorities project MASTER PLAN: MATERNAL, NEONATAL AND REPRODUCTIVE HEALTH GROUP is also a good source for cost-effectiveness estimates in MNRH in developing countries (see Graham et al. 2006, Lawn et al. 2006, Levine et al. 2006, and Lule et al. 2006). Some main findings are highlighted below. For maternal health (Table 2.2.1), increasing the number of births attended by skilled personnel will have an immediate impact on maternal mortality, especially in those countries with higher MMR. The implementation of a good referral system, backed by adequate transportation, reducing the delays in transporting patients to centers with more resources will have a great impact on MM for direct causes. Long term impact on indicators will depend upon the sustainability of the interventions, mainly in rural areas. Clearly many maternal and neonatal health interventions can be grouped together, thus resulting in even higher cost-effectiveness. An analysis of hundreds of maternal-newborn packages in high child/high mortality countries in sub-Saharan Africa and Southeast Asia found that the most costeffective packages were the following: interventions for newborn care at the community level (e.g., promotion of breast feeding), followed by selected antenatal care interventions (e.g., tetanus toxoid), interventions deliverable by a skilled attendant at birth in a health facility (e.g., normal delivery care by a skilled attendant), then by more complex interventions that require referral to a higher level health facility (Adam et al 2005). Infant mortality has decreased significantly in the entire region but neonatal mortality has decreased at a slower pace. Improving access to emergency care to newborns, especially in rural areas, will have an immediate impact on neonatal mortality if proper attendance to asphyxia and warming is implemented in birth attendance at the primary level, including home deliveries (Table 2.2.2, refer to Appendix 3 for a detailed listing of intervention package outcomes and impacts). Although cost-effectiveness data is mainly reported in studies from developed countries, in some cases interventions in other low-and-middle-income countries provide information for neonatal health programs. A recent examination of evidence-based interventions to reduce neonatal mortality in developing countries shows that compared with single interventions, packages of interventions are always more cost-effective, and much of the benefit is derived from communitylevel actions (Darmstadt et al 2005). Furthermore, settings with very high neonatal mortality see the greatest benefits from implementing these types of intervention packages. The improvement of access and quality of family planning services will have important short and long term impact on women’s and children’s health by reducing unwanted pregnancies and unsafe abortions. The impacts are still greater in adolescents because delaying the first pregnancy has positive effects on women, reducing high risk pregnancies, increasing access to education and improving their livelihoods. The expansion of the use of vasectomy in the region may greatly contribute to decrease fertility rates (Table 2.2.3). Contraception cost savings and cost-effectiveness estimates are often based on studies from the United States and Europe (Trussell 2007; Armstrong and Donaldson 2005; McGuire and Hughes 1995). However, the data consistently show that contraception is always cost-effective compared to no contraception (Mavranezouli 2009). Even the most conservative studies show an average of four dollars saved for each dollar spent on contraception (Foster et al 2009). Furthermore, long acting methods are the most cost-effective since the cost of delivering the contraceptive is almost negligible compared to the savings from avoiding a pregnancy. More effective methods (i.e., implants, long-acting injectables, IUD) are by far the more cost-effective (Trussell et al 1995). Thus, despite the lack of regional data, based on the literature all family planning interventions proposed are highly cost-effective. MASTER PLAN: MATERNAL, NEONATAL AND REPRODUCTIVE HEALTH GROUP 2.2.1 Maternal health Name of EP or Package of EPs Short-Term or Intermediate Outcomes Long-Term Impacts Cost Effectiveness Expensive and highly cost effective. Basic Emergency Obstetric Care (EmOC) -Increased number of basic EmOC services. -Increased number of deliveries attended by trained personnel. -Reduction in maternal morbidity. -Better referral systems to resolve highcomplexity cases. . Effectiveness widely demonstrated. The greatest cost is associated with personnel training and a factor that increases this cost in the region is the high turnover of medical personnel. All new members of health teams have to be trained and old ones should be supervised periodically. Costs will also increase with the implementation of supervision, monitoring and evaluation systems. -Reduced maternal mortality ratios. -Reduction in morbidity and direct causes of mortality. Evidence from South Asia and Sub-Reduce secondary mortality caused by Saharan Africa: Improvements in the obstetric complications by 50%.6 overall quality of care, especially at the primary level through the provision of BEmOC together with increased overall coverage are the most cost-effective intervention packages—and both include nutritional supplements. They are followed by increased coverage at the primary level. Improved quality of comprehensive EmOC is the least costeffective option (8). South Asia -Improved BEmOC ICER (Int$ per DALY averted 142) MASTER PLAN: MATERNAL, NEONATAL AND REPRODUCTIVE HEALTH GROUP -Improved BEmOC + coverage ICER (Int$ per DALY averted 144) Active management of the third stage of labor to prevent postpartum hemorrhage Best practices (interventions) to reduce maternal mortality from acute immediate postpartum vaginal hemorrhage -Increased number of personnel trained in the active management of the third stage of labor. -Increased number of deliveries with active management of the third stage of labor, as a percentage of all vaginal deliveries. -Fewer cases of moderate postpartum hemorrhage (> 500 ml.) -Fewer cases of severe postpartum hemorrhage (> 1000 ml.) . -Reduction in morbidity and direct causes of mortality. -Reduce the number of maternal deaths due to postpartum hemorrhage. -Reduced risk of postpartum hemorrhage > 500 ml of 0.38 (95% C.I. 0.32 – 0.46).11 Sub-Saharan Africa -Improved BEmOC ICER (Int$ per DALY averted 83) -Improved BEmOC + coverage ICER (Int$ per DALY averted 86) Complements above packages. Training of personnel is the most expensive component. The drugs are inexpensive but the guaranteed availability of Oxytocin requires a logistics system. The following package in most of Mesoamerica with 95% coverage, has ACER (Int$ per DALY averted 149.4): Community newborn care package (support for breastfeeding, support for low birth weight) + ANC+SMNC (skilled maternal and newborn care)+treatment of severe PEE+PPH (post partum -Increased number of personnel trained to hemorrhage) referral+community based manage hemorrhage complications and who pneumonia+maternal sepsis+ENC know when to refer patients to better-equipped (essential preventive care and facilities. -Reduction in morbidity and direct recognition of danger signs and referral). -Fewer cases of moderate postpartum causes of mortality. In Guatemala and Nicaragua, the same hemorrhage (> 500 ml.) -Reduce the risk of acute postpartum package is even more cost-effective: -Fewer cases of severe postpartum hemorrhage hemorrhage by 80%. (> 1000 ml.) -Reduce the number of maternal deaths ACER (Int$ per DALY averted 38): -Increased number of cases transferred to higher- due to postpartum hemorrhage. Management of hemorrhage as part of a level facilities opportunely. Women should be package, with 80% coverage in Bolivia, transferred opportunely and receiving Ecuador, Guatemala, Haití, Nicaragua y endovenous volume reposition. Perú: Community Newborn Care -Increased number of blood transfusions. Package (promotion of extra warmth for low birthweight babies and support to breastfeeding) + ANC (Primery level MASTER PLAN: MATERNAL, NEONATAL AND REPRODUCTIVE HEALTH GROUP Best practices (interventions) to reduce maternal mortality from eclampsia -Increased number of personnel trained to detect cases of pre-eclampsia early. -Increased availability of drugs. -Increased availability and use of protocols. -Increased number of cases treated for eclampsia. -Increased number of cases referred to higherlevel facilities and to ICU. -Reduce the number of convulsions through treatment with magnesium sulfate by half (RR 0.44, 95% CI 0.32-0.51)25 care, Skilled maternal care, initial management of post-partum hemorrhage) ACER (Int$ per DALY averted) $11 Prenatal care is an important component of this set of interventions as early detection of high-risk cases is crucial in order to have an impact. The same considerations regarding personnel training and turnover apply. -Reduction in morbidity and direct causes of mortality. -Reduce the maternal mortality rate by one third (RR 0.62, 95% CI 0.39-0.99)25 Two very similar MCH packages (MNH268 and MNH-277) that include prevention and management of eclampsia in Mesoamerica, with 95% coverage, in terms of ACERs were Int$76 per DALY averted and Int$65.4 per DALY averted In Guatemala and Nicaragua, the same packages are Int$27 per DALY averted and Int$31 per DALY averted). The cost of these interventions comes from the use of highly effective but expensive antibiotics. Training-related considerations apply as well. Best practices (interventions) to reduce maternal mortality from postpartum infection -Greater number of hospitals with personnel trained to prevent and treat postpartum infections. -Increased availability of highly effective antibiotics.- Increased number of cases treated for postpartum infection. -Increased number of cases of postpartum infection referred to a higherlevel facility. -Reduction in morbidity and direct causes of mortality. -Reduce postpartum infection morbidity by 75%. MASTER PLAN: MATERNAL, NEONATAL AND REPRODUCTIVE HEALTH GROUP Management of postpartum infection included in the following package: Management of maternal sepsis (including treatment with intravenous or intramuscular antibiotics) (95% coverage) Africa East: Int$34 per DALY averted Southeast region: Int$21 per DALY averted -Antibiotics for preterm premature rupture of membranes (95%) ACER(Int$ per DALY averted 35) -Higher level of education among the general population to avoid dangerous operations resulting in fewer unsafe abortions. -Increased number of personnel trained to treat Best practices unsafe abortion complications, especially (interventions) to infections. reduce maternal -Increased availability of antibiotics and medical mortality from septic teams prepared to carry out intensive treatments. abortion -Increased number of cases treated for septic abortion. -Increased number of cases of septic abortion referred to higher-level facilities. -Increased number of women referred to primary level health facilities. -Increased number of women referred to higherCommunity level facilities. awareness, education -Higher level of education among the general and training population to avoid dangerous operations resulting in fewer unsafe abortions. -Traditional birth attendants better equipped to to prevent and manage complications. -Reduction in morbidity and direct causes of mortality. -Decrease the number of cases of septic abortion by 80%. Training personnel to treat abortion complications can be expensive. Training for all referral-related actions must also be taken into account. There is no cost-effectiveness evidence. -Reduction in morbidity and mortality from eclampsia, septic abortion, hemorrhage and infection. MASTER PLAN: MATERNAL, NEONATAL AND REPRODUCTIVE HEALTH GROUP Low complexity, community level interventions are the most cost-effective. 