Staff Injury
advertisement

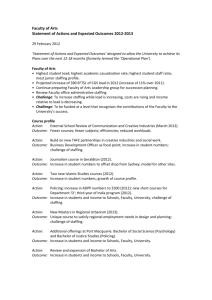
STAFFING EFFECTIVENESS PLAN FOR CARDIOPULMONARY DEPARTMENT MANUAL SECTION Respiratory Administration POLICY CODE and NUMBER PURPOSE: The purpose of this policy is to provide an approach and guideline that utilizes screening indicators for the staffing effectiveness of the Cardiopulmonary Department, and to provide for adjusting staffing based on census and workloads. POLICY: The department of Cardiopulmonary shall be staffed, with a sufficient number of qualified personnel, to provide the range of services described within the scope and function. Staffing will be determined using a budgeted standard which is based on historical data, patient acuity, and census. Cardiopulmonary services will be provided 24 hours a day, seven days a week. The Cardiopulmonary Department actively maintains on-going processes to assure that only qualified and competent staff provides care or support services. EMPLOYMENT: The department of Cardiopulmonary shall employ qualified/competent respiratory care practitioners who have established themselves in one of the following employment categories: Registered Respiratory Therapist (RRT) – Graduate of an AMA approved respiratory therapy program. Registered by the National Board for Respiratory Care. Current BCLS certification, ACLS certification preferred. Completion of identified competencies and equipment skills. Certified Respiratory Technician (CRT) – Graduate of an AMA approved respiratory therapy technician program and certified by the National Board for Respiratory Care. Current BCLS certification, ACLS certification preferred. Completion of identified competencies and equipment skills. Each employee performs his duties according to a criteria based job description that reflects patient and population, specific needs, and defines re-qualifications and competency standards. A performance appraisal is conducted for each employee upon completion of probation period and annually thereafter. Clinicians are also required to complete a competency/proficiency annually in the selected area to assure that on-going competency requirements are met. STAFFING EFFECTIVENESS PLAN FOR CARDIOPULMONARY DEPARTMENT STAFFING PLAN: I. All staffing will be evaluated on a daily basis and adjusted accordingly. Staffing is based on patient census, acuity, and the amount of time required completing the procedures requested by the ordering physician. Subsequently, staffing is flexed based on procedural demands of each shift. There are 1.5 hours per patient budgeted to cover 24 hours per day, seven days per week (which equates from the number of worked hours/census). Number of Hours Worked 72 68 64 56 Hospital Patient Census 45 40 37 32 Staffing Needs/24 hours 6 5.6 5.3 4.6 a. Total therapy units reflect all therapy given per shift, with ultimate goal between 44 to 48 units of therapy per shift per therapist average. b. Increased staffing needs are met through use of prn staff and/or overtime. Decreasing staffing needs are met by utilizing paid time off (PTO), vacation time, and /or request of that therapist at the discretion of the department director. Skill level of providers is as follows, total employees 23, 10-FTE (~12.8 FTE), 13-PRN, with 11-RRT and 12-CRTT. A per-diem pool of employees will be maintained in order to allow for an upswing in the volume of therapy to be rendered. It will be at the discretion of the department director to request additional staffing levels based on volume data. II. Department Director will be scheduled Monday – Friday, and will be on call if needed. III. Each shift will be allowed a number of staff positions with varying skill mixes, working under the direct supervision of the director. The director has the authority to adjust staffing levels as deemed appropriate. If staff needs to be added, per-diem pool staff should be first utilized, and overtime secondarily. IV. Patient Volume Adjustments – depending on the volume of the patient population, it will be necessary to adjust staffing levels. Acuity level assessment will be the responsibility of the senior staff member. V. Staff coverage – Day shift - 2/3 RCPs, Night shift - 2/3 RCPs VI. Respiratory Care Staffing Variance Report will be completed daily with written weekly report forwarded to COO or designee. This information will be utilized to evaluate staffing on a budgetary/operational level. STAFFING EFFECTIVENESS PLAN FOR CARDIOPULMONARY DEPARTMENT STAFFING EFFECTIVENESS: I. Monitoring and evaluation of the effectiveness of patient care and support services are maintained on an on-going basis through a well-defined program for improving organizational performance. II. The program emphasizes the analysis of the appropriateness of care, evaluation of problems and concerns identified, as well as opportunities for improvement of services and patient care. These activities provide mechanism to effectively assure a comparable level of care for all patients. III. This plan for provision of patient care is reviewed and revised as necessary. The following elements are taken into consideration in conducting the annual review: The facility’s mission; Strategic and budget planning process; Findings from performance improvement, risk management, utilization review and other evaluation activities; Changes in patient care needs; Patient requirements and implications for staffing; Relevant information from staffing variance reports; Adequacy of staff recruitment and development activities; IV. The staffing indicators are approved and trended data will be reported to the Performance Improvement Committee, Quality Council, Medical Executive Committee and Governing Board. V. Clinincal Indicators for the Cardiopulmonary Department include but are not limited to respiratory treatment rate and ventilator pneumonia rate. As indicated we will participate in organization wide clinincal indicators when applicable. VI. Human Resource indicators for the Cardiopulmonary Department include but are not limited to employee/staff injuries rate The COO, DQM and Cardiopulmonary Director and/or designees collaborate with various senior leadership, medical staff and department representatives to plan, implement and evaluate performance improvement activities and report the results of these activities, including performance improvement team outcomes, cost/quality and human resource outcomes to the Performance Improvement Committee. Cardiopulmonary personnel are encouraged to participate in performance improvement identification, implementation and evaluation. Feedback is provided through various means including but not limited to employee meetings, individual recognition and routine postings. The Cardiopulmonary Director and/or designees communicate with other departmental representatives on a regular basis to plan, implement and evaluate activities that support the cardiopulmonary care delivery services. STAFFING EFFECTIVENESS PLAN FOR CARDIOPULMONARY DEPARTMENT INDICATORS FOR 2003 Indicators Selection Rationale Formula Goal Monitoring Frequency Related to the Six C’s Monthly C3, C5, C6 Monthly C1, C3, C6 Monthly C2, C3, C6 Monthly C2, C3, C6 HR Respiratory Hours per Patient Day (RT-HPPD) Measure overall productivity of care providers. HPPD was in 2002 is 1.64. Skill-Mix 100% of direct care providers. Total worked hours in day Total patients in day 1.64 (2002) YTD average 1.46 (2003) HR Staff Injury C/S Vent Pneumonia Rate To measure the number of staff injuries compared with plan and provision of care. To measure patients on ventilator with newly diagnosed nosocomial pneumonia Total Departmental Staff Injury Number of patients on MV with new nosocomial pneumonia X 1000 Total vent days <12 YTD 3.00 YTD Rate C/S Delivered Treatment Rate To measure the number of respiratory treatments compared to overall treatments Number of treatments delivered X 100 Number of treatments 99.8% (2002) YTD Rate References: JC-HAS: OTHER: Original Date Review/Revision Date Supersedes all Previous 07/17/97 04/28/03 Approved: _____________________ Date 06/11/03