2.2.2 Neonatal health Name of EP or Package of EPs Short-Term or Intermediate Outcomes Increased number of trained TBAs and medical personnel. Essential Newborn Care Package Reduction of the risk of infections, asphyxia and hypothermia. Neonatal Resuscitation Reduction of the incidence of other conditions and complications from these conditions, such as: coagulation defects, acidosis, delayed fetal-to-newborn circulation adjustment, hyaline membrane disease and brain hemorrhage due to hypothermia, hypoglycemia, necrotizing enterocolitis, omphalitis, acute respiratory infections, diarrhea, septicemia, and neonatal conjunctivitis. The Clean Chain The Warm Chain Breastfeeding Cord, Eye and Skin Care Immunization Vitamin K Prevention of perinatal and early horizontal transmission of HBV. Long-Term Impacts Reduction in asphyxia-related deaths and mortality. Reduction in infection-related deaths and mortality. Reduction in hypothermia-related deaths and mortality. Reduction in intensive care hospitalization, disability, rehabilitation and physical therapy costs. Polio immunization costs US $20 per disability-adjusted lifeyear averted. Benefits in infant and child health and development. The estimated cost of routine hepatitis B vaccination was US $28 per disability-adjusted life year averted. Benefits adult health (decreased risk of liver disease due to Hep B vaccine, avoid disability). Reduce neonatal deaths among LBW babies. Identification of the LBW Baby Increase in referral of babies weighing less than 1,800 g to more specialized health care units. Reduction in NMR as a result of prevention of neonatal cold injury. Improvement in weight gain and growth Reduce disability due to preterm asphyxia, hemorrhagic disease and other neonatal complications among LBW newborns. Extra support for Warmth More efficient treatment of life threatening preterm-related diseases (respiratory distress syndrome, hemodinamically significant patent The bag-and-mask was $13 per averted death. Reductions in NMR and PMR. Increased number of TBAs/CHWs/ health providers trained in LBW baby identification. Extra Support for Feeding $0.25 per birth covered, $42 per asphyxia death averted. Eye prophylaxis costs US $ 1.40 per case averted when the rate of gonococcal infection is greater than ten percent. Reduction in hemorrhage-related neonatal mortality. Low Birth Weight Baby Package Extra Clinical Care of the LBW Baby Cost Effectiveness Reduction in hemorrhage-related NMR. Vitamin K injection costs US $52 per disability-adjusted life-year averted in areas of high incidence of LBW (more than 72 per 100,000 births). Oral Vitamin K is widely used in Europe and is considerably less expensive, but the efficacy of oral administration needs additional investigation. MASTER PLAN: MATERNAL, NEONATAL AND REPRODUCTIVE HEALTH GROUP Vitamin K duct arterious and necrotizing enterocolitis). Reduction in hypothermia damage, respiratory distress syndrome, hypoglycemia, diarrhea jaundice, sepsis, feeding-related asphyxia, and other morbidities. Reduction in the risk of acute otitis, severe lower respiratory tract infections and atopic dermatitis, sudden death syndrome and necrotizing enterocolitis, nosocomial infection, severe illness and lower respiratory tract disease. Emergency Care of Newborns with Complications Identification of Neonatal Danger Signs Quality Emergency Care of the Sick Newborn Interventions to treat: Severe Neonatal Infection Neonatal Tetanus Neonatal Asphyxia Neonatal Jaundice Birth Defects Severe Bleeding Uptake of antenatal and delivery services, home care practices, and health-care seeking. Improve key newborn care practices. Reduction in neonatal morbidity: sepsis, meningitis, pneumonia, asphyxia. hyperbilirubinemia Reduced neonatal bilirubin levels. Decrease in the risk of hypovolemic/hypoxic shock. Reduction in oxygen requirements due to acute anemia, restitution of intravascular volume, improvements in hemodynamics, decrease heart rate and cardiac output, improve growth parameters, decrease lactate levels, or decrease apneic episodes in stable premature infants. Reduction in time of hospital stay, intensive care hospitalization, and treatment costs. Reduction in costs from hospital stays, treatment, disability, rehabilitation and physical therapy. Reduction in the risk of asthma (young children), obesity, type 1 and 2 diabetes, and childhood leukemia. Reduce neonatal mortality. Reduce neonatal mortality due to sepsis, pneumonia, tetanus. Reduce disability, rehabilitation and physical therapy costs. Reduction in aesthetic and functional problems such as difficulties originated by cleft lip and palate (i.e., swallowing). Improvement in neurological outcomes of asphyxiated infants. Reduction in disability rehabilitation and physical therapy needs.13 See WHO-CHOICE maternal and neonatal intervention packages for regions AMRO-B and AMRO-D. Reduction in the risk of sensory neural hypoacusia prevalence. Reduction in choroathetoid cerebral palsy prevalence. Improved long term survival from Myelomeningocele. MASTER PLAN: MATERNAL, NEONATAL AND REPRODUCTIVE HEALTH GROUP 2.2.3 Reproductive health and family planning Name of EP or Package of EPs Implement quality family planning services for adolescents Ensure access to counseling and services for at least six contraceptive methods in health posts Short-Term or Intermediate Outcomes Greater use of reproductive health services. Increased number of new acceptors of contraceptives. Greater male participation in contraception. Reduction of gender imbalance. Increase the number of new acceptors of contraceptive methods. Increase user satisfaction and continuation rates. Change in method mix. Ensure access to vasectomy in hospitals and health centers Increased number of acceptors of vasectomy. Greater participation of men in FP. Implement postpartum and postabortion contraceptive counseling and services in all hospitals attending deliveries and abortions Increase prevalence of contraceptive use after deliveries and abortions. Long-Term Impacts Increased contraceptive use in adolescents. Reduced number of adolescent pregnancies. Reduction of unsafe abortions. Increased prevalence of modern contraceptive methods and decrease in traditional methods. Decrease in contraceptive unmet need. Improved contraceptive mix. Decreased number of unwanted pregnancies. Decreased abortion rates. Reduction of neonatal and maternal mortality. Increased intergestational intervals. Increased prevalence of IUD use. Reduction of maternal and neonatal mortality. MASTER PLAN: MATERNAL, NEONATAL AND REPRODUCTIVE HEALTH GROUP Cost Effectiveness Expensive and highly cost effective Highly cost effective Very inexpensive, the most cost effective program. Inexpensive and highly cost effective. 3. POSSIBLE SOLUTIONS: SELECTION OF EFFECTIVE PRACTICES FOR REGIONAL IMPLEMENTATION The next step in the development of this Master Plan was the identification of a group of the most effective practices, which in turn compose the proposals for solutions of identified problems. These interventions have been discussed at length with the working groups and country representatives. We are aware of the importance of aligning the proposed interventions with the ones proposed by other foundations or organizations that do substantive work in this area, specifically the Bill and Melinda Gates Foundation. The following tables present the main packages of interventions proposed for each area, describing the process of implementation of each practice or package and the factors necessary to achieve sustainability after the MHI ends. 3.1 Maternal health Effective Practices (EP) or Package of EPs Implementation Process To implement this intervention, it is necessary to train personnel to treat emergencies and to refer more complex problems to secondary and tertiary level facilities. The intervention has emphasis on primary level services for poor, indigenous and rural populations. It aims that all health centers and hospitals should have all personnel trained.in EmOC, including doctors (usually interns or general practitioners) nurses, midwives and auxiliary nurses. Training and supervision is crucial. Basic Emergency Obstetric Care (EmOC) Drugs Oxytocin Antibiotics Magnesium sulfate Misoprostol Procedures Attendance of normal vaginal delivery, Manual removal of placenta, Manual aspiration of placental remains, Treatment of severe pre-eclampsia and eclampsia Administration of oxytocin and antibiotics. Sustainability Political commitment. Supervision and monitoring processes with weekly evaluations of sets of indicators. Dissemination plans for EmOC guidelines and protocols. More ob-gyn specialists. Appropriate infrastructure for medication storage. Regional cooperation and economic support from donors. Human resources In the community: physicians, nurses, midwives In hospital: physicians, nurses Active management of the third stage of labor to prevent postpartum hemorrhage The implementation of this intervention includes an initial phase of training of all personnel attending vaginal deliveries, including doctors, nurses, auxiliary nurses, and midwives. Drugs Oxytocin Political commitment. Supervision and monitoring processes with weekly evaluations of sets of indicators. Trained personnel. MASTER PLAN: MATERNAL, NEONATAL AND REPRODUCTIVE HEALTH GROUP Procedures -Training of personnel -Use of uterotonics (oxytocin) -Immediate cord clamping -Assistance delivering the placenta with controlled cord traction Human resources In the community: physicians, nurses, midwives In hospital: physicians, nurses Other requirements In hospital: Update and disseminate guidelines The implementation of this intervention includes training of all personnel attending vaginal deliveries, including doctors, nurses and midwives, in management and referral. For its operation, it is necessary to ensure the availability of safe blood supply and medications such as Oxytocin and other uterine retractors. Drugs Oxytocin Best practices (interventions) to reduce maternal mortality from acute immediate postpartum vaginal hemorrhage Procedures Primary intervention components: -Coordination with others -Uterine massage -Administration of uterotonics (including misoprostol) -IV and blood transfusion -Catheter Secondary intervention components: -Examination of birth canal -Hysterectomy Human resources In hospital: physicians, nurses In the community: physicians, nurses, midwives Political commitment. Supervision and monitoring processes with weekly evaluations of sets of indicators. Better monitoring of neonatal and maternal mortality Installation and accreditation of blood banks to ensure the supply of safe blood. Strengthening training, monitoring and supervision of TBA’s, midwives and general practitioners. Legal advocacy. Other requirements In hospital: Update and disseminate guidelines. In the community: Necessity of reliable blood banks. Best practices (interventions) to reduce maternal mortality from eclampsia This intervention requires training of all personnel attending deliveries as well as those providing prenatal care since prevention is so important, and availability of drugs (magnesium sulfate and others). Drugs - Labetalol -Hidralazina Improved prenatal care. Improved quality of care. Procedures -Prevention of maternal hypoxy (oxygen mask) -Drug-based management of severe arterial hypertension MASTER PLAN: MATERNAL, NEONATAL AND REPRODUCTIVE HEALTH GROUP -Drug-based prevention of recurring convulsions -Evaluate uterus evacuation Human resources In hospital: physicians, nurses In the community: physicians, nurses, midwives Other requirements In hospital: Ongoing training of medical and nursing personnel. Its implementation requires training of all labor and delivery personnel. Drugs -Clindamycin -Getamicin Best practices (interventions) to reduce maternal mortality from postpartum infection Procedures -Administration of drugs including Clindamycin, Getamicin -Clinical observation -Evaluation of endouterine aspiration of placenta remains Ongoing training of health personnel in the proper management and importance of clean deliveries. Human resources In hospital: physicians, nurses In the community: physicians, nurses, midwives Other requirements In hospital: Update and disseminate postpartum guidelines and norms. The implementation of this intervention involves 2 main activities: training of health care providers for management of complications from abortion, and community education for referral of cases. Drugs Clindamycin Getamicin Best practices (interventions) to reduce maternal mortality from septic abortion Procedures -Patient stabilization -Blood and/or placenta analysis -Administration of antibiotics - Evaluation of endouterine aspiration of placenta remains -Post abortion counseling and contraception Develop a post-abortion care plan. Technical assistance from international organizations DAIA, political will. Application of laws and guidelines Human resources In the community: physicians, nurses, midwives In hospital: physicians, nurses Other requirements In the community: Systematic promotion of contraceptive methods, investigate clandestine abortions In hospital: . MASTER PLAN: MATERNAL, NEONATAL AND REPRODUCTIVE HEALTH GROUP This intervention consists in educating families and community members about danger signs (e.g., preeclampsia) and when/where to refer. Includes also training community midwives and traditional birth assistants in the above interventions (e.g., active management of the third stage of labor, prenatal counseling). Community awareness, education and training Procedures Training of TBA’s and community midwives in essential obstetric care. Components of preventing delays: ANC counseling, community mobilization activities on birth planning, recognition of danger signs, emergency first aid, emergency planning for referral (money, transportation, etc). Community awareness of the problem Involvement of rural and indigenous communities Components of preventing infection: clean delivery place, hands, cord cutting, etc. MASTER PLAN: MATERNAL, NEONATAL AND REPRODUCTIVE HEALTH GROUP 3.2 Neonatal health Effective Practices (EP) or packages of EPs Essential Newborn Care Intervention Package Implementation Process Drugs Vitamin K (1mg) Tetracycline solution (1%) or Erythromycin (0.5%) BCG vaccine Polio vaccine HBV vaccine Procedures Neonatal Resuscitation (Advanced if needed) Clean and warm chain application Promote breastfeeding/Mother training Eye prophylaxis care After delivery vaccination Vitamin K administration Human resources In hospital: Enough physicians and nurses addressed to newborn care exclusively In the community: One trained TBA/CHW/health provider/physician/nurse per delivery to achieve good outcomes even if are facing up a multiple delivery. TBA’s/CHW/health provider should seek for help in these case if possible Sustainability Political commitment. Supervision and monitoring processes with weekly evaluations of sets of indicators. Dissemination plans for essential newborn care guidelines and protocols. Guarantee TBA’s/ CHW’s/health providers training al newborn care interventions above all neonatal resuscitation Establish a Perinatal Epidemiology Surveillance System locally to address Fetal and Neonatal Mortality based on BABIES Matrix (birth weight and age at death boxes for intervention and evaluation system) (1). More pediatrics and neonatology specialists. Appropriate infrastructure for medication storage and distribution and to keep drugs availability Regional cooperation and economic support from donors. Other requirements Basic equipment: Dry clean cloth Bag and mask Suction apparatus Gloves Shelf to put the baby on Method to keep the baby warm (overhead light bulbs) Oxygen supply if possible Extra Care for LBW babies Drugs Oxygen Vitamin K (0.5mg) Tetracycline solution (1%) or Erythromycin (0.5%) 10% Dextrose solution BCG vaccine Polio vaccine Political commitment. Supervision and monitoring processes with weekly evaluations of sets of indicators. Dissemination plans for extra care for LBW babies and emergency newborn care guidelines and protocols. Establish a Perinatal Epidemiology MASTER PLAN: MATERNAL, NEONATAL AND REPRODUCTIVE HEALTH GROUP HBV vaccine Procedures Identification of the LBW baby After that basic procedures plus the following: Extra Clinical Care of the LBW baby (breastfeeding/danger signs) Extra support for Feeding Extra support for warmth Vitamin K administration. Human resources In hospital: Enough physicians and nurses addressed to newborn care exclusively In the community: One trained TBA/CHW/health provider/physician/nurse per delivery to achieve good outcomes even if are facing up a multiple delivery. TBA´s/CHW/health provider should seek for help in these case if possible Surveillance System locally to address Fetal and Neonatal Mortality based on BABIES Matrix (birth weight and age at death boxes for intervention and evaluation system) (1). Strengthening training, monitoring and supervision of TBA’s, midwives and general practitioners about LBW babies accurate management. -Guarantee neonatologist/pediatricians/physicia ns/ nurses training for healthy and ill LBW babies More pediatrics and neonatology specialists. Other requirements Basic equipment plus: Method to identify LBW baby (baby balance scale, color-coded tape to measure foot, chest, mid-arm or head circumference or/and assessment of gestational age) Feeding tubes Oxygen tubes Head oxygen box IV solution sets Thermometer. Method to keep baby warmth (kangaroo care, overhead radiant heater, hot cots or incubator) Compressed air source (if possible) Oxygen blender to mix oxygen and compressed air Pulse oximeter and oximeter probe (if possible) Re-closable food-grade plastic bags (1-gallon size) or plastic wrap. Emergency Newborn Care Package Drugs Oxygen 10% dextrose for intravenous use Injection cephalosporin such as cefotaxime, depending on local policy for treatment of neonatal sepsis Vitamin K injection (1mg) Epinephrine 1:10,000 (0.1 mg/mL) — 3-mL or 10-mL ampules Isotonic crystalloid (normal saline or Ringer’s lactate) for volume expansion — 100 or 250 mL Naloxone hydrochloride 0.4 mg/mL — 1-mL ampules, or 1.0 mg/mL — 2-mL ampules -Political commitment. -Supervision and monitoring processes with weekly evaluations of sets of indicators. -Dissemination plans for emergency newborn care guidelines and protocols. Establish a Perinatal Epidemiology Surveillance System locally to address Fetal and Neonatal Mortality based on BABIES Matrix (birth weight and age at death boxes for intervention and MASTER PLAN: MATERNAL, NEONATAL AND REPRODUCTIVE HEALTH GROUP Normal saline for flushes Anticonvulsants (i.e. phenobarbital) depending on local policy Vasoactive drugs (dopamine) Surfactant factor Indometacine/ibuprofen for PDA Tetanus antitoxin Procedures After basic procedures: Identification of the neonatal danger signs Provide quality services for the sick newborn Treat efficiently severe neonatal infection Treat neonatal tetanus Manage neonatal asphyxia Provide jaundice treatment Provide family centered care for babies with birth defects Provide adequate severe bleeding treatment Human resources In hospital: Enough physicians and nurses addressed to newborn care exclusively In the community: TBA’s/CHW’s/health providers and mothers trained in the identification of neonatal danger signs. evaluation system) (1). Strengthening training, monitoring and supervision of TBAs, midwives and general practitioners about neonatal danger signs identification. Guarantee neonatologist/pediatricians/physicia ns/ nurses training More pediatrics and neonatology specialists. Appropriate infrastructure for medication storage and distribution Keep drug availability Installation and accreditation of blood banks to ensure the supply of safe blood. Legal advocacy Reorganize human resources infrastructure by skills To develop health resources education systems (i.e. Pediatrics/Neonatology specialization programs at regional hospitals) Other requirements Drip IV sets/Feeding tubes Oxygen tubes/head oxygen box/nasal CPAP/neonatal mechanical ventilators Stetoscope Method to keep baby warmth (overhead radiant heater beds, hot cots or incubators) Laryngoscope with straight blades, -No. 0 (preterm) -No. 1 (term) Endotracheal tubes, 2.5-, 3.0-, 3.5-, 4.0-mm internal diameter (ID) Blood sugar sticks for detecting low blood sugar Bilirubinometer for “bedside” measurement of bilirubin Sterilizer to clean containers for expressed breastmilk. Umbilical vessel catheterization supplies Blood giving sets, ideally with micro-dropper system Blood transfusion sets Cardiac monitor and electrodes or pulse oximeter if possible MASTER PLAN: MATERNAL, NEONATAL AND REPRODUCTIVE HEALTH GROUP 3.3 Reproductive health and family planning Effective Practices (EP) or Package of EPs Implement quality family planning services for adolescents Implementation Process Sustainability Implement exclusive services for adolescents or reserve periods of time in RH facilities for adolescents when exclusive services are not feasible. Political will is very important. Although there is consensus on the importance of the issue, it is not a high priority for decision makers and managers (e.g., politically sensitive topic, adolescents not seen as an important priority group). Train personnel to attend adolescents including counseling and service provision. Information dissemination and community participation. Continuous advocacy. Ensure access to counseling and services for at least six contraceptive methods in health posts Availability of skilled personnel in primary and secondary health services. Continuous training. Ensure availability of methods. Advocacy for maintaining availability of controversial methods (i.e., emergency contraception, vasectomy). A system of continuous training is crucial for sustainability. Promotion of community participation through education is critical. A procurement and delivery system is critical for maintaining the availability of commodities (DAIA). Training of providers in counseling and service provision. Implementation of a continuous supervision system. Information dissemination to the community. Internal advocacy in the system. Information dissemination on the availability of the method. Ensure access to vasectomy in hospitals and health centers Training of providers on non scalpel technique (gynecologists, urologists and general practitioners) Training health providers on promotion of the method and counseling. Continuous training. Appropriate instruments should be purchased and delivered to hospitals and health posts. Continuous monitoring and supervision. Unbiased information dissemination. Increase access in primary health care. Post-partum and post-abortion contraceptive counseling and services Trained personnel already exist. Educational materials. Implement counseling in antenatal care. Training of providers, provision of supplies. Continuous monitoring. Intensive information dissemination. MASTER PLAN: MATERNAL, NEONATAL AND REPRODUCTIVE HEALTH GROUP 3.4 Implementation and timing of effective practices Discussions were held with the working group and country representatives in order to help define the core set of MNRH interventions presented in the previous section. As part of this exercise, we requested the country representatives to prioritize and select interventions that may be more relevant for their particular context, and to identify specific factors related to implementation of interventions and their sustainability. Results from the feedback of three countries are presented in Appendix 2. They all indicate that, based on a core set of interventions, countries can find themselves in a good position to identify areas of opportunity to implement interventions within their specific contexts. Although the implementation of a given intervention should take into account its specific characteristics, there are several guidelines common to the implementation of EPs in the area of maternal, neonatal and reproductive health. This Master Plan is for a first phase of five years, so this time-span should be taken into consideration for the implementation and evaluation of interventions. Application of the interventions proposed in this area requires personnel skilled in the treatment of different maternal and neonatal complications, as well as in counseling and administration of family planning methods. Given the limited capacity currently existing in the countries of the region, training activities constitute one of the first activities in the sequence of implementation of interventions. Some of the interventions will be partially or completely performed by the same personnel. Therefore, training activities usually will positive influence several interventions, especially the maternal and neonatal intervention packages which are based heavily on the training of medical personnel, midwives and TBAs, and lay people in the community. It is also critical to train not only physicians and nurses but to train all the personnel, mainly those in charge of the poorest communities. Training should be essentially practical and should be followed by continuous monitoring and supervision A crucial step in the implementation of interventions will be the country-specific definition of implementation sites. Focalization of interventions is an important requisite for their success and must consider the general guidelines on target populations as described in this Master Plan. Interventions should be mainly geared toward the community and primary health care levels, emphasizing activities among poor and indigenous populations. Expansion to less vulnerable urban communities should be considered after the programs are fully implemented in the poorest areas. Despite of the fact that interventions proposed have demonstrated to be effective in several settings, it is highly recommendable to initiate the activities undertaking operations research in some locations. Operations research will determine which are the interventions really adequate for the country and will allow refining the intervention or package of interventions that will be scaled up thereafter. The implementation of interventions should also carefully consider the evaluation component. A finding from the Situational Analysis in maternal, neonatal and reproductive health in Mesoamerica was the limited information available on the impact of interventions, and by no means should we miss the opportunity to rigorously evaluate the interventions proposed in this Master Plan. Thus impact evaluation design also constitutes one of the first major steps in the implementation process. Two additional aspects should be considered in the early phases of implementation. First, the interventions should build upon existing structures in the region. One example is to take advantage of the presence and structure of international organizations like the Pan American Health Organization to achieve an effective implementation. Another example is to build upon existing health or social programs, which may already have actions related to maternal, neonatal and reproductive health. This may be the case for countries like Guatemala, Honduras or Mexico, MASTER PLAN: MATERNAL, NEONATAL AND REPRODUCTIVE HEALTH GROUP where the existence of nationwide social programs with a health component may constitute a good platform for the implementation of evaluations. The final aspect to be considered in this part of the implementation and evaluation design process is to clearly define a governance mechanism which allows the coordination of actions between and among countries. Strong coordination between countries may give a regional perspective to the interventions, generating economies of scale and a more rational use of resources. Therefore it is important to think about a regional coordination mechanism, perhaps in the form of a regional technical advisory group. 3.5 Rationale for effective practices The main problem identified in the Theory of Change was that while all national governments in the region have recognized the great importance of improving the quality of reproductive health care and have designed policies and programs to reduce maternal and neonatal mortality and to improve reproductive health services with an emphasis on family planning, there is a lack of effective implementation of programs and interventions. This is due mainly to managerial deficiencies within the systems of service and resource provision which fail to make interventions fully accessible to the whole population. We believe the implementation of these particular interventions have the most potential to solve the problem stated above via an analysis of the different reasons that often lead to an unsuccessful implementation: a) While constituting a regional strategy, at the same time the EPs will constitute a public good that may generate economies of scale for all countries. This will help address the lack of funding in the region that has limited the implementation of interventions thus far. b) Given the limited resources in the region, the packages of practices and interventions presented yield great impact for the least amount of money. c) Adapting high level health system-focused interventions to community and primary-level strategies was an important consideration in the exploration and selection of intervention packages in MNRH which tend to be clinical in nature. d) A capacity building component is considered a crucial part of the implementation process of these interventions. This will also increase the number of competent and skilled personnel, the lack of which has been another reason for poor implementation of interventions. e) Issues of sustainability of each intervention have been considered in its selection and implementation. This may also reduce the effect of the high staff turnover existing in Mesoamerican countries, which adversely affects the successful implementation of interventions. f) The implementation of effective family planning interventions is crucial for MNRH because, as stated in the last High-Level Meeting on Maternal Health -- Millennium Development Goal 5 (MDG5), to prioritize family planning, is one of the most costeffective development investments because “ensuring access to modern contraception can prevent up to 40 per cent of maternal deaths.” The interventions proposed in this Master Plan have been selected after an extensive literature review, in which the effectiveness and when available, the costs, of these practices have been documented. In this sense, all the interventions proposed have sound evidence of their effectiveness, mainly in developing countries. They also take advantage of the windows of opportunity for reduction of maternal and neonatal mortality (i.e., the period right before and after birth), and of the windows of opportunity for family planning promotion (i.e., the period after abortion or birth). The targeting of these interventions to the most underserved segments of the population (the poor and indigenous groups) also increases their potential impact. MASTER PLAN: MATERNAL, NEONATAL AND REPRODUCTIVE HEALTH GROUP 4. INTEGRATION Since packages of interventions are more cost-effective than any single action, and given the opportunity to join forces with other program areas based on community and primary care-level platforms, we have identified several potential areas of integration. 4.1 Integration within the maternal, neonatal and reproductive health pillar A number of interventions in MNRH have impact on other indicators within this focus area. A clear example is that increasing family planning availability and provision may not only affect fertility indicators, but may also reduce maternal mortality rates through the prevention of unwanted pregnancies. It has been proposed that achieving wide accessibility to family planning methods may reduce maternal mortality by up to 40% (UNFPA 2009). In the same way, interventions directed at improving the quality of obstetric care due to infections, hypertensive disorders or abortions contribute to the overall reduction of maternal mortality. Likewise, for practical reasons many intervention packages addressing maternal mortality include actions geared toward reducing neonatal mortality. Therefore, all of the practices proposed for this focus area effectively integrate packages that could in turn, be directed to the poorest segments of population. Finally, increased access and utilization of maternal and reproductive health services will probably increase the access and utilization of procedures to detect or prevent diseases, such as cervical cancer, breast cancer, STIs, and even men would have access to screening for prostate cancer and chronic diseases. 4.2 Integration across the vaccines, nutrition, and vectors pillars Nutrition Group. The integration of MNRH interventions with nutrition activities should be carefully examined to avoid duplication and create positive synergies. Breastfeeding is an excellent example of an intervention that is also addressed within the nutrition group, as its impact on neonatal and child health is well-documented. Among the effective practices that could benefit both groups are the provision and availability of contraceptives, as well as pre and postnatal household visits by health workers. The nutrition group can also benefit MNRH with norms and guidelines on food and other nutrients supplementation during pregnancy to prevent nutritional diseases such as anemia Vaccines Group. The MNRH group shares with the vaccine group its interest in reducing child mortality, which includes our group’s health focus of neonatal mortality. While our group is focusing on neonatal emergency care and community preparedness to prevent neonatal mortality, vaccination also plays an important role in reducing newborn deaths. Synergies between both groups can also be identified in the improvement of birth records, which may enhance neonatal care and the implementation of vaccination campaigns. Wide access to vaccine against rubella should be ensured and clear guidelines on its use by women should be disseminated to all services attending women in reproductive age. Vectors Group. Education during antenatal care should include basic measures about prevention of malaria and dengue, two prevalent infections in some areas of our region. The vectors group should collaborate with the MNRH group in devising practical measures and educational materials to reduce the spread of the infections during pregnancy and prevent child infections. MASTER PLAN: MATERNAL, NEONATAL AND REPRODUCTIVE HEALTH GROUP 5. HUMAN AND SYSTEMS CAPACITY BUILDING 5.1 Maternal health Inputs Required Capacity Components of Basic Emergency Obstetric Care (EmOC) Weak. Policies and policies to strengthen capacity exists but systems do not provide enough resources for adequate training in EmOC. Implementation of programs is insufficient and the problem is aggravated by the rapid turn over of personnel. Managerial systems are unable to retain trained personnel working in rural areas Blood banks/safe blood supply Weak Availability of medications Weak Appropriate infrastructure Training of primary health facility personnel Training of community health personnel Coordination processes between community and health facility Political will Weak. However, there is an important variability by country in the existing infrastructure for delivery attendance Weak Weak Weak Medium 5.2 Neonatal health Inputs Required Training of primary health facility personnel Training of community health personnel Coordination between community and health facilities Availability of medications LBW warm chain equipment Material and human resources equipped NICU’s Implementation and monitoring evaluation Capacity Weak. The capacity exists but the systems do not provide resources for adequate training. Weak. The capacity exists but the systems do not provide resources for adequate training. Very weak. Facilities are often too overcrowded to receive new high risk mothers/babies. Cases from the community are often stigmatized as worst outcomes cases, thus TBAs don’t seek help. Weak. Basic drugs are available at community level but specialized drugs for emergency newborn care such as surfactant factor are expensive and in some places not longer available; even in more specialized facilities. Weak. Incubators and heat radiation beds are not available at community level. Other kind of methods should be implemented at that level. Availability in facilities is limited. Very weak. Not enough beds for all sick babies. Concentration of NICU’s, pediatricians and neonatologist at metropolitan areas. Very weak. Managers are not used to using data for decisions. No well-functioning perinatal surveillance systems in the region. Heterogenity of resources distribution is evident, there are countries with stronger material and human capacities at least in larger cities. Disparity seems to be a great conflict. MASTER PLAN: MATERNAL, NEONATAL AND REPRODUCTIVE HEALTH GROUP 5.3 Reproductive health and family planning Inputs Required Training of providers and managers for improving service delivery Training social workers to train the community for improving community participation Implementation of monitoring and evaluation systems Improvement of managerial systems Capacity Weak. The capacity exists but the systems do not provide resources for adequate training. Weak. Some work has been initiated in some countries but the capacity for training the community is very weak. Very weak. Managers are not used to using data for decisions. Weak. People are not well trained and there is excessive personnel turnover. 5.4 Needs As previously described, there are huge material resource and human resource needs in the region. While there is no doubt that every country has economic restrictions which severely limit health budgets, it is equally important to strengthen political commitment to allocate more resources to health sector, especially for women's health and family planning. Family planning programs in particular historically have been funded in large part through international assistance — and when this financial assistance is reduced or eliminated, governments have not been able to respond adequately to the reality of shrinking resources. This situation may also be influenced by the activities of conservative groups who regularly take action against family planning. With the advent of AIDS as an important public health problem in recent years, the flow of funds from international agencies has become polarized towards AIDS prevention and treatment programs. For example, the Global Fund to Fight AIDS, Malaria and Tuberculosis is an important source of funding for countries in the region, but the largest proportion of the organization’s funds goes to Africa. Furthermore, these funds do not contribute to the improvement of sexual and reproductive health care. Qualified and properly trained service providers and managers are greatly needed throughout the region, with the situation being far more serious in rural areas and indigenous communities. While countries have the potential to meet demand for health provider training, the programs that are implemented are insufficient for the ever- increasing demand, which is even more important in rural areas. The need for adequate training systems cannot be understated and is further aggravated by the lack of managerial capacity of systems that fail to get trained personnel to work in rural areas. Making decisions about training traditional birth attendants or otherwise incorporating them into the health system are also imperative. In terms of management, there is a lack of capacity and willingness to adopt continuous supervision, monitoring and evaluation policies and programs, such that an insufficient number of skilled health personnel neither maintain adequate levels of training nor remain working in rural areas, where needs are most pressing. Moreover, systems of monitoring the distribution of supplies are inadequate, leading to a lack of equipment and essential drugs in rural areas. In most of the countries in the region health systems have no mechanisms to encourage quality of care. Due to the lack of a culture of accountability there are few mechanisms to promote improvement in performance among staff not satisfactorily fulfilling their duties. MASTER PLAN: MATERNAL, NEONATAL AND REPRODUCTIVE HEALTH GROUP Last but not least, community participation is quite scarce despite being recognized as an important component of quality improvement. In recent years significant efforts have been made to increase and improve the quality of community involvement, but these attempts have largely been isolated efforts without potential for scaling up. In the area of family planning, there is still a great need for improvement in supply and distribution of contraceptives. Although the introduction of systems to ensure availability of contraceptive supplies (contraceptive security, or CS) in several countries has somewhat improved the situation, in reality there are still very few health centers offering an adequate range of methods (reversible and permanent methods, and at least six different methods). This lack of a sufficient variety of methods in health centers is one of the most important factors limiting access to services because put simply, it prevents a woman from obtaining her desired method. Besides being one of the fundamental sexual and reproductive rights of women, choice of method is a factor that positively influences quality of care. On the other hand, lack of free and informed choice of methods limits acceptance of methods in health facilities and also has a negative effect on the continuation of use and effectiveness. A number of studies have shown that when a woman receives the method she chooses freely, the chances of failure and early discontinuation of use is significantly reduced (Pariani et al 1991). Whether provided as part of labor and delivery or abortion services, obstetric care always carries a risk of complications requiring rapid transportation to a higher-level facility. The need for skilled personnel and the role of community involvement in the early detection of complications has been addressed already, but it is also crucial to have in place effective strategies means to transport patients before cases become irresolvable. Unfortunately, women die relatively frequently because they are not transported in a timely manner even when the problem has been diagnosed and transportation has been requested. Implementing comprehensive and efficient transportation services for these cases is urgently needed, as is the involvement of community members and various stakeholders, above all in rural areas. 5.5 Available resources This issue is quite complex: there is a significant shortage of resources, namely equipment and basic supplies, but the most important deficiency is the lack of qualified and adequately trained personnel, especially in rural areas. Several countries in the region have reasonable educational and training structures with university support. There are several high-level institutions renowned for their research and education activities MNRH, such as the Centro de Población de la Universidad de Costa Rica, or the Instituto Conmemorativo Gorgas in Panama, just to name a few. Universities graduate large numbers of health professionals (physicians, nurses, psychologists, etc.) every year who are well versed in theoretical knowledge, but unfortunately these professionals lack adequate practical proficiency. Most recently graduated physicians are able to unequivocally diagnose lupus erythematosus and other pathologies frequently seen in hospitals, but wouldn’t know or would at least be seriously challenged by an eclamptic patient, and would likely have difficulties resuscitating an asphyxiatic newborn. Although the lack of human resources is an important problem in and of itself, it is exacerbated by inadequate distribution. In-service health professional training is geared toward higher level professionals (i.e., physicians and nurses), who many times remain working in urban areas where there is already a reasonable amount of skilled personnel. Health systems are lacking in mechanisms to effectively incentivize health professionals to stay in small cities or rural areas, nor are there legal or administrative mechanisms to keep them working in the most underserved areas. It is fundamental to strengthen the training of support personnel, as well as monitoring and supervision mechanisms. Training should be understood as a continuous and integral process. MASTER PLAN: MATERNAL, NEONATAL AND REPRODUCTIVE HEALTH GROUP Training courses may not be adequate for professionals, especially support personnel, because sometimes they are taught by other professionals with limited teaching competence and technical knowledge. It is necessary to review the actual training processes, based on sporadic courses, to move to a more continuous in-service training through supervisors. Supervisors should also be properly trained to be able to train and provide support for their field staff. This implies the allocation of more resources to support supervisors to conduct training and supervision activities that can have a real impact on the quality of care. It is also necessary to strengthen the training of health administrators. Otherwise the implementation of interventions will be seriously affected due to the lack of achievement of program objectives and compliance with norms, lack of organization, and problems with maintaining physical and human resources in the areas where they are most needed. The administrators must also have some incentive to improve the quality of care, and not to limit the administrative tasks that they often face. This gap may not be difficult to resolve since countries and international agencies offer a variety of courses in health administration, but it is necessary to make serious efforts to improve the quality of administrators’ work. As highlighted in previous sections, the resources for transportation to higher-level facilities for resolution of emergency cases, especially obstetric cases, are quite limited. This is also the case for non-emergency cases, in which transportation or economic problems may affect access to medical care. Although availability of informational resources is increasing, program evaluation and control of supplies and stocks are limited. The lack of reliable information may affect the planning of activities, especially when decision makers are aware of the poor quality of data. This situation is not generalized in the entire region, since some countries such as Costa Rica have developed good information systems that allow the planning of activities based on national evidence. 6. FEASIBILITY All the interventions proposed have a relatively low cost because they are oriented towards primary health care and/or communities. The interventions proposed in this plan have been aligned with those of other organizations and foundations, specifically the Bill and Melinda Gates Foundation, which carried out a substantial amount of work in developing countries demonstrating the feasibility of proposed interventions. Despite some technical limitations, the necessary facilities and human resources for undertaking the interventions in most cases already exist in the countries. However, feasibility also relies on the political commitment of countries in the region. It is imperative to allocate resources for training personnel to provide basic needs and care, and to promote administrative measures to keep skilled personnel in the areas where the most vulnerable populations live. In addition, it is extremely important to have a minimum of equipment and basic supplies and medications for obstetric and neonatal care, as well as family planning. This plan offers several options of interventions in the area of MNRH and FP. The countries will have the opportunity to choose the ones they consider the most relevant for their specific situation, or even for specific sub-regions or municipalities within each country, given the costs and available budgets. In order to achieve sustainability after the Mesoamerican Health Initiative financial support ends, countries must exercise caution when designing the programs with the initial donor funding. Most of the proposed interventions require the implementation of strong training, supervision and evaluation components. The feasibility and sustainability of the interventions will heavily depend MASTER PLAN: MATERNAL, NEONATAL AND REPRODUCTIVE HEALTH GROUP on the proper use of the initial funds from this initiative in order to create sustainable mechanisms for training and administration that ensure the availability of equipment, medications and family planning methods. The importance of the capacity building element to the implementation and sustainability of interventions cannot be understated. The implementation of interventions to increase access to and quality of family planning services is fundamental for the feasibility of the maternal and neonatal interventions. Providing access to high quality family planning and reducing the unmet need for family planning may consequently reduce the number of unwanted and high-risk pregnancies, reducing maternal mortality by an estimated 40% (UNFPA 2009). Technical assistance for at least the first five years is also a crucial element for the design, implementation, monitoring and evaluation of activities. A technical committee, working with the BMGF and with support from COMISCA, should ensure that the interventions implemented are those with the greatest potential impact on poor and rural populations, and that they remain focused on primary health care and the promotion of community participation. Operative research, or participatory action research, also plays a role in estimating the feasibility of the proposed interventions. Although we have included in this plan interventions with proven effectiveness in different settings, it is highly advisable to start the implementation of each intervention in each country with operative or participatory action research prior to scaling up the programs. This type of research allows for the refinement of methods and tailored implementation. Additionally, advance planning of the timeline and speed of expansion and scaling up of activities greatly helps budget planning, another key feasibility element. 6.1 Barriers and challenges As stated in the Strategic Assessment, the key problem identified in the region relating to maternal, neonatal and reproductive health is the actual implementation of programs, standards and projects, despite usually being well written and approved by the necessary authorities. The countries of the region have very good reproductive health programs — i.e., up-to-date and scientifically sound — but in reality the level of implementation in most areas is much lower than planned. Furthermore, very few programs are thoroughly evaluated and some never even get beyond the planning stage. Besides the financial factor which is undeniably important, there are several other factors contributing to the lack of effective implementation in the region: Managerial deficiencies, including shortcomings in monitoring and supervision, resource management and equipment maintenance, among others. Managerial limitations are strongly linked to the political organization of the countries in the region. Political issues excessively influence health systems because policies are designed by whatever group is currently in charge, and as a result most managers at the central level as well as in the provinces lack autonomy. As a consequence, every time there is an election or even just the replacement of a minister there are changes in key personnel which threatens program continuity. Political changes may constitute a barrier to the implementation and sustainability of effective practices, and it is necessary to consider specific strategies to reduce the risks related to changes in government positions. This staff turnover has traditionally been a very important factor negatively influencing project implementation, as it is necessary to reinitiate negotiations to maintain even successful projects active. Lack of trained personnel which in some areas is a real problem, but in others only reflects problems in managerial systems unable to adequately distribute the available personnel. The concentration of skilled personnel in large urban areas in detriment to small cities or rural MASTER PLAN: MATERNAL, NEONATAL AND REPRODUCTIVE HEALTH GROUP areas is characteristic of the region. The need for a continuous training in this area has been identified as a very important factor to solve the problems of quality in family planning. Lack of effective commitment to maternal, neonatal and sexual and reproductive health. Despite the tremendous importance of this health area, financing for family planning is always very low because governments still do not effectively assume the commitment of providing contraception. Traditionally, contraceptive methods have been provided by international agencies and now that donors have halted contraceptive provision, governments have not completely covered the gap. A similar situation occurs with maternal health in rural areas where access to skilled birth attendance is very limited. Political and ideological opposition to family planning. Despite great advances in the recent years, family planning can still be a political and/or ideological problem in the region. Countries have included family planning in their health systems but access is still quite limited in most of them and the political forces against family planning are always alert and active. Abortion and emergency contraception are the prime examples of this barrier. Most countries of the region have very restrictive laws on abortion, including countries where abortion is prohibited in any circumstances. On the other hand, emergency contraception has been registered in all countries but several groups are advocating for its prohibition. COMISCA and other international bodies involved in the initiative should actively advocate for the maintenance of family planning programs and to ensure access to abortion in cases that almost all countries in the world accept: rape and severe health risk to the mother. Last but not least, the endemic lack of quality of health personnel and managerial systems reflects both the lack of commitment to quality and insufficient supervision. The concept of accountability is still only a concept in the region but systems have no mechanisms to ensure that norms or guidelines are properly used. This is one of the main challenges for carrying out training, which should not only be oriented towards technical issues but also should change the way health personnel treat women. This concept relates to respecting human rights, including sexual and reproductive rights. A general challenge that must be addressed in the implementation of interventions described in this Master Plan is the strengthening of health information systems which must follow from this initiative. The strategic assessment has identified severe limitations in information as it currently exists in the region. The availability of reliable information on the existence and performance of maternal, neonatal and reproductive health services will be of great help for the planning of specific interventions in each country. 6.2 Unintended consequences It is possible that the implementation of interventions, especially of family planning, may increase the demand for health services, which are sometimes already right at their capacity limit. Periodic control in family planning necessarily includes early detection and prevention of other diseases, e.g., detection or treatment of sexually transmitted infections or prostate cancer in the male, which may also increase the demand for services. The increase in demand may be especially important for the detection of cervical cancer through Pap smears which is a routine procedure for women consulting for or using family planning methods. Health services must be ready to respond to this additional demand, including the treatment of cancer in initial stages. Health education and promotion of community participation may also increase the demand for health care in all areas such as immunization, diabetes and hypertension screening, etc. The implementation of services for adolescents may also increase the demand for services other than SRH, which should be considered in the integral planning of health systems. MASTER PLAN: MATERNAL, NEONATAL AND REPRODUCTIVE HEALTH GROUP 6.3 Protecting other programs We consider the proposed interventions to have a very low potential to negatively influence other programs. However, it is important that different programs maintain good communication practices to avoid any possible negative interference of MNRH actions with other programs, and to avoid duplication of efforts and coordinate the use of resources. After all, good coordination among programs may benefit all of them. 7. NEWLY EMERGING ISSUES Political instability: Perhaps is not fair to include this issue in the section “Newly Emerging Issues” but it is a very important issue that should be always taken into consideration. For this reason it would be very important to reinforce the international commitments and agreements among the countries of the region. A big effort should be made to reinforce the influence of COMISCA in order to ensure the sustainability of programs, independently of changes of authorities in the countries. Epidemics and other health threats. The great increase in international mobility of populations increases the risk of transmission of infectious diseases including STIs. Political and ideological opposition to family planning. Despite great advances in recent years, family planning is still problematic in the region. All countries include family planning in their health systems but access remains very limited in some countries of the region and the political forces against family planning are always alert and active. Abortion and emergency contraception are the best examples. Most countries of the region have very restrictive laws on abortion, and there are even countries where abortion is prohibited under any circumstance. Emergency contraception has been registered in all the countries but several groups are advocating for its prohibition and have actually obtained transient prohibition of its delivery in the public sector. COMISCA and other international supporters of the initiative should actively advocate for the maintenance of family planning programs and to ensure access to abortion in cases that almost the entire world accepts: rape and severe health risk to the mother. There is a great imbalance between the funds allocated to AIDS programs and to reproductive health programs. Despite the fact that the epidemic in the region is quite concentrated, with a general prevalence of less than 1%, the programs for AIDS prevention and treatment have larger budgets compared to maternal, neonatal and family planning programs. It would not make sense to promote a decrease in funding for AIDS prevention, but it would be important to coordinate efforts and implement advocacy campaigns to reposition maternal and neonatal health and family planning as an important priority area, with the objective of increasing the funds available for the implementation of MNRH interventions. Natural disasters caused by global warming. While we can’t accurately predict the future, the changes in climate during the past few years most likely caused by global warming, will undoubtedly result in more frequent natural disasters such as floods, hurricanes and droughts. Responding to these disasters will be an extra burden on already limited national health budgets. Economic and financial crisis. We have already experienced the worst of the economic crisis but recovery is not yet complete. Furthermore, its impact on wealthy countries makes it quite likely that resources for international assistance will shrink. On the other hand, in reaction to the crisis the G-20 made a decision to make an important effort to maintain and even increase levels of assistance for the poorest countries. MASTER PLAN: MATERNAL, NEONATAL AND REPRODUCTIVE HEALTH GROUP 8. POLICY LANDSCAPE The countries of the region have made a strong commitment of improving health actions through the development of an integrated health program initially acting in four areas: nutrition, diseases transmitted by vectors, immunizations, and maternal, neonatal and reproductive health. The initiative has the explicit support of all the countries of the region and COMISCA is taking the lead in promoting its full implementation. The participation of COMISCA is especially important in those countries undergoing political instability that may interfere with the implementation of interventions in the context of the MHI. Support from other international organizations like PAHO may also provide a platform for the implementation and sustainability of interventions. Furthermore, all the countries of the region adopted the Millennium Declaration and committed to achieving the MDGs. However, in general, the countries of the Mesoamerican region have had slower progress than expected. In addition the global financial situation may compromise funding for programs to improve maternal health, the goal towards which there has been least progress so far. Since the mid-1990s, most developing countries have experienced a major reduction in donor funding for family planning on a per woman basis, despite the undeniable contribution of such programs to maternal and child health. On the other hand, the leaders of the G-20 have declared that the efforts to maintain official assistance for development will be intensified to protect at least the programs having impact on maternal and infant mortality in poor countries. The Mesoamerican health program recognizes the great importance of maternal and infant health and will give support to initiatives aimed at reducing maternal and neonatal mortality. All the countries of the region contributed towards the definition of the main needs that informed this Master Plan and are committed to increasing efforts to implement effective actions for improvement of maternal and neonatal health. Although Latin America is not a priority region for most major donors, the Bill and Melinda Gates Foundation, Carso and others have earmarked funds for implementation of some of the activities defined in this Master Plan, and will provide assistance to the region for better utilization of the available funds and in fundraising activities. MASTER PLAN: MATERNAL, NEONATAL AND REPRODUCTIVE HEALTH GROUP 9. INDICATORS FOR MONITORING AND EVALUATION MATERNAL HEALTH IMPACTS OUTCOMES OUTPUTS Basic Emergency Obstetric Care (EmOC) Reduction of maternal mortality Reduction in gap between income quintiles in the proportion of births attended by skilled personnel Indicator Definition Maternal Mortality ratio (Number of maternal deaths) / (100,00 live births) Ratio of births with EmOC in lowest and upper income quintiles of population Proportion of births with EmOC in lowest income quintile over proportion of births with EmOC in the upper income quintile Increase in the number of health centers/posts that offer basic EmOC Number of health centers and health posts that offer basic EmOC per 500,000 inhabitants (Number of health centers and health posts that offer basic EmOC / (Total number of health centers and health posts) *500,000 inhabitants Reduction in the number of women with obstetric complications who do not receive EmOC services Proportion of women with obstetric complications who do not receive EmOC services (Number of women with obstetric complications who do not receive EmOC services) / (Total number of woman who experience obstetric complications) * 100 Increase in the number of skilled personnel who can provide EmOC at the community and hospital levels Number of skilled personnel who can provide EmOC at the community and hospital levels (Number of skilled personnel who can provide EmOC at the community and hospital levels) / (Number of health personnel in the community and in the hospital) MASTER PLAN: MATERNAL, NEONATAL AND REPRODUCTIVE HEALTH GROUP Active management of the third stage of labor (AMTSL) to prevent postpartum hemorrhage OUTCOME OUTPUTS Definition Annual Number of maternal deaths from postpartum vaginal hemorrhage (%) (Number of maternal deaths from postpartum vaginal hemorrhage per year) / (Number of live births per year) *100,000 Reduction in the number of cases with severe vaginal hemorrhage Cases of moderate postpartum vaginal hemorrhage (>500 ml) (Number of cases of moderate and severe postpartum vaginal hemorrhage (>500 ml) per month) / (Number of vaginal deliveries per month) Increase in the number of deliveries with AMTSL Vaginal deliveries with AMTSL (Number of vaginal deliveries with AMTSL per month) / (Number of vaginal deliveries per month) Decrease in the number of cases of moderate and severe post-partum vaginal hemorrhage Percentage of vaginal deliveries with moderate an severe post-partum vaginal hemorrhage (Number of cases of moderate and severe post-partum vaginal hemorrhage) / (Number of vaginal deliveries in hospital with AMTS per month) Increase in the use of oxytocin or unijet Number of units of oxytocin or unijet used per month (Number of units of oxytocin or unijet used per month) / (Number of vaginal deliveries per month) Decrease in the application of blood transfusions in post-partum Number of post-partum blood transfusions per month (Number of blood transfusions per month) / (Number of vaginal deliveries in hospital per month) Increase in the number of personnel trained to provide AMTSL to prevent postpartum hemorrhage Skilled personnel who are trained to provide AMTSL (Number of skilled personnel who are trained to provide AMTSL) Reduction of maternal mortality due to postpartum hemorrhage IMPACTS Indicator MASTER PLAN: MATERNAL, NEONATAL AND REPRODUCTIVE HEALTH GROUP IMPACTS OUTCOMES Interventions to reduce maternal mortality from eclampsia Reduce maternal mortality due to eclampsia or pre-eclampsia Definition Maternal mortality ratio for eclampsia or pre-eclampsia (Number of maternal deaths caused by eclampsia per year) / (Number of live births per year) *100,000 Increase the number of cases of pre-eclampsia or eclampsia treated with the proposed intervention Cases of eclampsia that are treated (Number of cases of eclampsia that are treated according to proposed intervention) / (Number of cases of pre-eclampsia o eclampsia) Increase the number of cases of pre-eclampsia or eclampsia successfully transferred to higher-level institution (when required) Cases of eclampsia referred to higher-level institution (Number of cases of eclampsia referred to higher-level institution) / (Number of cases of pre-eclampsia o eclampsia) Improvement in the management of cases of preeclampsia or eclampsia OUTPUTS Indicator Increase in the number of personnel trained in the treatment of emergencies due to pre-eclampsia or eclampsia Ratio of discharges from severe pre-eclampsia or eclampsia to discharges from mild or moderate pre-eclampsia Personnel trained in the treatment of emergencies due to pre-eclampsia or eclampsia (Number of cases of severe pre-eclampsia or eclampsia) / (Number of cases of mild or moderate preeclampsia) Number of people trained in the treatment of emergencies due to pre-eclampsia or eclampsia MASTER PLAN: MATERNAL, NEONATAL AND REPRODUCTIVE HEALTH GROUP IMPACTS OUTCOMES OUTPUTS Interventions to reduce maternal mortality from postpartum infection Reduction of maternal deaths due to post-partum infection Indicator Definition Maternal mortality ratio for post-partum infection (Number of maternal deaths from post-partum infection per year) / (Number of live births per year) * 100,000 Increase in the number of emergencies from post-partum infections treated according to the proposed intervention Cases treated for postpartum infection (Number of cases treated for postpartum infection per month according to proposed intervention) / (Number of vaginal deliveries per month) Increased proportion of severe post-partum infections diagnosed and referred to higher-level institutions Cases of postpartum infection referred to higher-level institution (Number of cases of postpartum infection referred to higher-level institution per month) / (Number of vaginal deliveries per month) Increase the number of cases of post-partum infection treated at the community or primary level according to the proposed intervention Cases of postpartum infection treated initially in health centers or health posts (Number of cases of postpartum infection treated initially in health centers or health posts per month according to proposed intervention) / (Number of vaginal deliveries per month) Increase in personnel trained in the treatment of emergencies due to postpartum infections at the community and health facility level Personnel trained in the treatment of emergencies due to postpartum infection at the community and health facility level Number of persons trained in the treatment of emergencies from postpartum infection at the community and health facility level. MASTER PLAN: MATERNAL, NEONATAL AND REPRODUCTIVE HEALTH GROUP Best practices (interventions) to reduce maternal mortality from septic abortion IMPACTS OUTCOMES OUTPUTS Indicator Definition Reduction of maternal deaths due to abortion Maternal mortality ratio for abortion (Number of maternal deaths from abortion per year) / (Number of live births per year) * 100,000 Increase in the number of abortion emergencies treated according to intervention Septic abortion cases treated. (Number of cases treated for septic abortion per month according to proposed intervention) / (Total number of abortions per month) Septic abortion cases referred to higher-level institution (Number of septic abortion cases referred to higher-level institution) / (Total number of abortions) Cases of infection from septic abortion initially treated in basic health facilities or centers (Number of cases of infection from septic abortion initially treated in basic health facilities or centers) / (Total number of cases treated for septic abortion) Personnel trained in the treatment of abortion emergencies at the community and health facility level Number of persons trained in the treatment of abortion emergencies at the community and health facility level. Increase in the number of abortion emergencies referred to higher-level institution Increase in the number of cases of emergencies from abortion treated at the community or primary level according to the intervention Increase the personnel trained in the treatment of abortion emergencies at the community and health facility level MASTER PLAN: MATERNAL, NEONATAL AND REPRODUCTIVE HEALTH GROUP NEONATAL HEALTH *Due to the nature of the presentation of packages of neonatal health interventions, this set of indicators serves for all three bundled intervention packages (Essential Newborn Care, Extra Newborn Care for the LBW Baby and Emergency Newborn Care). They differ in the degree of severity of the health of the newborn but all share the same impact goals. Newborn essential care, LBW care and emergency care Indicators Reduction in intrapartum fetal mortality rate Intrapartum mortality rate (Babies born without heart beat and non sloughing skin with no succesful resuscitation after ten minutes)/(total births*) *1000 Decrease in neonatal& mortality rate Neonatal mortality rate (Number of babies born alive who die in the first 28 days of life)/(live births)*1000 Reduction in low birth weight neonatal& mortality rate Low birth weight neonatal mortality rate (Number of babies born alive who wheigthed less than 2500g at birth and die in the first 28 days of life)/(live births)*1000 Reduction in neonatal& mortality rate due to asphyxia perinatal, hypothermia, hypoglycemia, severe infectious complications or serious bleeding. Neonatal death rate for specific cause (perinatal asphyxia, hypothermia and complications, hypoglycemia, severe infection or serious bleeding. Definition (Number of babies born alive who die from a specific cause in the first 28 days of life)/(live births)*1000 IMPACTS (Stillbirths+Infant (first year)) deaths/ (total births*)/1000 As a global result, reduction in Fetal-infant mortality, infant mortality and under-5 mortality rates due to factors previously mentionated. Reduction of the gap between the proportion of babies with adequate EEENC at birth across income quintiles of population Fetal-Infant mortality (Deaths of infants under one year of age)/(live births)*1000 Infant mortality Under-5 mortality (Deaths of children under five years of age)/ the (number of population at risk during a certain period of time)*1000 Ratio of babies with EEENC at birth in lowest and upper income quintiles of population Proportion of babies with EEENC at birth in lowest income quintile over proportion of babies with EEENC at birth in the upper income quintile MASTER PLAN: MATERNAL, NEONATAL AND REPRODUCTIVE HEALTH GROUP OUTCOMES Decrease in perinatal asphyxia incidence Perinatal asphyxia incidence (New cases of perinatal asphyxia)/(live births)*100 Decrease in early neonatal sepsis incidence Early neonatal sepsis incidence (New cases of neonatal sepsis which occured among the three first days of life)/(live births)*100 Reduction in other specific early neonatal complications incidence Specific early neonatal complications incidence Improve mother/TBA´s/CHW´s/ health provider identification of pregnancy danger signs to refer high risk mother to a more specialized facility for delivery High risk pregnancies referred from community/primary care units to a more specialized facility for delivery Improve mother/TBA´s/CHW´s/ health provider identification of neonatal danger signs to refer high risk babies to a more specialized facility for treatment Reduce the ratio of babies with perinatal asphyxia with access to accurate resuscitation if needed (New cases of specific early neonatal complications which occured among the first seven days of life)/(live births)*100 Proportion of high risk pregnancies from community/primary care units referred to a more specialized facility for delivery High risk neonates referred from community/primary care units to a more specialized facility for treatment. Proportion of high risk neonates from community/primary care units referred to a more specialized facility for treatment Ratio of perinatal axphyxiate babies with accurate resuscitation (Number of babies with perinatal asphyxia)/(number of babies who receive neonatal resuscitation) Improve in the number of skilled newborn attendant at birth Skilled newborn attendant proportion (Number of skilled newborn attendants)/(Total of newborn attendants)*100 Increase in the number of women who breastfeed their baby in the first hour of life and mantain it during the first six months Mothers who breastfeed proportion (Number of mothers who breastfeed)/(Number of deliveries)*100 Increase in the number of baby friendly hospitals Friendly hospitals proportion (Number of friendly hospitals)/(Number of hospitals attending deliveries)*100 Increase in the number of babies who receive eye prophylaxis, clean and warm chain Eye prophylaxis, clean and warm chain proportion (Number of eye prophylaxis, clean and warm chain)/(live births)*100 OUTPUTS MASTER PLAN: MATERNAL, NEONATAL AND REPRODUCTIVE HEALTH GROUP REPRODUCTIVE HEALTH AND FAMILY PLANNING Implement quality family planning services for adolescents Indicators Number of new FP acceptors. Decreased number of pregnancies and deliveries in adolescents. IMPACTS Decreased number of STI in adolescents. Contraceptive prevalence in adolescents (surveys). Fertility rate in the 10-14 and 15-19 year old age brackets. Percentage of all deliveries occurring in women 10-19 years. Increased access and utilization of services. OUTCOMES Increased knowledge and use of contraceptive methods. Increased use of condoms for STI prevention. SRH services exclusive for adolescents in health centers. OUTPUTS Services offering FP and STI prevention for adolescents Number of adolescents registered in health centers. Number of adolescents requesting contraceptive methods and condoms for STI prevention. Number of services offering SRH services for adolescents at least twice a week. User satisfaction (surveys). Definition New acceptors of contraception by method per year who are adolescents (service statistics). Percentage of adolescents using contraception by methods (surveys). Percentage of total deliveries occurring in women 10-19 years old (maternity statistics, national register of deliveries). Number of adolescents registered in health centers. Number of adolescents requesting family planning and other sexual and reproductive health services (health services statistics). Number of adolescents receiving condoms from health services (health services statistics). Number of health centers offering services exclusively for adolescents (a facility exclusively for adolescents, dedicated space within the health center, or reserved periods of time). MASTER PLAN: MATERNAL, NEONATAL AND REPRODUCTIVE HEALTH GROUP Ensure access to counseling and services for at least six contraceptive methods in health centers and health posts Indicators Definition New acceptors by method per year. Number of new FP acceptors. IMPACTS Decrease in the number of unwanted pregnancies and abortions. Contraceptive prevalence (surveys). Fertility rates by age and TFR. Increase in the quality of FP services. OUTCOMES Increased in the number of people asking for contraception in FP services. Proportion of women using contraceptive methods (detailed by method). Average number of children that women would have during her entire reproductive life, if agespecific fertility rates are maintained. Health statistics, number of FP consultations. Number of consultations in FP. User satisfaction studies. Increase in the number of new acceptors and continuous users. User satisfaction, adherence to instructions and follow-up. Health statistics (number of new acceptors by method and number of FP consultations. More services offering at least six methods. OUTPUTS Increased access to contraceptive methods. Number of services offering at least six modern FP methods (counseling and services). Number of health posts and health centers offering at least six FP methods (administrative reports). More options of contraceptive methods. MASTER PLAN: MATERNAL, NEONATAL AND REPRODUCTIVE HEALTH GROUP Ensure access to vasectomy in hospitals and health centers Indicators Number of men undergoing vasectomy per year. IMPACTS Increased acceptance of the method. Failure rate of the method. Increased number of men undergoing vasectomy. Number of men requesting vasectomy reversal. Increased prevalence of use of the method (surveys). Increased access to and utilization of vasectomy. OUTCOMES Increased knowledge about the method and decrease of myths about it. Hospitals and health centers offering vasectomy as a contraceptive option. OUTPUTS Increased numbers of men requesting information about the method. Definition Number of men operated in hospitals or health centers (Official health services statistics). Failure rate (number of pregnancies after vasectomy per 100 procedures). Percentage of men who underwent vasectomy requesting and undergoing a surgery for vasectomy reversal (health services statistics). Prevalence of vasectomy (DHS). Men considering vasectomy. Number of men requesting vasectomy. Men utilizing vasectomy. Number of men undergoing vasectomy. Number of services (hospitals and health centers) effectively offering access to vasectomy. Number of hospitals offering the no scalpel technique vasectomy. Number of men requesting information on vasectomy. Number of hospitals and health centers offering vasectomy services (Official MOH statistics). Number of services offering the no scalpel technique. MASTER PLAN: MATERNAL, NEONATAL AND REPRODUCTIVE HEALTH GROUP Implement post-partum and postabortion contraceptive counseling and services in all hospitals attending deliveries and abortions IMPACTS OUTCOMES Increase in contraceptive use after delivery or abortion. Acceptance of contraceptive methods after delivery or abortion. Contribute to an increase in contraceptive prevalence. Contraceptive prevalence (surveys). Increase in the intergestational period. Intergestational period. Increased access to and utilization of contraceptive methods in the postpartum and post-abortion period. Increased knowledge and use of contraceptive methods. Increase in trained personnel who offer post-partum and post-abortion FP counseling and services. OUTPUTS Indicators Implementation of FP counseling and services in hospitals and health centers that attend deliveries and complications of abortion. Increased proportion of women receiving contraceptive counseling during the post-partum and postabortion period. Increased proportion of women having a delivery or an abortion who accept and receive a contraceptive method before discharge from the hospital. Number of hospitals and health centers offering FP counseling and services after delivery and abortion. User acceptance and satisfaction (studies, surveys). Definition Percentage of the total deliveries and abortions: (hospital statistics). Proportion of women using contraceptive methods (detailed by method). Time elapsed between the delivery and previous delivery or abortion (statistics from clinical records). Proportion of women receiving contraceptive counseling after a delivery or an abortion per year. Proportion of women who accept and receive a contraceptive method before discharge from the hospital (statistics of the hospital). Number of hospitals that attend deliveries and abortions that effectively offer post-partum and post-abortion FP counseling and services. MASTER PLAN: MATERNAL, NEONATAL AND REPRODUCTIVE HEALTH GROUP 10. IN-TEXT REFERENCES A fast track solution for reducing unintended pregnancies in the US: increase federal support for life-long provider education and training in reproductive health. Editorial. Contraception 2009; 80: 231-233. Adam T, Lim SS, Mehta S, Bhutta ZA, Fogstad H, Mathai M, Zupan J, Darmstadt GL. Cost effectiveness analysis of strategies for maternal and neonatal health in developing countries. BMJ (2005); 331:1107. Armstrong N and Donaldson C. The economics of sexual health (2005). Family Planning Association (UK). Cost effectiveness results for Maternal and Neonatal Health. WHO-CHOICE. Darmstadt GL, Bhutta ZA,Cousens S, Adam T, Walke N, Bernis L. Evidence-based, costeffective interventions: how many newborn babies can we save? Lancet (2005); 365: pp. 977–88. Foster DG, Rostovtseva DP, Brindis CD, Biggs MA, Hulett D, Darney PD. Cost savings from the provision of specific methods of contraception in a publicly funded program. American Journal of Public Health (2009) Vol. 99(3) pp. 446-51. Graham WJ, Cairns J, Bhattacharya S, Bullough CHW, Quayyum Z, Rogo K. Maternal and Perinatal Conditions. 2006. Disease Control Priorities in Developing Countries (2nd Edition) Eds. Jamison DT et al, 499-530. New York: Oxford University Press. Lawn JE, Zupan J, Begkoyian G, Knippenberg R. Newborn Survival. 2006. Disease Control Priorities in Developing Countries (2nd Edition) Eds. Jamison DT et al, 531-550. New York: Oxford University Press. Levine R, Langer A, Birdsall N, Matheny G, Wright M, Bayer A. Contraception. 2006. Disease Control Priorities in Developing Countries (2nd Edition) Eds. Jamison DT et al, 1075-1090. New York: Oxford University Press. Lule E, Rosen JE, Singh S, Knowles JC, Behrman JR. Adolescent Health Programs. 2006. Disease Control Priorities in Developing Countries (2nd Edition) Eds. Jamison DT et al, 11091126. New York: Oxford University Press. Mavranezouli I. Health economics of contraception. Best Practice & Research Clinical Obstetrics and Gynaecology (2009) Vol. 23, No. 2, 187-198. McGuire A and Hughes D. The cost-effectiveness of family planning service provision. Journal of Public Health Medicine (1995) Vol. 18 (2): pp. 189-196. Pariani S, Heer DM, Van Arsdol MD. Does choice make a difference to contraceptive use? Evidence from east Java. Jr Stud Fam Plann. 1991:Nov-Dec;22(6):384-90. Trussell J. The cost of unintended pregnancy in the United States. Contraception (2007) Vol. 75, pp. 168-170. Trussell J, Leveque JA, Koenig JD, et al. The economic value of contraception: a comparison of 15 methods. Am J Public Health (1995) 85: pp. 494–503 UNFPA. Proceedings of the High level meeting on maternal health - Millennium Development Goal 5 (MDG5). Addis Abbaba, 2009. MASTER PLAN: MATERNAL, NEONATAL AND REPRODUCTIVE HEALTH GROUP MASTER PLAN: MATERNAL, NEONATAL AND REPRODUCTIVE HEALTH GROUP